Bone is a living, well-organised, vascular form of connective tissue. It is largely composed of an organic protein, collagen, and an inorganic mineral, hydroxyapatite, which combine to provide a mechanical and supportive role in the body (Smith et al. 1983). Bone is a dynamic tissue that requires stress for normal development. The capacity of bone to adapt its structure to imposed loads has become known as Wolff’s Law:
Wolff’s law:
“states that bone responds to the stresses that are imposed upon it by rearranging its initial architecture in the best way to withstand stress (Porter 2008)
Bones function as:
- Protectors of vital organs – provides mechanical protection for most of the body’s internal organs, thereby reducing the risk of injury to them
- Supportive structures – the skeleton is the framework of the body it provides attachment for skeletal muscles
- Levers – the skeleton assists with movement
- Reservoirs for calcium and phosphorus – storage for minerals (calcium and phosphorus), which are released when needed into the blood
- Blood producing cells – develops red blood cells in the bone marrow.
Bone structure
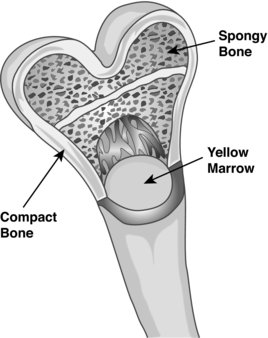
There are primarily three types of bone, namely: woven, compact and cancellous (Figure 7.2).
Woven bone
Woven bone is normally remodelled and replaced with either compact or cancellous bone. Woven bone is found during embryonic development, during fracture healing (callus formation), and in some pathological states, such as hyperparathyroidism and Padget Disease (Recker et al. 1992).
Compact bone
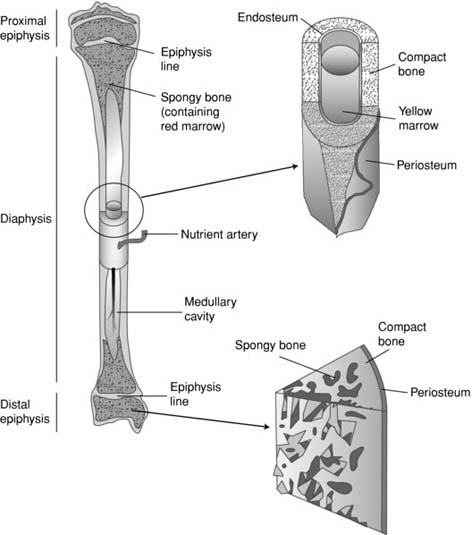
Compact bone is the outer structure and provides mechanical strength, while cancellous bone forms the inner structure and its function is the metabolic unit of the bone (Figure 7.3). Compact bone is dense bone and surrounds the cancellous bone. The primary structural unit of compact bone is an osteon, which is also known as a Haversian system. Osteons consist of cylindrical shaped lamellar bone that surrounds longitudinally oriented vascular channels called Haverisan canals; horizontally oriented vascular channels, which are known as Volkmann canals, connect adjacent osteons.
Cancellous bone
Cancellous (spongy) bone consists of spicules of bone enclosing cavities containing marrow (blood-forming cells). This type of bone is strong but the spaces make it light and flexible. Cancellous bone is always covered and therefore protected by compact bone. In long bones, cancellous bone is found in the epiphysis (at the end of the long bone); in some it also extends down inside into the shaft. In all other bones, it forms the central mass of bone within a compact bone lining.
In adults, 80% of the skeleton is compact bone. However, the relative proportions of compact and cancellous bone vary in different parts of the skeleton. For example, in the lumbar spine, cancellous bone accounts for about 70% of the total bone tissue, whereas in the femoral neck and radial diaphysis, it accounts for about 50% and 5%, respectively (Kanis 1994; Einhorn 1996; Fleisch 1997).
Bone covering
The periosteum is a membrane that lines the outer surface of all bones, (Netter 1987) except in the area of a joint where articular cartilage is present. It consists of dense irregular connective tissue. The periosteum is divided into a fibrous layer (outer) and an oseogenic layer (inner). The fibrous layer contains fibroblasts, while the oseogenic layer contains progenitor cells that develop into osteoblasts, which are cells that form and repair bones. The periosteum has nociceptors nerve endings present and is sensitive to injury. It also provides nourishment by providing the blood supply. It is attached to bone by strong collagenous fibres called Sharpey’s fibres, which extend to the outer circumferential and interstitial lamellae. It also provides an attachment for muscles and tendons. Bone, including the marrow, periosteum, metaphysic, diaphysis and epiphysis are richly supplied with blood vessels. Studies by Shim et al. (1967) and Tothill and MacPherson (1986) reported that approximately 7% of the cardiac output is sent to the skeleton.
Classification of bones
Bones are usually classified according to their shape. Table 7.1 summarises the main categories of bones.
Table 7.1 Categorisation of bones
| Type of bone | Function |
| Long bones | This type of bone functions as a lever They have greater length than width and consist of a shaft and a variable number of endings (extremities) They are usually somewhat curved for strength Examples include femur, tibia, fibula, humerus, ulna and radius |
| Flat bones | This type of bone has a broad surface for muscle attachment and is used for the protection of underlying organs Examples include cranial bones (protecting the brain), the sternum and ribs (protecting the organs in the thorax), and the scapulae. |
| Sesamoid bones | This type of bone develops in some tendons in locations where there is considerable friction, tension and physical stress. However their presence and quantity varies considerably from person to person Examples include patellae and under 1st metatarsal |
| Irregular bones | This type of bone has complicated shapes and so cannot be classified into any of the above (shape-based) categories. Their shapes are due to the functions they fulfil within the body e.g. providing major mechanical support for the body yet also protecting the spinal cord (in the case of the vertebrae) Examples include the vertebrae and some facial bones |
| Short bones | These types of bone are roughly cube-shaped and have approximately equal length and width Examples include ankle and wrist bones |
Bone formation and growth
Ossification is the name given to the formation of bone. There are three cells involved in bone metabolism:
1. Osteoblasts (bone forming cells) – mononuclear cells of mesenchymal origin.
2. Osteoclasts (bone eating cells).
3. Osteocytes (cells of the matrix) – found in mature adult bone.
Signalling pathways between these cells help regulate the balance between bone formation and bone reabsorption.
Osteoblasts are the bone-forming cells and they originate from local mesenchymal stem cells (bone marrow stroma or connective tissue mesenchyme). These stem cells undergo proliferation and differentiate to preosteoblasts and then to mature osteoblasts (Triffitt 1996). The plasma membrane of osteoblasts is rich in alkaline phosphatase, which enters the systemic circulation. The plasma concentration of this enzyme is used as a biochemical marker of bone formation. Osteocytes originate from osteoblasts embedded in the organic bone matrix, which subsequently become mineralised. They have numerous cell processes forming a network of thin canaliculi that connects them with active osteoblasts and flat lining cells. Osteocytes probably play a role in the homeostasis of this extracellular fluid and in the local activation of bone formation and/or resorption in response to mechanical loads (Nijweide et al. 1996).
Osteoclasts are giant cells containing 4–20 nuclei that reabsorb bone. Osteoclastic reabsorption takes place at the cell/bone interface in a sealed-off microenvironment (Baron 1996; Teitelbaum et al., 1996). The mechanism of bone resorption involves the secretion of hydrogen ions and proteolytic enzymes into the sub-osteoclastic resorbing compartment. The hydrogen ions dissolve the bone minerals, thereby exposing the organic matrix to the proteolytic enzymes (Baron 1996; Teitelbaum et al., 1996). These enzymes, which include collagenases and cathepsins, are responsible for the breakdown of the organic matrix.
Bone metabolism is under constant regulation by a host of hormonal and local factors. Three of the calcitropic hormones that most effect bone metabolism are parathyroid hormone, vitamin D and calcitonin (Table 7.2).
Table 7.2 Hormones that most effect bone metabolism
| Hormone | Description |
| Parathyroid hormone | Produced via the parathyroid glands, which are small endocrine glands in the neck Humans have four parathyroid glands, which are usually located behind the thyroid gland Increases the flow of calcium into the calcium pool Maintains body’s extracellular calcium pool level at a relatively constant level Osteoblasts are the only cells that have parathyroid hormone receptors Parathyroid hormone has antagonistic effects to those of calcitonin. |
| Vitamin D | Fat soluble molecule Stimulates intestinal and renal calcium binding proteins and facilitates active calcium transport Inhibits parathyroid hormone secretion |
| Calcitonin | Serves to inhibit calcium dependent cellular metabolic activity |
Cartilage
Cartilage is a non-vascular connective tissue that is divided, according to its minute structure, into:
- hyaline cartilage (articular) – covers joint surfaces
- fibrocartilage – knee meniscus, vertebral discs
- elastic cartilage – outer ear
These different forms of cartilage are distinguished by their structure, elasticity, and strength.
In general, cartilage is a tough, fibrous and blood vessel-free connective tissue that forms flexible linkages, supporting structures and acts as a shock absorber in joints such as the knee.
Hyaline (articular) cartilage is the most common type of cartilage. In addition to being found in articulated joints, hyaline cartilage forms the majority of the skeleton of a fetus. Later in fetal development, it is replaced by bone. The free surfaces of most hyaline cartilage (except that found in joints) are covered by a layer of fibrous connective tissue known as perichondrium. The perichondrium is rich in a type of cell known as the fibroblast. Compositionally, hyaline cartilage is made of water (75% by weight), collagen (10% by weight, mainly collagen type II), with the remainder being non-fibrous material, such as chondroitin sulphate and keratan sulphate. The collagen provides strength and makes hyaline cartilage resistant to compression. Also, the collagen provides a means by which the cartilage can be anchored to bone.
Cartilage is a metabolically active tissue that under normal conditions is maintained in a relatively slow state of turnover by a sparse population of chondrocytes distributed throughout the tissue (Naujok et al. 2008).
Common cartilage injuries
It is well known that lesions which are confined to the hyaline cartilage alone have little or no capacity to heal (Naujoks et al. 2008). In general, the individual becomes symptomatic and a significant progression to osteoarthritis is possible (Lohmander 2003).
Osteoarthritis (OA) is the most common form of arthritis, which is a leading cause of physical disability, increased healthcare usage and impaired quality of life (Felson 1990; Guccione et al. 1994). The term OA also applies particularly to the degeneration and excessive wear of cartilage. This condition develops and progresses with an increase in age. Epidemiological studies have demonstrated that participation in certain competitive sports increase the risk for OA (Kujala et al. 1994; Buckwalter and Lane 1997). Moderate regular running has low, if any risk leading to OA (Lane et al. 1993; Newton et al. 1997). Sport activities that appear to increase the risk for OA include those that demand high-intensity, acute, direct joint impact as a result of contact with other participants, playing surfaces or equipment (Buckwalter and Lane 1997).
Common skeletal injuries and their manifestation
As previously stated bone provides structural support and protection, facilitating movement and mineral storage. Therefore, injuries to bone can compromise any of these functions and interrupt daily functions.
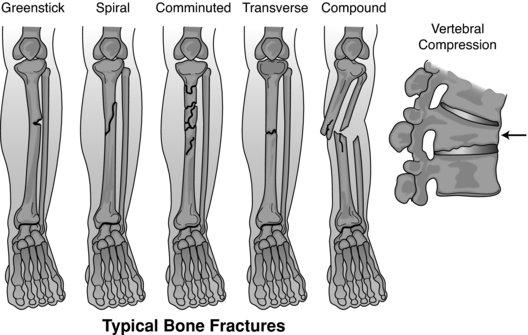
Bone fractures
Fractures are potentially serious injuries, damaging not only the bone but also the soft tissue in the surrounding area (diagram of types of fractures are illustrated in Figure 7.4) (Table 7.3). Although the bone tissue itself contains no nociceptors, bone fracture can be very painful, due to (1) the breaking in the continuity of the periosteum; (2) oedema of nearby soft tissues, caused by bleeding of torn periosteal blood vessels, evoking pressure pain; and (3) spasms in muscles trying to hold bone fragments in place.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree