Percutaneous Achilles Tendon Repair: Perspective 1
Karen M. Sutton
Sandra L. Tomak
Lamar L. Fleming
DEFINITION
Achilles tendon ruptures typically occur about 2 to 6 cm proximal to the tendon’s insertion site on the calcaneus.
This injury is relatively common among both high-performance athletes and the recreational athlete, particularly the “weekend warrior.”
Ruptures occur most often in men between 30 and 50 years of age.
ANATOMY
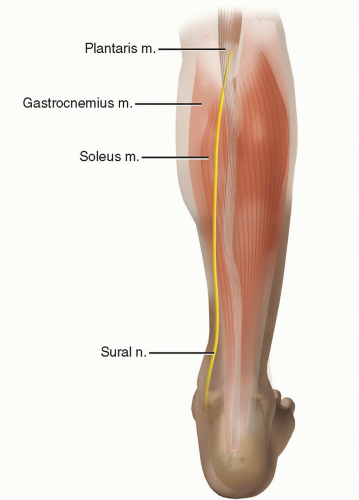
Tendinous portions of the gastrocnemius and soleus muscles coalesce to form the Achilles tendon (FIG 1).
The plantaris muscle is a distinct entity medial to the Achilles tendon.
The soleus tendon originates as a band proximally on the posterior surface of its muscle and the gastrocnemius tendon emerges from the distal margin of the muscle bellies.
The length of the tendon formed from the gastrocnemius and soleus range from 11 to 26 cm and 3 to 11 cm, respectively.
Viewed from proximal to distal, the Achilles tendon progressively becomes thinner in its anteroposterior dimensions, particularly from 4 cm proximal to the calcaneus to its insertion on the calcaneus.5
Ninety-five percent of the tendon collagen is type I collagen; a small percentage is elastic. Seventy percent of the dry weight of the tendon is collagen.18
The blood supply to the Achilles tendon arises from the musculotendinous junction, the osseous insertion, and multiple mesotenal vessels.
The tendon is most poorly vascularized at its midportion, receiving its blood supply from the paratenon.22 The mesotenal vessels decrease in number 2 to 6 cm proximal to the osseous insertion.24
The Achilles tendon receives much of its nutrition from the tenosynovial fluid that bathes the tendon and is contained within the paratenon.
PATHOGENESIS
Ruptures occur most commonly during athletic activities.
Both hyperpronation and cavus foot alignment are associated with Achilles tendon injuries. The cavus foot is thought to place more stress on the lateral side of the Achilles tendon and to absorb shock poorly.21
Inconsistent training, including sudden increases in training intensity; excessive training; training on hard surfaces; and running on sloping, hard, or slippery roads have been implicated in Achilles tendon problems.21
Mechanisms of injury, leading to eccentric loads on the Achilles tendon, include pushing off with the weight-bearing forefoot while extending the knee, unexpected dorsiflexion of the ankle, or violent dorsiflexion of a plantarflexed foot.1
With normal aging, the Achilles tendon decreases in cell density, collagen fibril diameter and density, and fiber waviness. These changes may make the aging athlete more susceptible to injury.24
NATURAL HISTORY
Chronic Achilles tendon injuries typically result in the patient’s inability to complete everyday tasks such as climbing stairs.9
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient reports sudden pain in the affected leg.
Some patients recall an audible pop or snap.
With Achilles tendon ruptures, patients occasionally experience a sensation as though they were “kicked” or “hit” in the injured calf.
Patients report an inability to bear weight and have weakness of the affected lower extremity.
Physical examination should include the following:
Palpation of gap: Palpate along the posterior aspect of the lower leg and a gap may be felt along the course of the tendon.
Positive: appreciable gap
Thompson test: With the patient prone, squeeze the proximal portion of the calf.
Positive: no plantarflexion of the ankle
False-positive results may be obtained with an intact plantaris tendon.
Knee flexion test: With the patient prone, have him or her actively flex both knees to 90 degrees.
Positive: asymmetric resting tension of both ankles; the affected foot may even fall into neutral or dorsiflexion
Needle test: Insert a hypodermic needle into the calf medial to the midline and 10 cm proximal to the insertion of the tendon. The ankle is put through passive range of motion.
Positive: The needle points proximally on dorsiflexion.
This test is usually only performed if there remains a high index of suspicion with the other tests being equivocal.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs (rarely required in evaluation of Achilles tendon ruptures)
In a lateral radiograph, the fat-filled triangular space (ie, Kager triangle) anterior to the Achilles tendon and between the posterior aspect of the tibia and the superior aspect of the calcaneus loses its regular configuration.
Magnetic resonance imaging (MRI) (FIG 2) (rarely required in evaluation of Achilles tendon ruptures)
T1- and T2-weighted images in the axial and sagittal planes should be used to evaluate Achilles tendon ruptures.
T1 weighted: A complete rupture of the Achilles tendon is identified as a disruption of the signal within the tendon.

FIG 2 • T2-weighted MRI scan displaying a complete rupture of the Achilles tendon about 5 cm proximal to the insertion site on the calcaneus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access