Pediatric Wrist and Hand
INJURIES TO THE CARPUS
Epidemiology
Rare, although carpal injuries may be underappreciated owing to difficulties in examining an injured child and the limited ability of plain radiographs to detail the immature skeleton.
The adjacent physis of the distal radius is among the most commonly injured; this is protective of the carpus as load transmission is diffused by injury to the distal radial physis, thus partially accounting for the rarity of pediatric carpal injuries.
Anatomy
The cartilaginous anlage of the wrist begins as a single mass; by the 10th week, this transforms into eight distinct masses, each in the contour of its respective mature carpal bone.
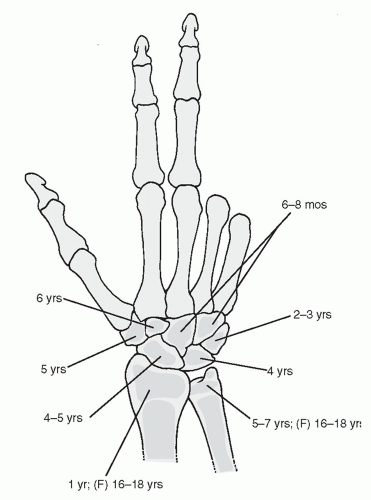
The appearance of ossification centers of the carpal bones ranges from 6 months for the capitate to 8 years of age for the pisiform. The order of appearance of the ossification centers is very consistent: capitate, hamate, triquetrum, lunate, scaphoid, trapezium, trapezoid, and pisiform (Fig. 46.1).
The ossific nuclei of the carpal bones are uniquely protected by cartilaginous shells. As the child matures, a critical bone-to-cartilage ratio is reached, after which carpal fractures are increasingly common (adolescence).
Mechanism of Injury
The most common mechanism of carpal injury in children is direct trauma to the wrist.
Clinical Evaluation
The clinical presentation of individual carpal injuries is variable, but in general, the most consistent sign of carpal injury is well-localized tenderness. In the agitated child, however, appreciation of localized tenderness may be difficult because distal radial pain may be confused with carpal tenderness.
A neurovascular examination is important, with documentation of distal sensation in median, radial, and ulnar distributions, appreciation of movement of all digits, and assessment of distal capillary refill.
Gross deformity may be present, ranging from displacement of the carpus to prominence of individual carpal bones.
Radiographic Evaluation
Anteroposterior (AP) and lateral views of the wrist should be obtained.
Comparison views of the uninjured, contralateral wrist may be helpful.
Scaphoid Fracture
The scaphoid is the most commonly fractured carpal bone.
The peak incidence occurs at age 15 years; injuries in the first decade are extremely rare, owing to the abundant cartilaginous envelope.
Unlike adults, the most common mechanism is direct trauma, with fractures of the distal one-third the most common. Proximal pole fractures are rare and typically result from scapholunate ligament avulsion.
Clinical evaluation: Patients present with wrist pain and swelling, with tenderness to deep palpation overlying the scaphoid and anatomic snuffbox. The snuffbox is typically obscured by swelling.
Radiographic evaluation: The diagnosis can usually be made on the basis of anteroposterior (AP) and lateral views of the wrist. Oblique views and scaphoid views, or a posterior-anterior (PA) view in ulnar deviation of the wrist, may aid in the diagnosis or assist in further fracture definition. Technetium bone scan has been replaced with magnetic resonance imaging. Alternatively, computed tomography and ultrasound evaluation may be used to diagnose occult scaphoid fractures.
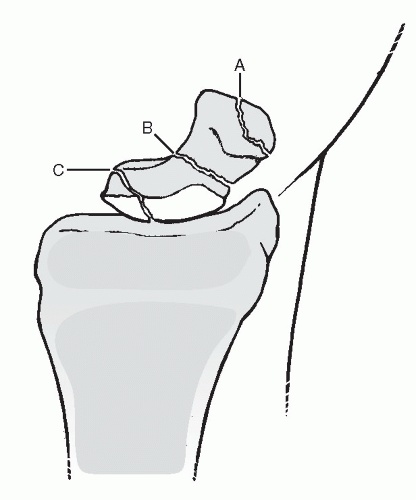
Classification (Fig. 46.2)
Type A: Fractures of the distal pole
A1: Extra-articular distal pole fractures
A2: Intra-articular distal pole fractures
Type B: Fractures of the middle third (waist fractures)
Type C: Fractures of the proximal pole
Treatment
A fracture should be presumed if snuffbox tenderness is present, even if a fracture is not obvious on plain radiographs. Initial treatment in the emergency department should consist of a thumb spica splint or cast immobilization if swelling is not pronounced. In the pediatric population, a long arm cast or splint is typically necessary for adequate initial immobilization. This should be maintained for 2 weeks, at which time repeat evaluation should be undertaken.
For stable, nondisplaced fractures, a long arm cast should be placed with the wrist in neutral deviation and flexion/extension and
maintained for 6 to 8 weeks or until radiographic evidence of healing has occurred.
Displaced fractures in the pediatric population may be initially addressed with closed reduction and percutaneous pinning. Distal pole fractures can generally be reduced by traction and ulnar deviation.
Residual displacement >1 mm, angulation >10 degrees, or scaphoid fractures in adolescents generally require open reduction and internal fixation. A headless compression screw or smooth Kirschner wires may be used for fracture fixation, with postoperative immobilization consisting of a long arm thumb spica cast for 6 weeks.
Complications
Delayed union, nonunion, and malunion: These are rare in the pediatric population and may necessitate operative fixation with bone grafting to achieve union.
Osteonecrosis: Extremely rare in the pediatric population and occurs with fractures of the proximal pole in skeletally mature individuals.
Missed diagnosis: Clinical suspicion should outweigh normal appearing radiographs and a brief period of immobilization (2 weeks) can be followed by repeat clinical examination and further radiographic studies if warranted.
Lunate Fracture
This extremely rare injury occurs primarily from severe, direct trauma (e.g., crush injury).
Clinical evaluation reveals tenderness to palpation on the volar wrist overlying the distal radius and lunate, with painful range of motion.
Radiographic evaluation: AP and lateral views of the wrist are often inadequate to establish the diagnosis of lunate fracture because osseous details are frequently obscured by overlapping densities.
Oblique views may be helpful, but computed tomography or technetium bone scanning are better for diagnosis.
Treatment
Nondisplaced fractures or unrecognized fractures generally heal uneventfully and may be recognized only in retrospect. When diagnosed, they should be treated in a short arm cast or splint for 2 to 4 weeks until radiographic and symptomatic healing occurs.
Displaced or comminuted fractures should be treated surgically to allow adequate apposition for formation of vascular anastomoses. This may be achieved with open reduction and internal fixation, although the severity of the injury mechanism typically results in concomitant injuries to the wrist that may result in growth arrest.
Complications
Osteonecrosis: Referred to as “lunatomalacia” in the pediatric population, this occurs in children less than 10 years of age. Symptoms are rarely dramatic. Radiography reveals mildly increased density of the lunate with no change in morphology. Immobilization of up to 1 year may be necessary for treatment, but it usually results in good functional and symptomatic recovery.
Triquetrum Fracture
Rare, but the true incidence is unknown owing to the late ossification of the triquetrum, with potential injuries unrecognized.
The mechanism of fracture is typically direct trauma to the ulnar wrist or avulsion by dorsal ligamentous structures.
Clinical evaluation reveals tenderness to palpation on the dorsoulnar aspect of the wrist as well as painful range of motion.
Radiographic evaluation: Transverse fractures of the body can generally be identified on AP views in older children and adolescents. Distraction views may be helpful in these cases.
Treatment
Nondisplaced fractures of the triquetrum body or dorsal chip fractures may be treated in a short arm cast or ulnar gutter splint for 2 to 4 weeks when symptomatic improvement occurs.
Significantly displaced fractures may be amenable to open reduction and internal fixation.
Pisiform Fracture
No specific discussions of pisiform fractures in the pediatric population exist in the literature.
Direct trauma causing a comminuted fracture or a flexor carpi ulnaris avulsion may occur in late adolescence.
Radiographic evaluation is typically unrevealing, because ossification of the pisiform does not occur until age 8 years.
Treatment is symptomatic only, with immobilization in an ulnar gutter splint until the patient is comfortable.
Trapezium Fracture
Extremely rare in children and adults.
The mechanism of injury is axial loading of the adducted thumb, driving the base of the first metacarpal onto the articular surface of the trapezium with dorsal impaction. Avulsion fractures may occur with forceful deviation, traction, or rotation of the thumb. Direct trauma to the palmar arch may result in avulsion of the trapezial ridge by the transverse carpal ligament.
Clinical evaluation reveals tenderness to palpation of the radial wrist, accompanied by painful range of motion at the first carpometacarpal joint with stress testing.
Radiographic evaluation: Fractures are difficult to identify because of the late ossification of the trapezium. In older children and adolescents, identifiable fractures may be appreciated on standard AP and lateral views.
Superimposition of the first metacarpal base may be eliminated by obtaining a Robert view or a true AP view of the first carpometacarpal joint and trapezium.
Treatment:
Most fractures are amenable to thumb spica splinting or casting to immobilize the first carpometacarpal joint for 3 to 5 weeks.
Rarely, severely displaced fractures may require open reduction and internal fixation to restore articular congruity and maintain carpometacarpal joint integrity.
Trapezoid Fracture
Fractures of the trapezoid in children are extremely rare.
Axial load transmitted through the second metacarpal may lead to dislocation, more often dorsal, with associated capsular ligament disruption. Direct trauma from blast or crush injuries may cause trapezoid fracture.
Clinical evaluation demonstrates tenderness proximal to the base of the second metacarpal with painful range of motion of the second carpometacarpal joint.
Radiographic evaluation: Fractures are difficult to identify secondary to late ossification. In older children and adolescents, they may be identified on the AP radiograph based on a loss of the normal relationship
between the second metacarpal base and the trapezoid. Comparison with the contralateral, normal wrist may aid in the diagnosis. The trapezoid, or fracture fragments, may be superimposed over the trapezium or capitate, and the second metacarpal may be proximally displaced.
Treatment:
Most fractures may be treated with a splint or short arm cast for 3 to 5 weeks.
Severely displaced fractures may require open reduction and internal fixation with Kirschner wires with attention to restoration of articular congruity.
Capitate Fracture
Uncommon as an isolated injury owing to its relatively protected position.
A fracture of the capitate is more commonly associated with greater arc injury pattern (transscaphoid, transcapitate perilunate fracturedislocation). A variation of this is the naviculocapitate syndrome, in which the capitate and scaphoid are fractured without associated dislocation.
The mechanism of injury is typically direct trauma or a crushing force that results in associated carpal or metacarpal fracture. Hyperdorsiflexion may cause impaction of the capitate waist against the lunate or dorsal aspect of the radius.
Clinical evaluation reveals point tenderness as well as variable painful dorsiflexion of the wrist as the capitate impinges on the dorsal rim of the radius.
Radiographic evaluation:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree