Pedicled and Free Latissimus Flap for Elbow and Forearm Coverage
Kenji Kawamura
Kevin C. Chung
Indications/Contraindications
The latissimus dorsi (LD) has proven to be a reliable muscle in the coverage of soft tissue defects about the shoulder and elbow. Familiarity with this muscle and its application in cases of trauma is essential for all upper extremity surgeons. The major arterial inflow and venous outflow for the LD flap is based on the thoracodorsal artery and venae comitantes. The average diameter of the thoracodorsal artery is 2.5 mm, and that of venae comitantes is 3.0 mm. The average length of maximum vascular pedicle is 12 cm, which can be obtained by dissecting the thoracodorsal vessels toward the proximal axillary artery and vein.
The indication for the use of the LD flap to the elbow and forearm is to cover a large skin and soft tissue defect that cannot be managed with local flaps. In cases in which vital muscle structures were damaged, the LD flap can provide coverage of soft tissue defects, as well as functional muscle transfer to restore of elbow, wrist, and finger motion. Unstable soft tissue coverage over elbow fracture or recalcitrant infection around the elbow may also be amenable to the LD flap because this flap provides well-vascularized tissue that can seal dead spaces and increase blood flow to the local environment.
The pedicled LD flap can cover the forearm up to approximately 8 cm distal to the olecranon when transposed anteriorly, and about 6 cm distal to the olecranon when transposed posteriorly. Soft tissue defects over 8 cm distal from the olecranon are not suitable for the pedicled LD flap transfer, and if this muscle is to be used, the free LD flap transfer should be considered.
Contraindications for flap use include previous injury to the muscle or pedicle, such as in cases of previous thoracotomy, axillary arterial injury, or in some cases, axillary lymphadenectomy. Breast cancer surgery may injure the nerve or arterial supply to the LD muscle, rendering it fibrotic and inadequate for transfer. In such patients, palpation of a contracting LD muscle usually verifies an uninjured nerve and vascular pedicle.
The LD muscle functions as an expendable adductor, extender, and internal rotator of the arm. These functions are essential for activities of daily living for patients with contralateral shoulder girdle paralysis or extremity paralysis from spinal cord injury. One must be careful in evaluating the impact of removing the LD muscle in these situations. In general, one should not use the LD muscle for soft tissue coverage in these patients because of functional requirements.
Preoperative Planning
The LD flap can be harvested as not only a muscle flap but also a musculocutaneous flap. Muscle flap covered with skin graft is less bulky and can seal deep defects, however, musculocutaneous flap gives better aesthetic reconstruction because the skin paddle can conform to the skin texture of the upper arm. When a LD musculocutaneous flap is applied, it is recommended that the skin paddle is designed several centimeters superior to the muscle origin at the iliac crest to avoid the risk of skin paddle necrosis because the blood supply of the subcutaneous tissue near the origin is inconsistent. When greater flap reach is required, a portion of the skin paddle may be designed over the inferior margin of the muscle. This technique can facilitate a greater distal coverage of the forearm when the pedicled LD musculocutaneous flap is rotated. The entire skin paddle can survive if enough musculocutaneous perforators are included in the proximal portion of the skin paddle design.
The arc of transposition of the LD flap depends on the location of the wound. When defects are present in the posterior aspect of the elbow and forearm, posterior arc transposition of the pedicled LD flap is recommended. Similarly, when defects are present in the anterior aspect, anterior arc transposition is recommended.
It is important to assess the strength of the LD muscle preoperatively when the LD flap is used for simultaneous soft tissue coverage and functional restoration. When a soft tissue defect is caused by a trauma, particularly associated with a motorcycle accident, the LD muscle may be paralyzed by brachial plexus injury. If the paralyzed LD muscle is planned to be used as a functional transfer, reinnervation of the LD muscle by another motor nerve, for example, intercostal nerve or accessory nerve, can be performed during operative procedures. LD muscle previously paralyzed by neurologic disorders can only be used for soft tissue coverage and should not be used for functional muscle transfer.
Preoperative angiography of the injured upper extremity will help plan for free LD flap transfer. The free flap transfer may require a more proximal vessel dissection, vein grafting, and end-to-side anastomoses in cases with a potential disruption of the recipient vessels.
For aesthetic consideration at the donor site, it is important to ask for the patient’s clothing preference preoperatively for planning the skin incision. For example, a transverse incision along the bra line is recommended to conceal the donor site scar for a woman, but an oblique incision may be suitable for a patient who likes to wear backless dresses. Furthermore, the endoscopic harvesting technique may be preferred for children, those who are prone to hypertrophic scars, and for other aesthetic considerations.
Surgery
The patient, under general anesthesia, is placed in the lateral decubitus position. The injured upper limb and ipsilateral hemithorax caudal to the iliac crest are prepped and draped. The injured upper limb is supported on a sterile Mayo stand with a 90-degree abduction position of the shoulder (Fig. 11-1A). The lateral buttock and thigh are also prepared for skin grafting if necessary. A beanbag or axillary roll with padding is placed on the opposite axilla to protect the dependent shoulder in the decubitus position, and all other pressure points are also carefully padded.
In cases of traumatic defects, the wounds are again thoroughly debrided before the flap procedure is performed. When a LD musculocutaneous flap is applied, the skin paddle that includes the perforators arising from the branch of the thoracodorsal artery is designed on the LD muscle. There is a longitudinal row of perforators 2 to 5 centimeters from the lateral border of the LD muscle, which can be easily identified with a Doppler blood flowmeter. The largest skin paddle that can be moved safely is 20 × 15 cm, however, primary closure is only possible with skin paddles 8 cm in width.
The procedure is performed with ×2.5 loupe magnification. The incision usually begins at the posterior aspect of the axilla angled along the anterolateral border of the latissimus dorsi muscle and extends inferiorly to the iliac crest. An aesthetic incision in a woman is designed in a transverse incision along the bra line. The LD muscle is dissected medially to the paraspinous muscle and caudally to the lumbosacral fascia. The origin of the muscle is detached from the thoracic and lumbar vertebra, posterior ribs, and lumbosacral fascia. The flap is elevated superiorly toward the axilla to separate the undersurface of the muscle from the chest wall. Perforators from the intercostal and lumbar arteries are clipped. The neurovascular pedicle, which includes the thoracodorsal artery, venae comitantes, and nerve, is identified more proximally on the undersurface of the muscle. The thoracodorsal
vessels are carefully dissected toward the proximal axillary artery. The circumflex scapular vessels and the serratus anterior and teres major branches are ligated to allow maximal pedicle length. Leaving the thoracodorsal nerve intact may be considered when the flap is transferred on the pedicle, even though the flap is not used as a functional transfer. Retaining innervation minimizes postoperative muscle atrophy and will maintain muscle thickness and durability. This consideration is particularly important for distal elbow coverage when the thin muscle near the origin of the LD muscle at the iliac crest maintains its bulk.
vessels are carefully dissected toward the proximal axillary artery. The circumflex scapular vessels and the serratus anterior and teres major branches are ligated to allow maximal pedicle length. Leaving the thoracodorsal nerve intact may be considered when the flap is transferred on the pedicle, even though the flap is not used as a functional transfer. Retaining innervation minimizes postoperative muscle atrophy and will maintain muscle thickness and durability. This consideration is particularly important for distal elbow coverage when the thin muscle near the origin of the LD muscle at the iliac crest maintains its bulk.
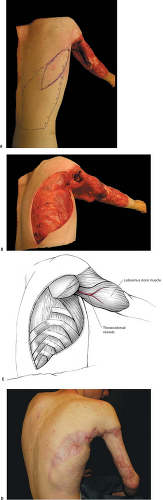 FIGURE 11-1 A: The patient was placed in the lateral decubitus position with the injured upper limb on a sterile Mayo stand with a 90-degree abduction position of the shoulder. B:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|





