Pediatric Ankle
EPIDEMIOLOGY
Ankle injuries account for up to 18% of all physeal injuries; they are third in frequency following phalangeal and distal radius physeal injuries.
Fifty-eight percent of ankle physeal injuries occur during athletic participation.
They represent 10% to 40% of all injuries in skeletally immature athletes.
Tibial physeal fractures are most common from 8 to 15 years of age.
Fibular physeal injuries are most common from 8 to 14 years of age.
Ligamentous injuries are rare in children because their ligaments are stronger relative to the physis.
After age 15 to 16 years, see adult fracture pattern.
ANATOMY
The ankle is a modified hinge joint stabilized by medial and lateral ligamentous complexes. All ligaments attach distal to the physes of the tibia and fibula—important in the pathoanatomy of pediatric ankle fracture patterns.
The distal tibial ossific nucleus appears between the ages of 6 and 24 months; it fuses with the tibial shaft at about age 15 years in girls and 17 years in boys. Over an 18-month period, the lateral portion of the distal tibial physis remains open while the medial part has closed.
The distal fibular ossific nucleus appears at the age of 9 to 24 months and unites with the fibula shaft 12 to 24 months after tibial physis closure.
Secondary ossification centers occur and can be confused with a fracture of either the medial or lateral malleolus; they are often bilateral.
The unique fracture patterns occur with the fusion of tibial physis from central to anteromedial to posteromedial and finally to lateral.
MECHANISM OF INJURY
Direct: Trauma to the ankle from a fall, motor vehicle accident, or pedestrian-motor vehicle accident.
Indirect: Axial force transmission through the forefoot and hindfoot or rotational force of the body on a planted foot; it may be secondary to a fall or, more commonly, athletic participation.
CLINICAL EVALUATION
Patients with displaced ankle fractures typically present with pain and gross deformity, as well as an inability to ambulate.
Physical examination may demonstrate tenderness, swelling, and ecchymosis.
Ligamentous instability may be present, but it is usually difficult to elicit on presentation owing to pain and swelling from the acute injury.
Ankle sprains are a diagnosis of exclusion and should be differentiated from a nondisplaced fracture based on the location of tenderness.
Neurovascular examination is essential, with documentation of dorsalis pedis and posterior tibial pulses, capillary refill, sensation to light touch and pinprick, and motor testing.
Dressings and splints placed in the field should be removed and soft tissue conditions assessed, with attention to skin lacerations that may indicate open fracture or fracture blisters that may compromise wound healing.
The ipsilateral foot, leg, and knee should be examined for concomitant injury.
RADIOGRAPHIC EVALUATION
Anteroposterior (AP), lateral, and mortise views of the ankle should be obtained. Tenderness of the proximal fibula warrants appropriate views of the leg.
Clinical examination will dictate the possible indication for obtaining views of the knee and foot.
Stress views of the ankle may be obtained to determine possible undisplaced transphyseal fractures.
The presence of secondary ossification centers (a medial os subtibiale in 20% of patients or a lateral os subfibulare in 1% of patients) should not be confused with fracture, although tenderness may indicate injury.
A Tillaux fragment represents an osseous fragment from the lateral distal tibia that has been avulsed during injury.
Computed tomography (CT) is often helpful for evaluation of complex intra-articular fractures, such as the juvenile Tillaux or triplane fracture.
Magnetic resonance imaging has been used to delineate osteochondral injuries in association with ankle fractures.
CLASSIFICATION
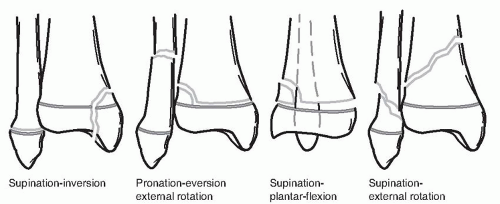
Dias and Tachdjian
Lauge-Hansen principles are followed, incorporating the Salter-Harris classification.
The typology is simplified by noting the direction of physeal displacement, Salter-Harris type, and location of the metaphyseal fragment.
The classification aids in determining the proper maneuver for closed reduction (Fig. 51.1).
Supination-External Rotation (SER)
Stage I: Salter-Harris type II fracture of the distal tibia with the metaphyseal fragment located posterolaterally; the distal fragment is displaced posteriorly, but the Thurston-Holland fragment is seen on the AP x-ray, which differentiates it from a supination-plantar flexion (SPF) injury.
Stage II: As external rotation force continues, a spiral fracture of the fibula occurs beginning medially and extending posterosuperiorly; it differs from an adult SER injury.
Pronation-Eversion-External Rotation (PEER)
This type comprises 15% to 20% of pediatric ankle fractures.
Marked valgus deformity occurs.
Tibial and fibular fractures occur simultaneously.
Salter-Harris type II fracture of the distal tibial physis is most commonly seen, but type I also occurs; the metaphyseal fragment is located laterally.
The short oblique distal fibular fracture occurs 4 to 7 cm proximal to the fibula tip.
 Get Clinical Tree app for offline access 
|








