Pediatric Shoulder
PROXIMAL HUMERUS FRACTURES
Epidemiology
These account for <5% of fractures in children.
Incidence ranges from 1.2 to 4.4 per 10,000 per year.
They are most common in adolescents owing to increased sports participation and are often metaphyseal, physeal, or both.
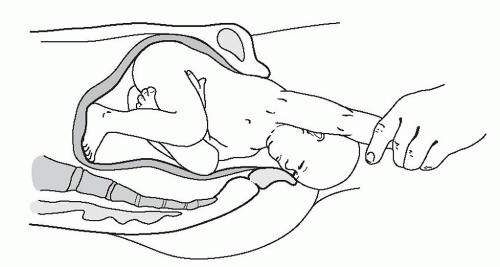
Neonates may sustain birth trauma to the proximal humeral physis, representing 1.9% to 6.7% of physeal injuries (Fig. 43.1).
Anatomy
Eighty percent of humeral growth occurs at the proximal physis, giving this region great remodeling potential.
There are three centers of ossification in the proximal humerus:
Humeral head: This ossifies at 6 months.
Greater tuberosity: This ossifies at 1 to 3 years.
Lesser tuberosity: This ossifies at 4 to 5 years.
The greater and lesser tuberosities coalesce at 6 to 7 years and then fuse with the humeral head between 7 and 13 years of age.
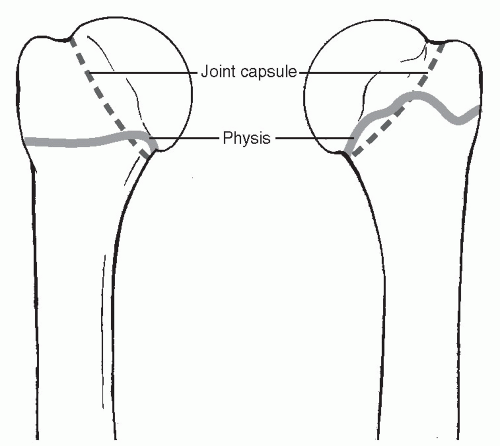
The joint capsule extends to the metaphysis, rendering some fractures of the metaphysis intracapsular (Fig. 43.2).
The primary vascular supply is via the anterolateral ascending branch of the anterior circumflex artery, with a small portion of the greater tuberosity and inferior humeral head supplied by branches of the posterior circumflex artery.
The physis closes at ages 14 to 17 years in girls and at ages 16 to 18 years in boys.
The physeal apex is posteromedial and is associated with a strong, thick periosteum.
Type I physeal fractures occur through the hypertrophic zone adjacent to the zone of provisional calcification. The layer of embryonal cartilage is preserved, leading to normal growth.
Muscular deforming forces: The subscapularis attaches to the lesser tuberosity. The remainder of the rotator cuff (teres minor, supraspinatus, and infraspinatus) attaches to the posterior epiphysis and greater tuberosity. The pectoralis major attaches to the anterior medial metaphysis, and the deltoid connects to the lateral shaft.
Mechanism of Injury
Indirect: Resulting from a fall backward onto an outstretched hand with the elbow extended and the wrist dorsiflexed. Birth injuries may
occur as the arm is hyperextended or rotated as the infant is being delivered. Shoulder dystocia is strongly associated with macrosomia from maternal diabetes.
Direct: Resulting from direct trauma to the posterolateral aspect of the shoulder.
Clinical Evaluation
Newborns present with pseudoparalysis with the arm held in extension. A history of birth trauma may be elicited. A fever is variably present. Infection, clavicle fracture, shoulder dislocation, and brachial plexus injury must be ruled out.
Older children present with pain, dysfunction, swelling, and ecchymosis, and the humeral shaft fragment may be palpable anteriorly. The shoulder is tender to palpation, with a painful range of motion that may reveal crepitus.
Typically, the arm is held in internal rotation to prevent anteromedial pull of the distal fragment by the pectoralis major.
A careful neurovascular examination is required, including assessment of the axillary, musculocutaneous, radial, ulnar, and median nerves.
Radiographic Evaluation
Anteroposterior (AP), lateral (in the plane of the scapula; “Y” view), and axillary views should be obtained, with comparison views of the contralateral side if necessary.
Ultrasound: This may be necessary in the newborn because the epiphysis is not yet ossified.
Computed tomography may be useful to aid in the diagnosis and classification of posterior dislocations and complex fractures.
Magnetic resonance imaging is more useful than bone scan to detect occult fractures because the physis normally has increased radionuclide uptake, making a bone scan difficult to interpret.
Classification
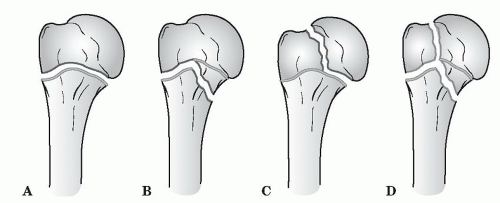
Salter-Harris (Fig. 43.3)
Type I: Transphyseal fracture; usually a birth injury
Type II: Transphyseal fracture that exits through the metaphysis; usually occurring in adolescents (>12 years old); metaphyseal fragment always posteromedial
Type III: Transphyseal fracture that exits through the epiphysis uncommon; associated with dislocations
Type IV: Rare; fracture that traverses the epiphysis and the physis, exiting the metaphysis; associated with open fractures
Neer-Horowitz Classification of Proximal Humeral Plate Fractures
Grade I: <5 mm displacement
Grade II: Displacement less than one-third the width of the shaft
Grade III: Displacement one-third to two-thirds the width of the shaft
Grade IV: Displacement greater than two-thirds the width of the shaft, including total displacement
Treatment
Treatment depends on the age of the patient as well as the fracture pattern.
Newborns
Most fractures are Salter-Harris type I. The prognosis is excellent.
Ultrasound can be used to guide reduction.
Closed reduction: This is the treatment of choice and is achieved by applying gentle traction, 90 degrees of flexion, then 90 degrees of abduction and external rotation.
Stable fracture: The arm is immobilized against the chest for 5 to 10 days.
Unstable fracture: The arm is held abducted and is externally rotated for 3 to 4 days to allow early callus formation.
Ages 1 to 4 Years
These are typically Salter-Harris type I or, less frequently, type II.
Treatment is by closed reduction.
The arm is held in a sling for 10 days followed by progressive return to activity.
Extensive remodeling is possible.
Ages 5 to 12 Years
The metaphyseal fracture (type II) is the most common in this age group because this area is undergoing the most rapid remodeling and is therefore structurally vulnerable.
Treatment is by closed reduction. Most are stable following reduction.
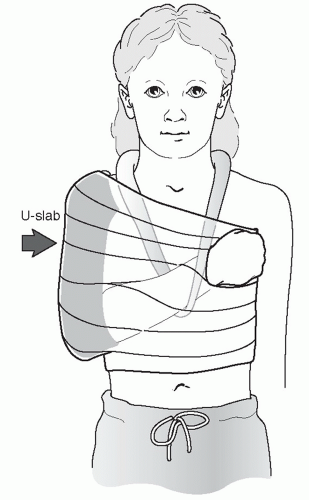
Stable fracture: A sling and swathe is used (Fig. 43.4).
Unstable fracture: The arm is placed in a shoulder spica cast with the arm in the salute position for 2 to 3 weeks, after which the patient may be placed in a sling, with progressive return to activity.
Ages 12 Years to Maturity
These are either Salter-Harris type II or, less frequently, type I.
Treatment is typically by closed reduction.
There is less remodeling potential than in younger children.
Stable fracture: A sling and swathe is used for 2 to 3 weeks followed by progressive range-of-motion exercises.
Unstable fracture and Salter-Harris type IV: Immobilization is maintained in a shoulder spica cast with the arm in the salute position for 2 to 3 weeks, after which the patient may be placed in a sling, with progressive return to activity.
One should consider surgical stabilization for displaced fractures in adolescents.
Acceptable Deformity
Ages 1 to 4 years: 70 degrees of angulation with any amount of displacement
Ages 5 to 12 years: 40 to 45 degrees of angulation and displacement of one-half the width of the shaft
Ages 12 years to maturity: 15 to 20 degrees of angulation and displacement of <30% the width of the shaft
Open Treatment
Indications for open reduction and internal fixation include:
Open fractures
Fractures with associated neurovascular compromise
Salter-Harris types III and IV fractures with displacement
Irreducible fractures with soft tissue interposition (biceps tendon)
In children, fixation is most often achieved with percutaneous, smooth Kirschner wires or Steinmann pins.
Prognosis
Neer-Horowitz grades I and II fractures do well because of the remodeling potential of the proximal humeral physis.
Neer-Horowitz grades III and IV fractures may be left with up to 3 mm of shortening or residual angulation. This is well tolerated by the patient and is often clinically insignificant.
As a rule, the younger the patient, the higher the potential for remodeling and the greater the acceptable initial deformity.
Complications
Proximal humeral varus: Rare, usually affecting patients less than 1 year of age, but it may complicate fractures in patients as old as 5 years of age. It may result in a decrease of the neck-shaft angle to 90 degrees with humeral shortening and mild-to-moderate loss of glenohumeral abduction. Remodeling potential is great in this age group, however, so improvement is likely without intervention. Proximal humeral osteotomy may be performed in cases of extreme functional limitation.
Limb length inequality: Rarely significant and tends to occur more commonly in surgically treated patients as opposed to those treated nonoperatively.
Loss of motion: Rare and tends to occur more commonly in surgically treated patients. Older children tend to have more postfracture difficulties with shoulder stiffness than younger children.
Inferior glenohumeral subluxation: May complicate patients with Salter-Harris type II fractures of the proximal humerus secondary to a loss
of deltoid and rotator cuff tone. It may be addressed by a period of immobilization followed by rotator cuff strengthening exercises.
Osteonecrosis: May occur with associated disruption of the anterolateral ascending branch of the anterior circumflex artery, especially in fractures or dislocations that are not acutely reduced. This is almost never seen in closed fractures.
Nerve injury: Most commonly axillary nerve injury in fracture-dislocations. Lesions that do not show signs of recovery in 4 months should be explored.
Growth arrest: May occur when the physis is crushed or significantly displaced or when a physeal bar forms. It may require excision of the physeal bar. Limb lengthening may be required for functional deficits or severe cosmetic deformity.
CLAVICLE FRACTURES
Epidemiology
Most frequent long bone fracture in children (8% to 15% of all pediatric fractures).
These occur in 0.5% of normal deliveries and 1.6% of breech deliveries (they account for 90% of obstetric fractures). The incidence of birth fractures involving the clavicle ranges from 2.8 to 7.2 per 1,000 term deliveries, and clavicular fractures account for 84% to 92% of all obstetric fractures.
In macrosomic infants (>4,000 g), the incidence is 13%.
Eighty percent of clavicle fractures occur in the midshaft, most frequently just lateral to the insertion of the subclavius muscle, which protects the underlying neurovascular structures.
Ten percent to 15% of clavicle fractures involve the lateral aspect, with the remainder representing medial fractures (5%).
Anatomy
The clavicle is the first bone to ossify; this occurs by intramembranous ossification.
The secondary centers develop via endochondral ossification:
The medial epiphysis, where 80% of growth occurs, ossifies at ages 12 to 19 years and fuses by ages 22 to 25 years (last bone to fuse).
The lateral epiphysis does not ossify until it fuses at age 19 years.
Clavicular range of motion involves rotation about its long axis (approximately 50 degrees) accompanied by elevation of 30 degrees with full shoulder abduction and 35 degrees of anterior-posterior angulation with shoulder protraction and retraction.
The periosteal sleeve always remains in the anatomic position. Th erefore, remodeling is ensured.
Mechanism of Injury
Indirect: Fall onto an outstretched hand.
Direct: This is the most common mechanism, resulting from direct trauma to the clavicle or acromion; it carries the highest incidence of injury to the underlying neurovascular and pulmonary structures.
Birth injury: Occurs during delivery of the shoulders through a narrow pelvis with direct pressure from the symphysis pubis or from obstetric pressure directly applied to the clavicle during delivery.
Medial clavicle fractures or dislocations usually represent Salter-Harris type I or II fractures. True sternoclavicular joint dislocations are rare. The inferomedial periosteal sleeve remains intact and provides a scaffold for remodeling. Because 80% of the growth occurs at the medial physis, there is great potential for remodeling.
Lateral clavicle fractures occur as a result of direct trauma to the acromion. The coracoclavicular ligaments always remain intact and are attached to the inferior periosteal tube. The acromioclavicular ligament is always intact and is attached to the distal fragment.
Clinical Evaluation
Birth fractures of the clavicle are usually obvious, with an asymmetric, palpable mass overlying the fractured clavicle. An asymmetric Moro reflex is usually present. Nonobvious injuries may be misdiagnosed as congenital muscular torticollis because the patient will often turn his or her head toward the fracture to relax the sternocleidomastoid muscle.
Children with clavicle fractures typically present with a painful, palpable mass along the clavicle. Tenderness is usually discrete over the site of injury, but it may be diffuse in cases of plastic bowing. There may be tenting of the skin, crepitus, and ecchymosis.
Neurovascular status must be carefully evaluated because injuries to the brachial plexus and upper extremity vasculature may occur. Rule out brachial plexus palsy.
Pulmonary status must be assessed, especially if direct trauma is the mechanism of injury. Medial clavicular fractures may be associated with tracheal compression, especially with severe posterior displacement.
Differential diagnosis
Cleidocranial dysostosis: This defect in intramembranous ossification, most commonly affecting the clavicle, is characterized by absence of the distal end of the clavicle, a central defect, or complete absence of the clavicle. Treatment is symptomatic only.
Congenital pseudarthrosis: This most commonly occurs at the junction of the middle and distal thirds of the right clavicle, with smooth, pointed bone ends. Pseudarthrosis of the left clavicle is
found only in patients with dextrocardia. Patients present with no antecedent history of trauma, only a palpable bump. Treatment is supportive only, with bone grafting and intramedullary fixation reserved for symptomatic cases.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree