Pediatric Femoral Shaft
EPIDEMIOLOGY
Represent 1.6% of all fractures in the pediatric population.
Males are more commonly affected at a ratio of 2.6:1.
Bimodal distribution of incidence: The first peak is from 2 to 4 years of age, and the second is in mid-adolescence.
There is also a seasonal distribution, with a higher incidence during the summer months.
In children younger than walking age, 80% are caused by child abuse; this decreases to 30% in toddlers.
In adolescence, >90% of femoral fractures are caused by motor vehicle accidents.
ANATOMY
During childhood, remodeling in the femur causes a change from primarily weaker woven bone to stronger lamellar bone.
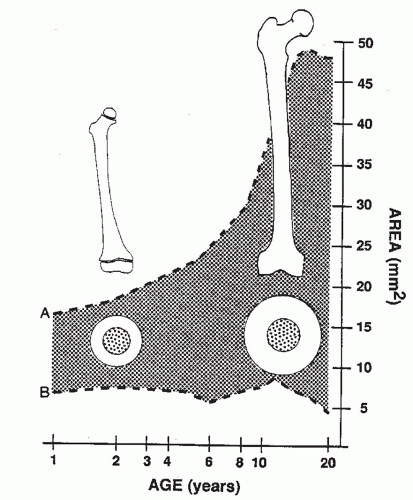
Up to age 16 years, there is a geometric increase in the femoral shaft diameter and relative cortical thickness of the femur, resulting in a markedly increased area moment of inertia and strength. This partially explains the bimodal distribution of injury pattern, in which younger patients experience fractures under load conditions reached in normal play or minor trauma, whereas in adolescence, highenergy trauma is required to reach the stresses necessary for fracture (Fig. 48.1).
MECHANISM OF INJURY
Direct trauma: Causes include motor vehicle accidents, pedestrian injury, fall, and child abuse.
Indirect trauma: The cause is rotational injury.
CLINICAL EVALUATION
Patients with a history of high-energy injury should undergo full trauma evaluation as indicated.
The presence of a femoral shaft fracture results in an inability to ambulate, with extreme pain, variable swelling, and variable gross deformity. The diagnosis is more difficult in patients with multiple trauma or head injury or in nonambulatory, severely disabled children.
A careful neurovascular examination is essential.
Splints or bandages placed in the field must be removed with a careful examination of the overlying soft tissues to rule out the possibility of an open fracture.
Hypotension from an isolated femoral shaft fracture is uncommon. The Waddell triad of head injury, intra-abdominal or intrathoracic trauma, and femoral shaft fracture is strongly associated with vehicular trauma and is a more likely cause of volume loss. However, the presence of a severely swollen thigh may indicate large volume loss into muscle compartments surrounding the fracture.
Compartment syndrome is rare and occurs only with severe hemorrhage into thigh compartments.
The ipsilateral hip and knee should be examined for associated injuries.
RADIOGRAPHIC EVALUATION
Anteroposterior and lateral views of the femur should be obtained.
Radiographs of the hip and knee should be obtained to rule out associated injuries; intertrochanteric fractures, femoral neck fractures, hip dislocation, physeal injuries to the distal femur, ligamentous disruptions, meniscal tears, and tibial fractures have all been described in association with femoral shaft fractures.
Magnetic resonance imaging (MRI) or computed tomography (CT) scans are generally unnecessary but may aid in the diagnosis of otherwise occult nondisplaced, buckle, or stress fractures.
CLASSIFICATION
Descriptive
Open versus closed
Level of fracture: proximal, middle, distal third
Fracture pattern: transverse, spiral, oblique, butterfly fragment
Comminution
Displacement
Angulation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree