Percutaneous Pedicle Screw Fixation and Fusion for Trauma
David H. Wei
Kelley Banagan
Steven C. Ludwig
DEFINITION
The advancement of minimally invasive techniques in spinal surgery, specifically percutaneous pedicle screw fixation, has reduced approach-related morbidity.
These techniques have been shown to be advantageous in patients with spine tumors and deformities and have become increasingly applicable for managing complex spinal trauma, including thoracolumbar trauma.
The goals of treatment of traumatic spine fracture remain the same whether an open or percutaneous approach is used: stabilize the spine to facilitate rehabilitation; enhance neurologic recovery; and prevent neurologic deterioration, delayed pain, and postoperative deformity.
ANATOMY
Traditional open posterior surgical approaches can result in extensive soft tissue damage, muscle denervation, and ischemia, with subsequent paraspinal muscular atrophy and decreased strength.
In addition, open approaches can lead to increased blood loss, protracted postoperative pain, and higher infection rates.
In contrast, minimally invasive procedures involve less extensile and thus less disruptive dissection. Important relevant anatomy and anatomic landmarks are discussed in following text.
PATHOGENESIS
The most common mechanisms of traumatic injury to the thoracolumbar spine are motor vehicle accidents, falls from height, and domestic violence.
When traumatic injury results in spinal cord injury, the loss of neurologic function is attributed to both a primary and a secondary injury process.
The primary injury is sustained when the spinal cord and column absorb energy from the trauma, with resultant spinal deformation and persistent postinjury compression.
A cascade of secondary effects ensue, including vascular changes, cell membrane lipid peroxidation, free radical formation, electrolyte shifts, neurotransmitter accumulation, and inflammation. This cascade results in expansion of the initial area of injury in a rostrocaudal fashion, leading to further gray matter loss and white matter degeneration.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Preoperative advanced imaging is a critical tool for understanding the patient’s pathoanatomy and preoperative planning.
Commonly, computed tomography (CT) and magnetic resonance imaging (MRI) scans are obtained to assess bony and spinal cord injury, respectively.
Additionally, MRI can be used to assess the competency of the posterior ligamentous structures, which can assist in determining the overall stability of the injury.
Using preoperative images as a guide, the fluoroscope can then be precisely rotated in the axial plane to the degree of medial angulation seen on axial view CT or MRI scans at the respective level.
NONOPERATIVE MANAGEMENT
Thoracolumbar trauma has historically been managed with conservative treatment in the form of traction, casting, and bed rest.
However, nonoperative treatment can be complicated by the morbidities associated with prolonged immobilization.
With the development of minimally invasive spine surgery (MISS), we have learned that decreased surgical time, decreased blood loss, and a reduction in postoperative surgical site infection can decrease surgical morbidity in patients with multiple traumatic injuries.3
The application of these principles in the setting of spine trauma offers the patient earlier mobilization and rehabilitation.
SURGICAL MANAGEMENT
Indications for minimally invasive percutaneous pedicle screw fixation continue to be established.
Multiple variables are important when considering surgical intervention, including fracture morphology, neurologic involvement, and the status of the posterior ligamentous complex.
The Thoracolumbar Injury Classification and Severity Score can be used to help guide the surgeon’s decision-making process for operative versus nonoperative fracture management.
Once the decision for surgical intervention has been made, the relative indications for minimally invasive techniques include unstable thoracolumbar burst fractures, stableburst fractures for which conservative treatment has failed, flexion-distraction injuries, extension-distraction injuries, unstable sacral fractures requiring lumbopelvic stabilization, and fracture-dislocations.
Preoperative Planning
Before the surgical procedure, a thorough understanding of the patient’s surgical anatomy is essential because traditional
visual and tactile landmarks for pedicular fixation are not present. Thus, without optimal preoperative fluoroscopic visualization, the surgeon must keep in mind the potential risk for screw malposition.
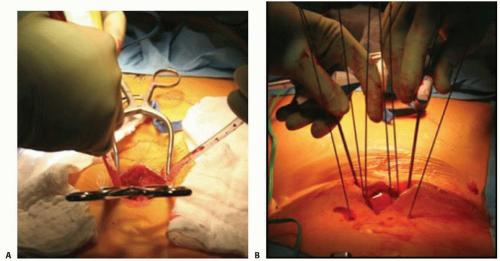
In addition, corrective maneuvers for fracture reduction need to be planned. Fracture reduction can be accomplished with a mini-open technique at the fracture level (FIG 1A), through patient positioning, or with more standardized compression-distraction forces through the pedicular implants.
Achieving biologic fusion is challenging in multilevel traumatic cases, and the benefit of doing so is not entirely clear. If necessary, the fusion procedure can be performed in a staged fashion through a standardized midline approach when the patient is physiologically stable (“damage control”).
Alternatively, in cases in which anterior reconstruction or decompression is indicated, fusion can be achieved anteriorly with stabilization performed posteriorly with minimally invasive percutaneous pedicle screw placement.
Other options for achieving fusion include the use of a posterior cannula through a midline posterior approach to the facet joint. FIG 1B shows a hybrid approach to facet fusion, combining percutaneous fixation and a mini-open technique.
Positioning
The operative setup and positioning for minimally invasive spine procedures are the same as for conventional open posterior procedures.
The patient is positioned prone on a radiolucent table, with care being taken to pad the entire body in a systematic fashion.
Ensure that the eyes are well protected, the cervical spine is in a neutral position, the arms are positioned in 90 degrees of abduction and 90 degrees of elbow flexion, the bony prominences are well padded, and vital structures and distal extremities are protected from incidental injury during the operation. Additionally, the abdomen must be free of compression to improve venous return.
Approach
Percutaneous pedicle instrumentation can be performed by one of four methods: true anteroposterior (AP) targeting, Magerl (or owl’s eye) technique, image-guided navigation, and biplanar fluoroscopy.
We describe the first two methods because these are the authors’ preferred techniques for the following reasons:
By using only a true AP view, the setup is more time efficient.
Sterility is maintained when not alternating between AP and lateral views.
Two surgeons can operate simultaneously on both sides, thereby reducing procedure time and radiation exposure. However, this technique might not be feasible for every patient. Obesity, severely deformed anatomy, and osteopenia are factors that might preclude acceptable imaging of vertebral landmarks.
TECHNIQUES
▪ Fluoroscopic Imaging
When performing MISS, fluoroscopic imaging is essential. Therefore, the surgeon must be able to obtain a clear image and identify each vertebral body that requires treatment in both the AP and lateral views.
After the patient is positioned, the surgeon should obtain a true AP view with the center of the x-ray beam parallel to the superior endplate of the vertebra. This will produce a single superior endplate shadow as the anterior and posterior margins are superimposed on each other.
Furthermore, the pedicle shadows should be just inferior to the superior endplate shadow and the spinous process will lie equidistant between the pedicles (TECH FIG 1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree