Chapter 25 Pathogenesis of Chronic Elbow Instability
Introduction
The elbow is a trocho-gynglymoid joint with rotatory and hinge movement. The joint consists of articulations between the humerus, ulna and radius. The humero-ulnar joint is a functional hinge with high congruency between the deep trochlea of the humerus and the greater sigmoid notch of the ulna. This allows flexion and extension movement of the forearm relative to the humerus. In addition, the humeroradial joint and the proximal radio-ulnar joint allow rotational or pivoting movements of the forearm. The top of the radial head, with its concavity, and the spherical capitellum articulate with concavity compression that is further constrained by the annular ligament (AL) that surrounds the radial head. This anatomical complex construction is described in detail in Chapter 2.
Due to this inherently stable bony construction that is further enhanced by strong ligaments, chronic and recurrent instability of the elbow joint was for many years believed to be unusual. Reports of recurrent elbow instability were sparse, and mostly consisted of case studies that were associated with novel surgical techniques for elbow joint restabilization.1
Osborne and Cotteril were the first authors to focus on the lateral/radial collateral ligament injury as the key injury in elbow joint dislocations, and they reported a surgical reconstruction of the lateral joint capsule that prevented recurrent dislocation of the elbow joint.1
Presentation and investigations
In the 1980s and 1990s increasing interest in clinical elbow problems led to a number of publications on clinical and in vitro examinations of elbow joint stability. Many of these papers investigated different components of the elbow joint and their relative influence on preserving elbow joint stability. This led to a more detailed understanding of the different constraining joint structures of the elbow, and a definition of the so-called primary, secondary and tertiary stabilizers. The primary stabilizers were defined as structures that following injury caused immediate instability or in vitro laxity to the elbow joint, whereas secondary or tertiary stabilizers only gave increased instability or laxity in combination with injury to the primary or other stabilizers.2,3
The most recent papers have focused on the more clinically relevant combinations of injury that can, for example, be the result of an elbow fracture–dislocation, and the destabilizing influence that this has on the elbow.4
This work has improved our understanding of elbow stability and has identified that with instability symptoms of pain, limited motion, recurrent dislocations, chronic dislocation and in some cases a sensation that the joint is unstable will be reported by the patient.5
Different pathologies can cause elbow joint instability. These include acute dislocation of the elbow joint, a simple elbow joint distortion and intra-articular elbow fractures with or without joint dislocation. Surgically induced injury to the collateral ligaments will also cause instability, as will chronic diseases such as rheumatoid arthritis and malignancies that affect the elbow joint and cause instability through either articular joint side destruction and/or destruction of the soft tissues, leading to immediate loss of the inherent joint constraint.5
Aetiology of elbow instability
Soft tissues
Muscles
Recent experimental elbow models have shown a tendency to reduce the immediate elbow joint laxity that occurs following ligament divisions with simultaneous loading of the muscle tendons. This is in contrast to the passive stabilizing effect of the muscular tendons that only have a minor effect on stability.6,7 The in vivo contribution from these factors to the static joint constraints of ligaments and bone is still unknown, though in the clinical setting a muscular hypotonia following a dislocation has been observed. It has been speculated that this might increase immediate joint instability.8 Furthermore, it has been demonstrated that the flexor and extensor origins that lie in direct intimate continuity with the ulnar and radial collateral ligament complexes, respectively, can be avulsed or ruptured together with the ligaments when the elbow joint dislocates.9
Elbow joint capsule
The posterior capsule is usually a thin transparent membrane, whereas the anterior capsule has significant transverse and obliquely directed bands that blend intimately with the AL and the ulnar and radial collateral ligaments (Fig. 25.1).
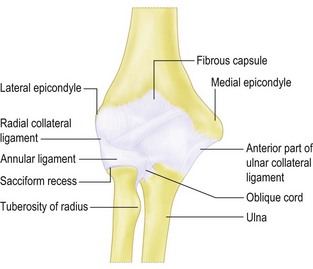
Figure 25.1 There is a cruciate orientation of the fibres of the anterior capsule that might provide some strength.
Morrey and Sanchez Sotello. The elbow and its disorders. 4th edn. 2008, Fig. 2-23, p. 20. Redrawn from Langmann J, Woerdeman MW. Atlas of medical anatomy. Philadelphia, PA: WB Saunders Co 1978.
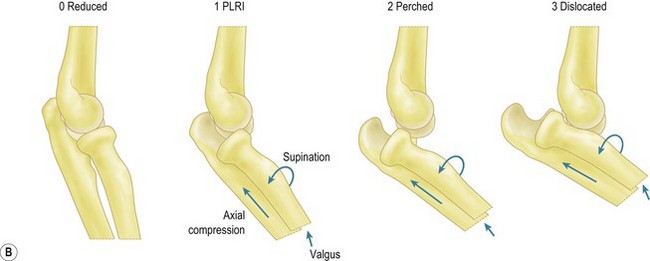
Both the posterior and anterior capsule have been reported to be torn following an elbow joint dislocation.10 Originally the strong anterior capsule was believed to possess a certain restraint to valgus and varus stress in extension, as well as a certain restraint to joint distraction.11 We have examined the elbow joint kinematics following isolated excision of the anterior and the posterior capsular tissue, with preservation of the ligaments. No laxity to forced valgus, varus or rotation was observed, other than what was induced by puncturing the joint, and removing the inherent negative intra-articular pressure and its immediate stabilizing effect.12 In this set-up, however, no data were reported in full elbow joint extension.12 In another study we found a primary but minor stabilizing effect of the anterior capsule to varus and external rotation in full elbow joint extension.13 More recently, in a study on experimental posterior elbow dislocation, we observed that in full extension the stabilizing influence of the capsule to forced external rotation actually exceeded that of the lateral collateral ligament (LCL) (Fig. 25.2).14 O’Driscoll showed that capsular resection associated with LCL injury was necessary to bring the elbow joint into the so-called perched position, indicating that some kind of secondary stabilizing effect of capsular tissue does exist (Fig. 25.3).10
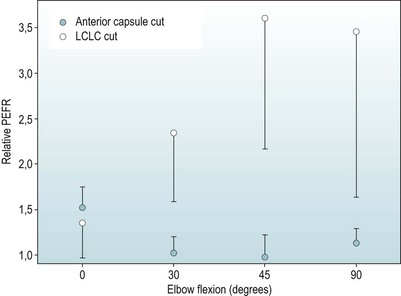
Redrawn from Deutch SR, Olsen BS, Jensen SL, et al. Ligamentous and capsular restraints to experimental posterior elbow joint dislocation. Scand J Med Sci Sports 2003; 13:311–316 (Fig. 5).
Ligaments
The elbow has two strong stabilizing ligament complexes: the medial collateral ligament complex (MCL) (Fig. 25.4) and the lateral collateral ligament complex (LCLC) (Fig. 25.5). In the literature MCL injury is reported to result from chronic tears due to repetitive valgus trauma associated with overhead throwing or hyperextension injury to the elbow. In contrast, LCLC injury is due to acute trauma that implies forced external rotation of the elbow with or without elbow joint dislocation. Clinically, a bilateral ligament injury is documented in clinical situations with elbow joint dislocations.9
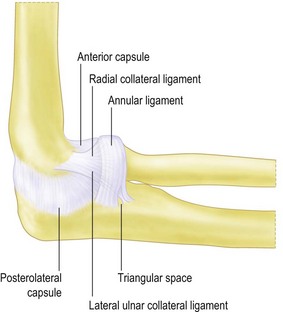
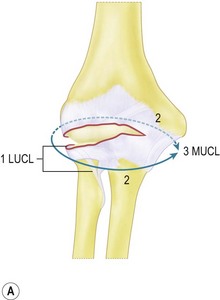
Figure 25.5 The anatomy of the lateral collateral ligament complex.
Redrawn from Olsen BS, Vaesel MT, Søjbjerg JO, et al. Lateral collateral ligament of the elbow joint: anatomy and kinematics. J Shoulder Elbow Surg 1996; 5:103–112 (Fig. 2).
Experimentally the circle concept of ligamentous damage in elbow joint subluxation and dislocation describes the different stages in an elbow joint dislocation and the immediate ligamentous damage that occurs (Fig. 25.3).10
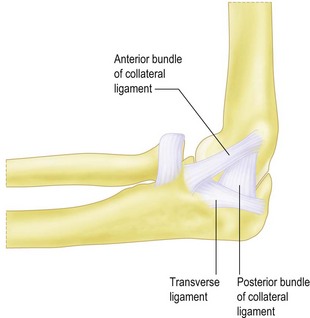
The medial collateral ligament complex
The MCL (Fig. 25.4) is divided into an anterior bundle, posterior bundle and transverse ligament. The anterior bundle extends from the undersurface of the medial epicondyle and inserts on the medial side of the coronoid process. It is the most prominent structure in the complex, and is described as the strongest ligament, with a mean load to failure of 260 N.15 We have described different bands in the anterior bundle.3 Failure, however, to define a reproducible guide to the separation of these bands has led to a common understanding that this ligament structure is a continuum of fibres that induces constraint with increasing joint flexion from anterior to posterior.3,15–17
The posterior bundle is a fan-shaped thickening of the capsule somewhat thinner than the anterior bundle. It extends from the medial epicondyle and inserts on the medial side of the olecranon. It has been reported as a capsular thickening rather than a distinct ligament.3,16
The transverse ligament spans the area between the medial tip of the olecranon and the medial side of the coronoid process. It is difficult to distinguish this structure from the capsular tissue. At the present time there is no evidence that this structure confers any elbow stability.16
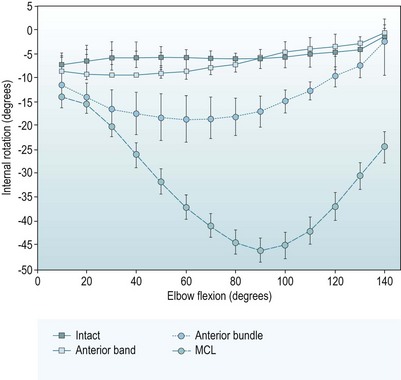
Different studies have reported on the stability provided by the MCL.2,3,10,11,14–18 We have performed an extensive kinematic examination of this ligament complex with intact osseous joint architecture.3 The study showed a significant increase in laxity to forced valgus and internal rotation of the elbow joint following excision of the entire anterior bundle. The maximal laxity to forced valgus was 14.2° at 70° of joint flexion (Fig. 25.6) and the maximal laxity to forced internal rotation wa. 18,5° at 60° of joint flexion (Fig. 25.7). Severance of the anterior fibres in the anterior bundle tended to induce elbow joint laxity to forced valgus and internal rotation in joint extension, and severance of the posterior fibres tended to induce a minor laxity of the elbow joint to forced internal rotation in elbow flexion. Isolated posterior bundle dissection did not give any immediate joint laxity. Sectioning the posterior bundle after the anterior bundle, however, resulted in marked instability of the specimens, with a maximal laxity to forced valgus of 31.2° at 90° of joint flexion (Fig. 25.6), and a maximal laxity to forced internal rotation of 45.5° at the same flexion position (Fig. 25.7). Medial collateral ligament transection induced no changes in joint laxity to forced varus and external rotation.3
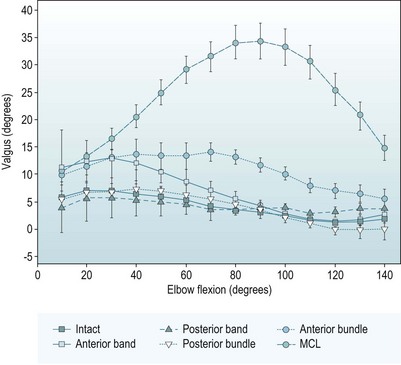
Redrawn from Floris S, Olsen BS, Dalstra M, et al. The medial collateral ligament of the elbow joint: anatomy and kinematics. J Shoulder Elbow Surg 1998; 7:345–751 (Fig. 5).
Redrawn from Floris S, Olsen BS, Dalstra M, et al. The medial collateral ligament of the elbow joint: anatomy and kinematics. J Shoulder Elbow Surg 1998; 7:345–751 (Fig. 7).
Jensen et al showed that isolated reconstruction of the anterior bundle in the MCL-deficient elbow normalized joint stability.18 In another study it was observed that forearm supination tended to stabilize an MCL-deficient elbow joint.19 Generally these observations on laxity associated with MCL-deficient elbows have been confirmed by the findings of other studies using different experimental arrangements.2,15–18
The lateral collateral ligament complex
The LCLC (Fig. 25.5) is divided into the radial or lateral collateral ligament (LCL), which extends from the undersurface of the lateral epicondyle and inserts into the AL. The most posterior fibres pass through the AL and insert distal to the AL on the proximal supinator crest of the ulna.20,21 This ligament band was named the lateral ulnar collateral ligament (LUCL) by O’Driscoll et al.22 In contrast to the observations by these authors we observed the LUCL intimately associated with the LCL superior to the AL, and when passing the AL we observed the ligament to be an integrated part of the AL. The demarcation between the thick ligament and the thinner anterior and posterolateral joint capsule was distinct.20–22
The AL surrounds the radial head and inserts on the anterior and posterior margins of the lesser sigmoid notch.16,20–22
Generally the LCLC has been observed to be a continuum of fibres rather than discrete bands.23
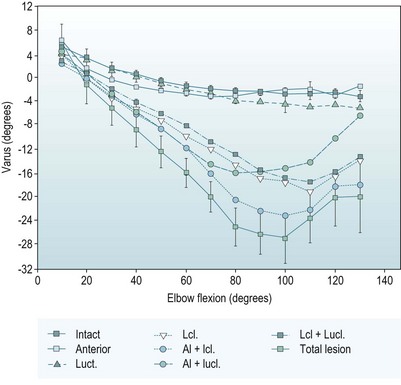
Early studies investigated the influence of the LCL on varus stressed elbow joint stability, and found the LCL to be a constraint of minor importance.11 More recently we performed a series of studies to describe the basic kinematics of the LCLC. We observed that isolated sectioning of the LUCL or the AL produced only minor elbow joint laxity to forced varus (Fig. 25.8) and external rotation (Fig. 25.9). Isolated dissection of the LCL including the posterior LUCL fibres produced a maximal laxity to forced varus of 15.5° at 110° of joint flexion and a maximal laxity to forced external rotation of 22.8° at the same joint flexion. Total LCLC dissection increased the laxity to varus stress to 24.5° at 100° joint flexion and the laxity to forced external rotation to 40° at 80° of joint flexion. The LCLC lesions gave no laxity to forced valgus and internal rotation.20,21 Reconstruction of the LCL, between the humeral epicondyle and the ulna, was shown to normalize elbow constraint in the LCLC deficient elbow joint.21,23 We did not observe any influence on joint kinematics from changes in forearm rotation.20 A more recent study, however, has observed that forearm pronation and muscle loading tend to stabilize the LCL-deficient elbow.6,14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree