Pediatric Forearm
EPIDEMIOLOGY
These injuries are very common. They make up 40% of all pediatric fractures (only 4% are diaphyseal fractures), with a 3:1 male predominance in distal radius fractures.
Eighty percent occur in children >5 years of age.
The peak incidence corresponds to the peak velocity of growth when the bone is weakest owing to dissociation between bone growth and mineralization.
Fifteen percent have ipsilateral supracondylar fracture.
One percent have neurologic injury, most commonly median nerve.
Of pediatric forearm fractures, 60% occur in the distal metaphyses of the radius or ulna, 20% in the shaft, 14% in the distal physis, and <4% in the proximal third.
ANATOMY
The radial and ulnar shafts ossify during the eighth week of gestation.
The distal radial epiphysis appears at age 1 year (often from two centers); the distal ulnar epiphysis appears at age 5 years; the radial head appears at ages 5 to 7 years; the olecranon appears at ages 9 to 10 years. These all close between the ages of 16 and 18 years.
The distal physis accounts for 80% of forearm growth.
With advancing skeletal age, there is a tendency for fractures to occur in an increasingly distal location owing to the distal recession of the transition between the more vulnerable wider metaphysis and the narrower and stronger diaphysis.
Osteology
The radius is a curved bone, cylindric in the proximal third, triangular in the middle third, and flat distally with an apex lateral bow.
The ulna has a triangular shape throughout, with an apex posterior bow in the proximal third.
The proximal radioulnar joint is most stable in supination where the broadest part of the radial head contacts the radial notch of the ulna and the interosseous membrane is most taut. The annular ligament is its major soft tissue stabilizer.
The distal radioulnar joint (DRUJ) is stabilized by the ulnar collateral ligament, the anterior and posterior radioulnar ligaments, and the pronator quadratus muscle. Three percent of distal radius fractures have concomitant DRUJ disruption.
The triangular fibrocartilage complex (TFCC) has an articular disc joined by volar and dorsal radiocarpal ligaments and by ulnar collateral ligament fibers. It attaches to the distal radius at its ulnar margin, with its apex attached to the base of the ulna styloid, extending distally to the base of the fifth metacarpal.
The periosteum is very strong and thick in the child. It is generally disrupted on the convex fracture side, whereas an intact hinge remains on the concave side. This is an important consideration when attempting closed reduction.
Biomechanics
The posterior distal radioulnar ligament is taut in pronation, whereas the anterior ligament is taut in supination.
The radius effectively shortens with pronation and lengthens with supination.
The interosseous space is narrowest in pronation and widest in neutral to 30 degrees of supination. Further supination or pronation relaxes the membrane.
The average range of pronation/supination is 90/90 degrees (50/50 degrees necessary for activities of daily living).
Middle third deformity has a greater effect on supination, with the distal third affecting pronation to a greater degree.
Malreduction of 10 degrees in the middle third limits rotation by 20 to 30 degrees.
Bayonet apposition (overlapping) of the radius and ulna does not reduce forearm rotation.
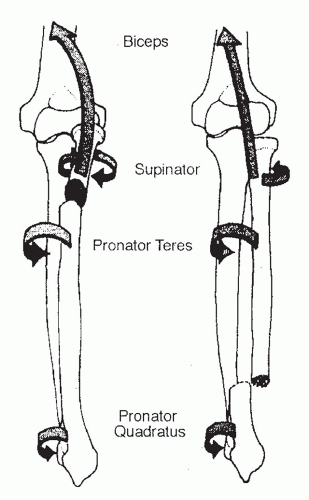
Deforming muscle forces (Fig. 45.1)
Proximal third fractures:
Biceps and supinator: These function to flex and supinate the proximal fragment.
Pronator teres and pronator quadratus: These pronate the distal fragment.
Middle third fractures:
Supinator, biceps, and pronator teres: The proximal fragment is in neutral.
Pronator quadratus: Pronates the distal fragment.
Distal third fractures:
Brachioradialis: Dorsiflexes and radially deviates the distal segment.
Pronator quadratus, wrist flexors and extensors, and thumb abductors: They also cause fracture deformity.
MECHANISM OF INJURY
Indirect: The mechanism is a fall onto an outstretched hand. Forearm rotation determines the direction of angulation:
Pronation: Flexion injury (dorsal angulation)
Supination: Extension injury (volar angulation)
Direct: Direct trauma to the radial or ulnar shaft.
CLINICAL EVALUATION
The patient typically presents with pain, swelling, variable gross deformity, and a refusal to use the injured upper extremity.
A careful neurovascular examination is essential. Injuries to the wrist may be accompanied by symptoms of carpal tunnel compression and more proximal fractures may be associated with anterior interosseous nerve (AIN) or posterior interosseous nerve (PIN) injuries.
The ipsilateral hand, wrist, forearm, and arm should be palpated, with examination of the ipsilateral elbow and shoulder to rule out associated fractures or dislocations.
In cases of dramatic swelling of the forearm, compartment syndrome should be ruled out on the basis of serial neurovascular examinations with compartment pressure monitoring if indicated. Pain on passive extension of the digits is most sensitive for recognition of a possible developing compartment syndrome; the presence of any of the “classic” signs of compartment syndrome (pain out of proportion to injury, pallor, paresthesias, pulselessness, paralysis) should be aggressively evaluated with possible forearm fasciotomy.
Examination of skin integrity must be performed, with removal of all bandages and splints placed in the field.
RADIOGRAPHIC EVALUATION
Anteroposterior and lateral views of forearm, wrist, and elbow should be obtained. The forearm should not be rotated to obtain these views; instead, the beam should be rotated to obtain a crosstable view.
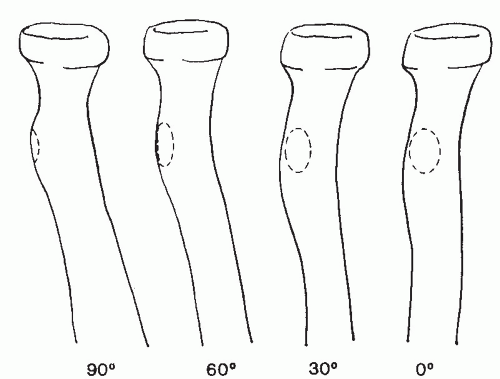
The bicipital tuberosity is the landmark for identifying the rotational position of the proximal fragment (Fig. 45.2):
Ninety degrees of supination: It is directed medially.
Neutral: It is directed posteriorly.
Ninety degrees of pronation: This is directed laterally.
In the normal, uninjured radius, the bicipital tuberosity is 180 degrees to the radial styloid.
RADIUS AND ULNA SHAFT FRACTURES
Classification
Descriptive
1. Location: Proximal, middle, distal third
2. Type: Plastic deformation, incomplete (greenstick), compression (torus or buckle), or complete
3. Displacement
4. Angulation
Nonoperative Treatment
Gross deformity should be corrected on presentation to limit injury to soft tissues. The extremity should be splinted for pain relief and for prevention of further injury if closed reduction will be delayed (Fig. 45.3).
The extent and type of fracture and the child’s age are factors that determine whether reduction can be carried out with sedation, local anesthesia, or general anesthesia.
Finger traps may be applied with weights to aid in reduction.
Closed reduction and application of a well-molded (both three-point and interosseous molds) long arm cast or splint should be performed for most fractures, unless the fracture is open, unstable, irreducible, or associated with compartment syndrome.
Reduction should be maintained with pressure on the side of the intact periosteum (concave side).
Exaggeration of the deformity to disengage the fragment and to relieve tension of the periosteum is only performed for distal radius fractures, not shaft fractures.
Because of deforming muscle forces, the level of the fracture determines forearm rotation of immobilization:
Proximal third fractures: Supination
Middle third fractures: Neutral
Distal third fractures: Pronation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree