The knee is a ginglymoid (hinge) joint consisting of three articulations: patellofemoral, tibiofemoral, and tibiofibular.
Under normal cyclic loading, the knee may experience up to five times body weight per step.
The normal range of motion is from 10 degrees of extension to 140 degrees of flexion, with 8 to 12 degrees of rotation through the flexion/extension arc.
The dynamic and static stability of the knee is conferred mainly by soft tissues (ligaments, muscles, tendons, menisci) in addition to the bony articulations.
Because ligaments in the immature skeleton are more resistant to tensile stresses than are physeal plates and metaphyseal bone, trauma leads to physeal separation and avulsions not seen in the skeletally mature patient.
There are three physeal plates with secondary ossification centers.
Appearance of ossification centers is as follows:
Distal femur: 39th fetal week
Proximal tibia: by 2 months
Tibial tubercle: 9 years
Physeal closure is as follows:
Distal femur: 16 to 19 years
Proximal tibia: 16 to 19 years
Tibial tubercle: 15 to 17 years
The patella is a sesamoid bone, with its own ossification center, which appears at age 3 to 5 years.
Tibial spine: This is the site of insertion of the anterior cruciate ligament (ACL).
Two-thirds of longitudinal growth of the lower extremity is provided by the distal femoral (9 mm per year) and proximal tibial (6 mm per year) physes.
This is the most commonly injured physis around the knee.
They comprise 1% to 6% of all physeal injuries and less than 1% of all fractures in children.
Most (two-thirds) are Salter-Harris type II fractures and occur in adolescents.
They comprise 12% to 18% of all femur fractures in children.
The distal femoral epiphysis is the largest and fastest growing physis in the body.
There is no inherent protection of the physis. Ligamentous and tendinous structures insert on the epiphysis.
The sciatic nerve divides at the level of the distal femur.
The popliteal artery gives off the superior geniculate branches to the knee just posterior to the femoral metaphysis.
Direct trauma to the distal femur may occur from vehicular trauma, falling onto a flexed knee, or during athletic activity, such as a lateral blow to the knee with a planted, cleated foot as in football. In infants, distal femoral fracture may be associated with child abuse.
Indirect injury: Varus/valgus or hyperextension/hyperflexion force; results in simultaneous compression to one aspect of the physis with distraction to the other. Indirect force may result in epiphyseal separation from the metaphysis. Most typically, the physeal separation begins on the tension side and exits the metaphysis on the compression side (Salter-Harris type II).
Birth injury secondary to breech presentation or arthrogryposis may cause this physeal separation injury.
Minimal trauma in conditions that cause generalized weakening of the growth plate (osteomyelitis, leukemia, myelodysplasia) may also be causative.
Patients are typically unable to bear weight on the injured lower extremity, although patients with a nondisplaced physeal injury from a low-energy mechanism (e.g., athletic injury) may ambulate with an antalgic gait.
Older children and adolescents may relate a history of hearing or feeling a “pop” along with associated knee effusion and soft tissue swelling; this may be confused with a ligamentous injury.
The knee is typically in flexion owing to hamstring spasm.
Gross shortening or angular deformity is variable, with potential compromise of the neurovascular structures resulting from traction injury, laceration, or compression. A complete neurovascular assessment is thus critical.
Point tenderness may be elicited over the physis; this is usually performed by palpating the distal femur at the level of the superior pole of the patella and adductor tubercle.
Most commonly, epiphyseal displacement is in the coronal plane producing a varus or valgus deformity.
Anteroposterior (AP), lateral, and oblique views should be obtained. Radiographs of the contralateral lower extremity may be obtained for comparison if the diagnosis is in doubt.
Stress views may be obtained to diagnose nondisplaced separations in which the clinical examination is highly suggestive of physeal injury (knees with effusion and point tenderness over physis in the setting of a negative AP and lateral radiograph). Adequate
analgesia is necessary to relax muscular spasm and to prevent both false-negative stress radiographs and physeal injury.
The physeal line should be 3- to 5-mm thick until adolescence.
Salter-Harris type III injuries usually have vertically oriented epiphyseal fracture components that are best appreciated on an AP view.
Computed tomography may be useful to assess fracture fragment definition.
In infants, separation of the distal femoral physis may be difficult to assess unless there is gross displacement because only the center of the epiphysis is ossified at birth; this should be in line with the anatomic axis of the femur on both AP and lateral views. Magnetic resonance imaging, ultrasound, or arthrography may aid in the diagnosis of distal femoral injury in these patients.
Arteriography of the lower extremity should be pursued if vascular injury is suspected.
Knee dislocations are uncommon in the skeletally immature, whereas physeal separation of the distal femoral physis may be associated with vascular injury.
TABLE 49.1 Imaging Studies in the Evaluation of Distal Femoral Physeal Fractures | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||
This is indicated for nondisplaced fractures.
A tense knee joint effusion may be relieved by sterile aspiration for symptomatic relief.
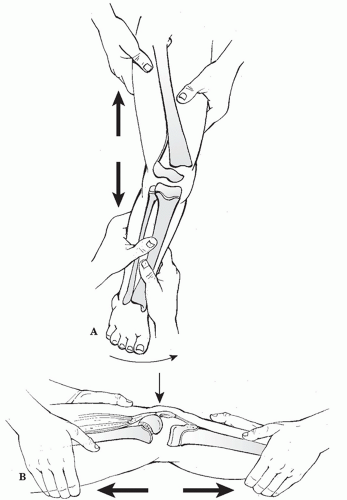
Closed reduction using general anesthesia may be performed for displaced fractures in which a stable result can be obtained (Fig. 49.2).
Sufficient traction should be applied during manipulation to minimize grinding of physeal cartilage (90% traction, 10% leverage). The position of immobilization varies with direction of displacement.
Medial/lateral: Immobilize in 15 to 20 degrees of knee flexion. Cast in valgus mold for medial metaphyseal fragment and varus mold for lateral metaphyseal fragment to tension intact periosteum.
Anterior: Immobilize initially at 90 degrees of knee flexion, then decrease flexion with time.
Posterior: Immobilize in extension.
A residual varus/valgus deformity after reduction tends not to remodel.
Crutch ambulation with toe-touch weight bearing may be instituted at 3 weeks after injury.
The cast may be discontinued at 4 to 8 weeks, depending on the patient’s age and healing status. A removable posterior splint and active range-of-motion exercises are instituted at this time.
Athletic activities should be restricted until knee range of motion has returned, symptoms have resolved, and sufficient quadriceps strength has been regained.
Indications for open reduction and internal fixation include:
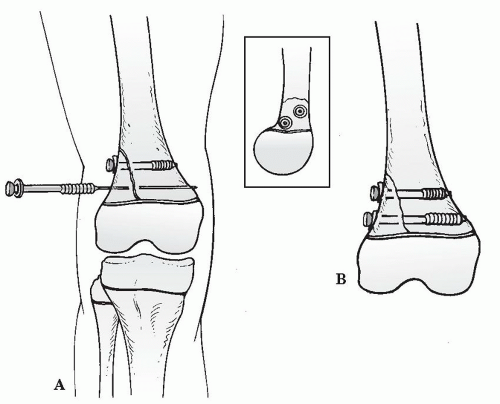
Irreducible Salter-Harris type II fracture with interposed soft tissue: Cannulated 4.0- or 6.5-mm screw fixation may be used to secure the metaphyseal spike (Fig. 49.3).
Unstable reduction is an indication.
Salter-Harris types III and IV: Joint congruity must be restored.
To minimize residual deformity and growth disturbance, specific principles should be observed for internal fixation.
Avoid crossing the physis if possible.
If the physis must be crossed, use smooth pins as perpendicular as possible to the physis.
Remove fixation that crosses the physis as soon as possible.
Postoperatively, the patient is maintained in a long leg cast in 10 degrees of knee flexion. The patient may be ambulatory with crutches in 1 to 2 days with non-weight bearing on the injured extremity. At 1 week, the patient may begin straight leg raises.
If at 4 weeks evidence of osseous healing is demonstrated radiographically, the cast may be discontinued with a posterior splint in place for protection. The patient may be advanced to partial weight bearing with active range-of-motion exercises.
The patient typically resumes a normal, active lifestyle at 4 to 6 months after injury.
Popliteal artery injury (<2%): Associated with hyperextension or anterior epiphyseal displacement injuries in which a traction injury may be sustained or by direct laceration from the sharp metaphyseal spike.
A cool, pulseless foot that persists despite reduction should be worked up with angiography to rule out laceration.
Vascular embarrassment that resolves following reduction should be observed for 48 to 72 hours to rule out an intimal tear and subsequent thrombosis.
Peroneal nerve palsy (3%): Caused by traction injury during fracture or reduction or secondary to initially anterior/medial displaced epiphysis. Persistent peroneal palsy over 3 to 6 months should be evaluated by electromyography and by exploration as may be indicated.
Recurrent displacement: Fractures of questionable stability following closed reduction should receive operative fixation (either percutaneous pins or internal fixation) to prevent late or recurrent displacement. Anterior and posterior displacements are particularly unstable.
Knee instability (up to 37% of patients): Knee instability may be present, indicating concomitant ligamentous compromise that was not appreciated at the time of index presentation. The patient may be treated with rehabilitation for lower extremity strengthening or may require operative treatment. Collateral ligaments may be acutely repaired if instability exists after fracture fixation.
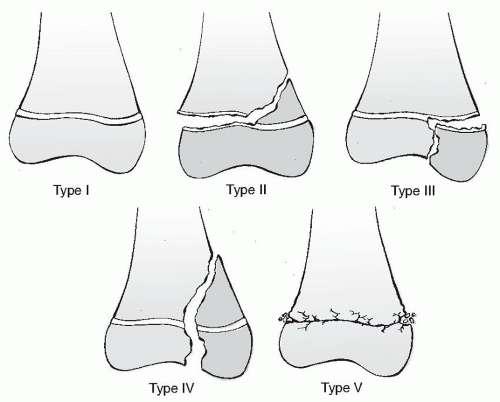
Angular deformity (19%): This results from the initial physeal injury (Salter-Harris types I and II), asymmetric physeal closure (bar formation, Salter-Harris types III and IV), or unrecognized physeal injury (Salter-Harris type V).
Observation, physeal bar excision (<30% of physis, >2 years of remaining growth), hemiepiphysiodesis, epiphyseolysis, or wedge osteotomy may be indicated.
Physeal closure is usually the rule for distal femoral physeal fractures. A resultant leg length discrepancy (24%) depends on the amount of remaining growth: This is usually clinically insignificant if <2 years of growth remain; otherwise, the discrepancy tends to progress at the rate of 1 cm per year.
Discrepancy <2.0 cm at skeletal maturity is usually of no functional or cosmetic significance.
Discrepancy of 2.5 to 5 cm may be treated with contralateral epiphysiodesis (femoral or tibial, or both) or femoral shortening depending on the projected length discrepancy.
Discrepancy >5 cm may be an indication for femoral lengthening combined with epiphysiodesis of the contralateral distal femur or proximal tibia.
Knee stiffness (16%): Results from adhesions or capsular or muscular contracture following surgery. It is usually related to the duration of immobilization; therefore, early discontinuation of the cast with active range of motion is desirable.
These comprise 0.6% to 0.8% of all physeal injuries.
The average age is 14 years.
Most occur in adolescent males.
The popliteal artery traverses the posterior aspect of the knee and is tethered to the knee capsule by connective tissue septa posterior to the proximal tibia. The vascular supply is derived from the anastomosis of the inferior geniculate arteries.
The physis is well protected by osseous and soft tissue structures, which may account for the low incidence of injuries to this structure.
Lateral: Fibula
Anterior: Patellar tendon/ligament
Medial: Medial collateral ligament (MCL; inserts into metaphysis)
Posteromedial: Semimembranosus insertion
Direct: Trauma to the proximal tibia (motor vehicle bumper, lawnmower accident)
Indirect: More common and involves hyperextension, abduction, or hyperflexion from athletic injury, motor vehicle accident, fall, or landing from a jump with a concurrent MCL tear
Birth injury: Results from hyperextension during breech delivery or arthrogryposis
Pathologic condition: Osteomyelitis of the proximal tibia and myelomeningocele are causes.
Patients typically present with an inability to bear weight on the injured extremity. The knee may be tense with hemarthrosis, and extension is limited by hamstring spasm.
Tenderness is present 1 to 1.5 cm distal to the joint line, and variable gross deformity may be present.
Neurovascular status should be carefully assessed for popliteal artery or peroneal nerve compromise. The anterior, lateral, superficial posterior, and deep posterior compartments should be palpated for pain or turgor. Patients suspected of having elevated compartment pressures should receive serial neurovascular examinations with measurement of compartment pressures as indicated.
Associated ligamentous injuries should be suspected, although it may be difficult to appreciate these injuries secondary to the dramatic presentation of the fracture.
AP, lateral, and oblique views of the affected knee should be obtained. Radiographs of the contralateral knee may be obtained for comparison.
Stress radiographs in coronal and sagittal planes may be obtained, but hyperextension of the knee should be avoided because of potential injury to popliteal structures.
Most patients with proximal tibial physeal injuries are adolescents in whom the secondary ossicle of the tibial tubercle has appeared. A smooth, horizontal radiolucency at the base of the tibial tubercle should not be confused with an epiphyseal fracture.
Magnetic resonance imaging may aid in identification of soft tissue interposition when reduction is difficult or impossible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree