Pediatric Foot
TALUS
Epidemiology
It is extremely rare in children (0.01% to 0.08% ofall pediatric fractures).
Most represent fractures through the talar neck.
Anatomy
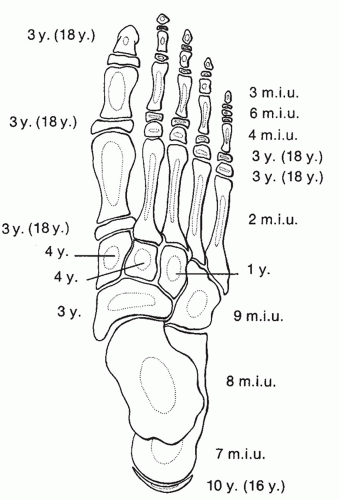
The ossification center of the talus appears at 8 months in utero (Fig. 52.1).
Two thirds of the talus is covered with articular cartilage.
The body of the talus is covered superiorly by the trochlear articular surface through which the body weight is transmitted. The anterior aspect is wider than the posterior aspect, which confers intrinsic stability to the ankle.
Arterial supply to the talus is from two main sources:
Artery to the tarsal canal: This arises from the posterior tibial artery 1 cm proximal to the origin of the medial and lateral plantar arteries. It gives off a deltoid branch immediately after its origin that anastomoses with branches from the dorsalis pedis over the talar neck.
Artery of the tarsal sinus: This originates from the anastomotic loop of the perforating peroneal and lateral tarsal branches of the dorsalis pedis artery.
An os trigonum is present in up to 50% of normal feet. It arises from a separate ossification center just posterior to the lateral tubercle of the posterior talar process.
Mechanism of Injury
Forced dorsiflexion of the ankle from motor vehicle accident or fall represents the most common mechanism of injury in children. This typically results in a fracture of the talar neck.
Isolated fractures of the talar dome and body have been described but are extremely rare.
Clinical Evaluation
Patients typically present with pain on weight bearing on the affected extremity.
Ankle range of motion is typically painful, especially with dorsiflexion, and may elicit crepitus.
Diffuse swelling of the hindfoot may be present, with tenderness to palpation of the talus and subtalar joint.
A neurovascular examination should be performed.
Radiographic Evaluation
Standard anteroposterior (AP), mortise, and lateral radiographs of the ankle should be obtained, as well as AP, lateral, and oblique views of the foot.
Computed tomographic (CT) scanning may be useful for preoperative planning.
Magnetic resonance imaging (MRI) may be used to identify occult injuries in children <10 years old owing to limited ossification at this age.
Classification
Descriptive
Location: Most talar fractures in children occur through the talar neck.
Angulation: Usually varus
Displacement: in millimeters
Dislocation: Subtalar, talonavicular, or ankle joints
Pattern: Presence of comminution
Hawkins Talar Neck Fractures
This classification is for adults, but it is often used for children.
Type I: Nondisplaced
Type II: Displaced with associated subtalar subluxation or dislocation
Type III: Displaced with associated subtalar and ankle dislocation
Type IV: Type III with associated talonavicular subluxation or dislocation
See Chapter 40 for figures.
Treatment
Nonoperative
Nondisplaced fractures may be managed in a long leg cast with the knee flexed 30 degrees to prevent weight bearing. This is maintained for 6 to 8 weeks with serial radiographs to assess healing status. The patient may then be advanced to weight bearing in a short leg walking cast for an additional 2 to 3 weeks.
Operative
This is indicated for displaced fractures.
Minimally displaced fractures can often be treated successfully with closed reduction with plantar flexion of the forefoot as well as hindfoot eversion or inversion, depending on the displacement.
Displaced fractures are usually amenable to internal fixation using a posterolateral approach and 3.5-mm or 4.0-mm cannulated screws or Kirschner wires placed from a posterior to anterior direction. In this manner, dissection around the talar neck is avoided.
Postoperatively, the patient is maintained in a short leg cast for 6 to 8 weeks, with removal of wires at 3 to 4 weeks.
Complications
Osteonecrosis: This may occur with disruption or thrombosis of the tenuous vascular supply to the talus. This is related to the initial degree of displacement and angulation and, theoretically, the time until fracture reduction. It tends to occur within 6 months of injury.
Hawkins sign represents subchondral osteopenia in the vascularized, non-weight-bearing talus at 6 to 8 weeks. Although this tends to indicate talar viability, the presence of this sign does not rule out osteonecrosis.
Type I fractures: 0% to 27% incidence of osteonecrosis reported
Type II fractures: 42% incidence
Type III, IV fractures: >90% incidence
CALCANEUS
Epidemiology
This is a rare injury (less than 2%), typically involving older children (>9 years) and adolescents.
Most are extra-articular, involving the apophysis or tuberosity. Most occur secondary to a fall from height.
Of these, 33% are associated with other injuries, including lumbar vertebral and ipsilateral lower extremity injuries.
Anatomy
The primary ossification center appears at 7 months in utero; a secondary ossification center appears at age 10 years and fuses by age 16 years.
The calcaneal fracture patterns in children differ from that of adults, primarily for three reasons:
1. The lateral process, which is responsible for calcaneal impaction resulting in joint depression injury in adults, is diminutive in the immature calcaneus.
2. The posterior facet is parallel to the ground, rather than inclined as it is in adults.
3. In children, the calcaneus is composed of an ossific nucleus surrounded by cartilage, which is responsible for the dissipation of the injurious forces that produce classic fracture patterns in adults.
Mechanism of Injury
Most calcaneal fractures occur as a result of a fall or a jump from a height, although typically a lower energy injury occurs than seen with adult fractures.
Open fractures may result from lawn mower injuries.
Clinical Evaluation
Patients are typically unable to walk secondary to hindfoot pain.
On physical examination, pain, swelling, and tenderness can usually be appreciated at the site of injury.
Examination of the ipsilateral lower extremity and lumbar spine is essential, because associated injuries are common.
A careful neurovascular examination should be performed.
Injury is initially missed in 44% to 55% of cases.
Radiographic Evaluation
Dorsoplantar, lateral, axial, and lateral oblique views should be obtained for evaluation of pediatric calcaneal fractures.
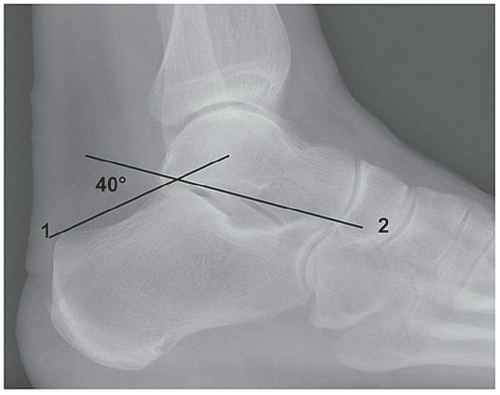
The Böhler tuber joint angle: This is represented by the intersection of two lines: a line from the highest point of the anterior process of the calcaneus to the highest point of the posterior articular surface and a line drawn between the same point on the posterior articular surface and the most superior point of the tuberosity. Normally, this angle is between 25 and 40 degrees; flattening of this angle indicates collapse of the posterior facet (Fig. 52.2).
Comparison views of the contralateral foot may help detect subtle changes in the Böhler angle.
Technetium bone scanning may be utilized when calcaneal fracture is suspected but is not appreciated on standard radiographs.
Computed tomography may aid in fracture definition, particularly in intra-articular fractures in which preoperative planning may be facilitated by three-dimensional characterization of fragments.
Classification
Schmidt and Weiner (Fig. 52.3)
Type I: A. Fracture of the tuberosity or apophysis
B. Fracture of the sustentaculum
C. Fracture of the anterior process
D. Fracture of the anterior inferolateral process
E. Avulsion fracture of the body
 Get Clinical Tree app for offline access 
|