Pediatric Hip
PEDIATRIC HIP FRACTURES
Epidemiology
Hip fractures are rare in children, occurring less than 1% as often as in adults.
Anatomy
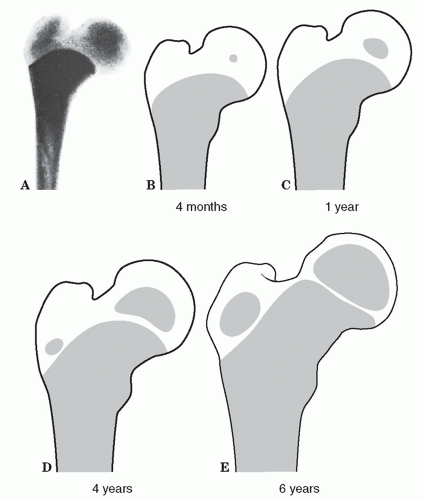
Ossification (Fig. 47.1)
Proximal femur: week 7 in utero
Proximal femoral epiphysis: ages 4 to 8 months
Trochanter: 4 years
The proximal femoral epiphysis fuses by age 18 years, the trochanteric apophysis by ages 16 to 18 years.
The proximal femoral physis contributes significantly to metaphyseal growth of the femoral neck and less to primary appositional growth of the femoral head. Thus, disruptions in this region may lead to architectural changes that may affect the overall anatomic development of the proximal femur.
The trochanteric apophysis contributes significantly to appositional growth of the greater trochanter and less to the metaphyseal growth of the femur.
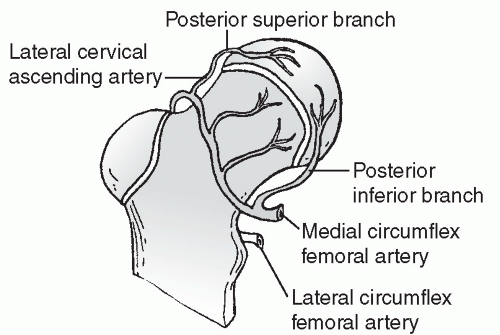
Blood is supplied to the hip by the lateral femoral circumflex artery and, more importantly, the medial femoral circumflex artery. Anastomoses at the anterosuperior portion of the intertrochanteric groove form the extracapsular ring. Ascending retinacular vessels go to the epiphysis (Fig. 47.2).
By 3 or 4 years of age, the lateral posterosuperior vessels (branches of the medial femoral circumflex) predominate and supply the entire anterolateral portion of the capital femoral epiphysis.
Vessels of the ligamentum teres contribute little before age 8 years and approximately 20% in adulthood.
Capsulotomy does not damage the blood supply to the femoral head, but violation of the intertrochanteric notch or the lateral ascending cervical vessels can render the femoral head avascular.
Mechanism of Injury
Axial loading, torsion, hyperabduction, or a direct blow can result in a hip fracture. Severe, direct trauma (e.g., motor vehicle accident) accounts for 75% to 80% of pediatric hip fractures.
Pathologic: Fracture occurs through bone cyst or fibrous dysplasia; tumors account for the remainder.
Stress fractures: These are uncommon.
Clinical Evaluation
The patient typically presents with a shortened and externally rotated lower extremity.
Range of hip motion is painful with variable crepitus.
Swelling, ecchymosis, and tenderness to palpation are generally present over the injured hip.
A careful neurovascular examination should be performed.
Radiographic Evaluation
Anteroposterior (AP) views of the pelvis and a cross-table lateral view of the affected hip should be obtained, with the leg extended and internally rotated as far as is tolerable by the patient.
Developmental coxa vara should not be confused with hip fracture, especially in patients <5 years of age. Comparison with the contralateral hip may aid in the distinction.
Computed tomography may aid in the diagnosis of nondisplaced fractures or stress fractures.
A radioisotope bone scan obtained 48 hours after injury may demonstrate increased uptake at the occult fracture site.
Magnetic resonance imaging may detect occult fractures within 24 hours of injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree