Patellofemoral pain is an extremely common disorder, especially in female athletes. There is, however, no true consensus as to the cause and appropriate treatment for patellofemoral pain. This article reviews the epidemiology of patellofemoral pain as well as the proposed etiologies, including quadriceps dysfunction, static alignment disorders, and dynamic alignment disorders. The article also reviews both conservative and surgical treatment of patellofemoral pain.
Patellofemoral pain syndrome is defined as retropatellar or peripatellar pain. It is an extremely common diagnosis in the female athlete. However, obtaining an accurate diagnosis and outlining appropriate treatment are often challenging. Consensus is lacking in the literature regarding the cause and treatment of the syndrome . The patellofemoral joint is complex and dependent on quadriceps function as well as on static and dynamic restraints. The etiology of patellofemoral pain is multifactorial with proposed causes including overuse, overload, biomechanical problems, and muscular dysfunction. Accurate diagnosis requires specific knowledge of the anatomy, biomechanics, and functional behavior of the patellofemoral joint . Most patients are successfully treated by conservative means with the rare few requiring surgical intervention.
Epidemiology of patellofemoral pain
Patellofemoral pain syndrome is considered one of the most common disorders of the knee, accounting for 25% of all knee injuries treated in sports medicine clinics . In clinics that manage patients who have musculoskeletal syndromes, patellofemoral pain syndrome accounts for almost 10% of all visits (76 of 814 visits) and for 20% to 40% of all knee problems (76 of 266 visits) . DeHaven and Lintner reported that among patients diagnosed with patellofemoral pain syndrome over a 7-year period, 18.1% were men and 33.2% were women. They also found an age predilection for the second and third decade of life. Fairbank and colleagues reported on 446 randomly selected students age 13 to 19 years, finding 30% of them had experienced anterior knee pain in the last year and 18% of those in pain had stopped participating in sports because of the knee pain. Taunton and colleagues retrospectively evaluated all patients presenting from 1998 to 2000 to a single health clinic for injuries related to running. Of the 2002 patients, the most common complaint was patellofemoral pain at 16.5%. Of those patients with patellofemoral pain related to running, 38% were men and 62% were women.
Biomechanical etiology of patellofemoral pain syndrome
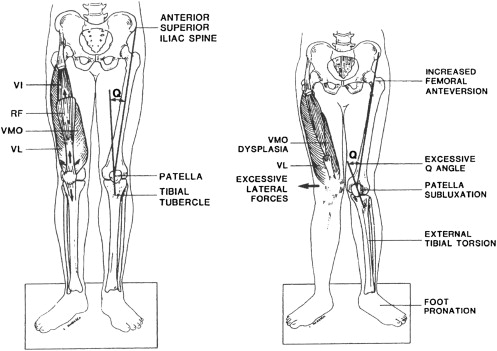
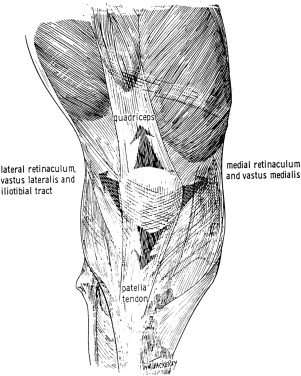
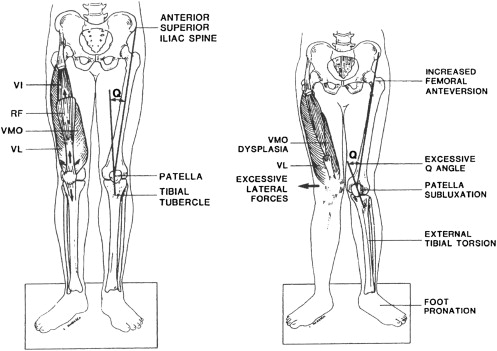
In 1968, Hughston wrote that the primary source of anterior knee pain was extensor mechanism malalignment. In 1979, James coined the term “miserable malalignment syndrome” as the cause of anterior knee pain, describing a combination of factors, including femoral anteversion, squinting patella, patella alta, increased quadriceps angle (Q angle), and tibial external rotation ( Fig. 1 ). These early observations form the foundation for research into the etiology of patellofemoral pain syndrome (PFPS). PFPS has a multifactorial etiology with factors ranging from unsuitable playing surfaces and overtraining, to skeletal alignment abnormalities, to poor neuromuscular control of the lower extremity. The connection among these factors is that they are all assumed to alter the tracking of the patella within the trochlear groove. Proper tracking requires balanced forces acting on the patella ( Fig. 2 ). If any force acting on the patella is too large or too small, then the movement of the patella may be altered, thereby placing additional stresses on the soft tissue of the joint. As the stress exceeds the tissues’ mechanical strength, microdamage, inflammation, and pain result. After a comprehensive review of the literature, the authors have grouped the various etiological factors into three major groups: quadriceps dysfunction, static alignment, and dynamic alignment.
Quadriceps dysfunction
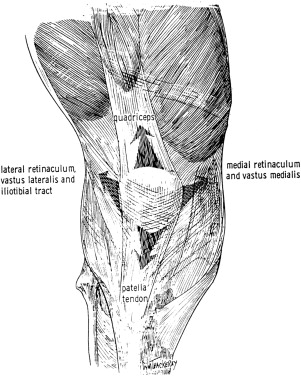
The patella is most directly stabilized by the distal quadriceps, especially the vastus medialis obliques and vastus lateralis. Lateral dynamic forces are produced by the vastus lateralis through the quadriceps tendon and by the biceps femoris, gluteal muscles, and tensor fascia latae through the iliotibial band and lateral retinaculum . The vastus medialis obliques exclusively produce medial dynamic forces . Weakness or delayed firing of the vastus medialis obliques is thought to cause the patella to track laterally, irritating the soft tissues about the joint . While some studies support a difference in vastus medialis oblique and/or vastus lateralis activity in PFPS patients , others have found no differences between those with PFPS and healthy controls . Contradictory results may be explained by the variety of tasks analyzed and data collection methods used in these studies. Contradictory results may also mean that quadriceps dysfunction is not found in all patients with PFPS.
Static malalignment
The anatomical alignment of the pelvis and lower extremity may play a role in the development of PFPS in some individuals. This is referred to as “static alignment” because it is identifiable when the patient is not moving. These findings are also not easily modified with conservative rehabilitation.
A common clinical measurement of the alignment of the lower extremity is the Q angle. This is the angle formed by the intersection of two lines, one connecting the anterior superior iliac spine and the center of the patella and the other connecting the center of the patella to the tibial tuberosity. This angle is thought to represent the line of action of the quadriceps force. A larger Q angle indicates that a greater force is acting laterally on the patella, which may contribute to lateral patellar tracking . Although many sources report that a Q angle greater than 15° to 20° is a risk factor for developing PFPS, the literature is inconsistent in supporting this finding . A review of this literature by Livingston describes how there is a consensus that the Q angle for a typical woman is 3° to 6° larger than the Q angle for a typical man, but there is limited evidence that a Q angle greater than 15° to 20° is related to extensor mechanism dysfunction. For example, only some PFPS patients have a Q angle greater than normal. The inconclusive findings may stem from inconsistent methods for measuring the Q angle. It is also possible that a larger than normal Q angle is just one of several contributing factors to PFPS.
Static malalignment, such as femoral neck anteversion, genu valgum, and external tibial torsion, are also theoretically related to PFPS because they would increase the Q angle. Anteversion, an increased angle between the frontal plane and the femoral neck, can lead to a lower extremity that rotates internally and a gait that toes in . One cadaveric study of knees supports the theory that increased femoral internal rotation leads to increased contact pressure between the patella and the lateral trochlear groove, which would seemingly lead to symptoms of PFPS . Although no difference in femoral anteversion between PFPS and control subjects has been found , it was reported that PFPS patients who failed conservative treatment had significantly more anteversion than those who were successfully treated conservatively . Genu valgum also increases the Q angle and potentially increases the laterally directed forces on the patella . However, when measured statically, there has been no difference in genu valgum between PFPS subjects and controls . Genu valgum may play a more important role in the cause of PFPS during dynamic movement and is described in a later section. External tibial torsion can occur during development as a compensation for femoral anteversion . This leads to the feet pointing outward when the knees are facing forward. The Q angle is larger in these individuals because of the lateral location of the tibial tuberosity. This static malalignment has been seen in some individuals with PFPS. Eckhoff and colleagues reported that PFPS patients who had failed conservative treatment had approximately 6° more tibial external rotation than did those who had successful conservative treatment. Although the majority of PFPS patients have good outcomes with conservative rehabilitation, the studies by Eckhoff and colleagues illustrate that some patients have skeletal static malalignment that will not respond to conservative rehabilitation and may require surgical intervention .
It is often stated that hyperpronation of the foot is a causative factor for PFPS . In theory, increased pronation causes the tibia to internally rotate during the weight acceptance phase of gait, thereby preventing the tibia from fully externally rotating during midstance. This prevents the knee from fully locking via the screw-home mechanism. To compensate, the femur internally rotates to allow the knee to fully lock. Femoral internal rotation during quadriceps contraction may cause a greater lateral force on the patella as it is compressed against the lateral trochlear groove . While some studies have shown increased pronation in PFPS subjects , other studies show no such increase . Despite the inconclusive findings of these studies, there is sufficient evidence that treating PFPS with foot orthotics improves patient outcomes . The exact mechanism as to why foot orthotics are an effective treatment is still being investigated.
In conclusion, studies show that a small percentage of patients with PFPS have symptoms that are likely caused primarily by a static malalignment resulting in increased stress to the patellofemoral joint. For a large majority of PFPS patients, however, no static malalignment is present.
Dynamic malalignment
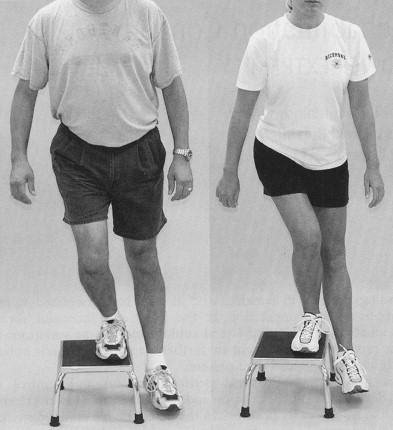
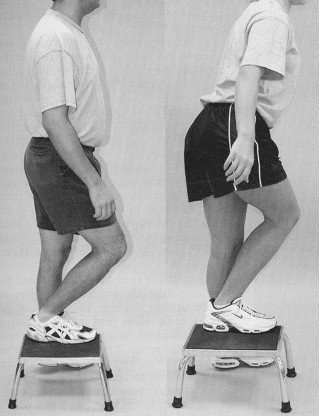
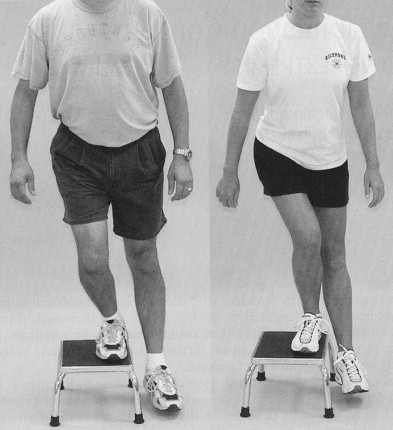
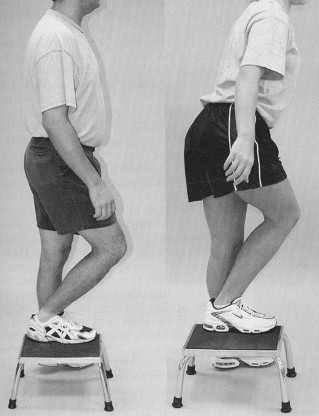
Examining for the static malalignment described above has a place in clinical and scientific evaluation. However, many of those malalignments change once movement is initiated. Furthermore, additional malalignment may exist during movement as a result of poor muscular control of the segments. For example, several investigators have shown that the static Q angle has no direct relationship to PFPS . Rather, it is the “dynamic Q angle” that causes dysfunction, according to these investigators. The concept of poor dynamic alignment took form when clinicians observed a consistent pattern of excessive contralateral pelvic drop, hip adduction and internal rotation, knee abduction, and tibial external rotation and hyperpronation when patients performed a single-leg squat or step down ( Figs. 3 and 4 ). Several investigators have described this movement pattern and its link to PFPS . It was previously thought that abnormal tracking of the patella was due to the abnormal movement of the patella within the trochlear groove. Recently, thinking has changed to the concept that abnormal patellar tracking may be due to abnormal movement of the femur beneath the patella. Dynamic MRI has shown that, during weight-bearing, PFPS subjects had greater femoral internal rotation than controls had . This supports the idea that poor control of the femur may contribute to PFPS symptoms in some subjects.
The observed pattern of poor dynamic alignment has been quantified using kinematic analysis. The fact that a disproportionate number of females suffer noncontact anterior cruciate ligament (ACL) injuries has driven researchers to examine biomechanical differences between males and females during certain movements. Both noncontact ACL injury and PFPS are more prevalent in females and the underlying movement patterns that result in these injuries are similar. The difference is that noncontact ACL injuries occur when a load too large for the ligaments to handle is suddenly applied to the lower extremity. In PFPS, the movement pattern causes increased loading of the tissues of the patellofemoral joint gradually, resulting in the overuse injury.
Three-dimensional video analysis shows that females compared to males have a greater peak knee abduction angle and less knee flexion during a side cutting maneuver , greater knee abduction during a bilateral drop-landing , and greater hip adduction and hip internal rotation during running and cutting. Zeller and colleagues showed that females compared to males had greater foot dorsiflexion, foot pronation, hip adduction, hip flexion, and hip external rotation during a single-leg squat. Lephart and colleagues had slightly different results when examining a single-leg landing. They found that females compared to males had greater hip internal rotation and less knee flexion and knee internal rotation.
Though slight differences in tasks and analysis prevent an absolute consensus on kinematic gender differences during functional tasks, the pattern of poor dynamic alignment in females is supported by objective data. The excessive frontal and transverse plane motion seen in females during functional tasks has been attributed to weakness in the hip abductors and external rotators . During single-leg activities, the gluteus medius is essential in maintaining the position of the pelvis so that the lower extremity is properly aligned. It has been reported that 18.9% of the energy expended during running is used to control movement in the frontal plane . Gluteus medius weakness allows the contralateral pelvis to drop, which puts the stance leg in an adducted position. This is accompanied by excessive internal rotation of the femur and tibia, as well as hyperpronation of the subtalar joint . Weakness in contralateral hip, abdominal, and low back muscles has also been theorized as a factor in poor dynamic alignment .
Recent research has supported this theory that proximal muscle weakness is associated with lower-extremity injury . Recreational runners with a variety of overuse injuries, including PFPS, were found to have significant hip abductor weakness on the injured side compared with the uninjured side and compared with uninjured controls . Ireland and colleagues showed that females with PFPS were significantly weaker in isometric hip abduction and external rotation than uninjured females. They suggested that this weakness may be a cause of the poor dynamic alignment pattern commonly seen in these patients. However, the investigators did not assess lower-extremity motion. In a separate study on hip strength and lower-extremity injury in collegiate athletes, Leetun and colleagues reported that subjects who became injured during the season displayed weakness in hip abduction and external rotation during preparticipation examinations. They were also weaker in hip external rotation and abduction as well as in some of the core muscle endurance assessments. Both of the aforementioned studies hypothesize that the proximal weakness might explain why females display poor dynamic alignment and this may be a factor in both PFPS and noncontact ACL injury. Another study showed that healthy subjects with increased femoral anteversion had lower gluteus medius and vastus medialis oblique electromyographic activity during a clamshell exercise than those with normal hip rotation . This may provide one explanation for how a static malalignment can influence muscle activity during a dynamic task. Although objective data on the prevalence of proximal muscle weakness in PFPS patients is not found in the literature, observations from clinical practice suggest that at least 50% of patients presenting with PFPS have observable weakness of the hip and/or core muscles. Additional research is needed to further understand the role of the hip and core musculature in the development of PFPS.
Biomechanical etiology of patellofemoral pain syndrome
In 1968, Hughston wrote that the primary source of anterior knee pain was extensor mechanism malalignment. In 1979, James coined the term “miserable malalignment syndrome” as the cause of anterior knee pain, describing a combination of factors, including femoral anteversion, squinting patella, patella alta, increased quadriceps angle (Q angle), and tibial external rotation ( Fig. 1 ). These early observations form the foundation for research into the etiology of patellofemoral pain syndrome (PFPS). PFPS has a multifactorial etiology with factors ranging from unsuitable playing surfaces and overtraining, to skeletal alignment abnormalities, to poor neuromuscular control of the lower extremity. The connection among these factors is that they are all assumed to alter the tracking of the patella within the trochlear groove. Proper tracking requires balanced forces acting on the patella ( Fig. 2 ). If any force acting on the patella is too large or too small, then the movement of the patella may be altered, thereby placing additional stresses on the soft tissue of the joint. As the stress exceeds the tissues’ mechanical strength, microdamage, inflammation, and pain result. After a comprehensive review of the literature, the authors have grouped the various etiological factors into three major groups: quadriceps dysfunction, static alignment, and dynamic alignment.
Quadriceps dysfunction
The patella is most directly stabilized by the distal quadriceps, especially the vastus medialis obliques and vastus lateralis. Lateral dynamic forces are produced by the vastus lateralis through the quadriceps tendon and by the biceps femoris, gluteal muscles, and tensor fascia latae through the iliotibial band and lateral retinaculum . The vastus medialis obliques exclusively produce medial dynamic forces . Weakness or delayed firing of the vastus medialis obliques is thought to cause the patella to track laterally, irritating the soft tissues about the joint . While some studies support a difference in vastus medialis oblique and/or vastus lateralis activity in PFPS patients , others have found no differences between those with PFPS and healthy controls . Contradictory results may be explained by the variety of tasks analyzed and data collection methods used in these studies. Contradictory results may also mean that quadriceps dysfunction is not found in all patients with PFPS.
Static malalignment
The anatomical alignment of the pelvis and lower extremity may play a role in the development of PFPS in some individuals. This is referred to as “static alignment” because it is identifiable when the patient is not moving. These findings are also not easily modified with conservative rehabilitation.
A common clinical measurement of the alignment of the lower extremity is the Q angle. This is the angle formed by the intersection of two lines, one connecting the anterior superior iliac spine and the center of the patella and the other connecting the center of the patella to the tibial tuberosity. This angle is thought to represent the line of action of the quadriceps force. A larger Q angle indicates that a greater force is acting laterally on the patella, which may contribute to lateral patellar tracking . Although many sources report that a Q angle greater than 15° to 20° is a risk factor for developing PFPS, the literature is inconsistent in supporting this finding . A review of this literature by Livingston describes how there is a consensus that the Q angle for a typical woman is 3° to 6° larger than the Q angle for a typical man, but there is limited evidence that a Q angle greater than 15° to 20° is related to extensor mechanism dysfunction. For example, only some PFPS patients have a Q angle greater than normal. The inconclusive findings may stem from inconsistent methods for measuring the Q angle. It is also possible that a larger than normal Q angle is just one of several contributing factors to PFPS.
Static malalignment, such as femoral neck anteversion, genu valgum, and external tibial torsion, are also theoretically related to PFPS because they would increase the Q angle. Anteversion, an increased angle between the frontal plane and the femoral neck, can lead to a lower extremity that rotates internally and a gait that toes in . One cadaveric study of knees supports the theory that increased femoral internal rotation leads to increased contact pressure between the patella and the lateral trochlear groove, which would seemingly lead to symptoms of PFPS . Although no difference in femoral anteversion between PFPS and control subjects has been found , it was reported that PFPS patients who failed conservative treatment had significantly more anteversion than those who were successfully treated conservatively . Genu valgum also increases the Q angle and potentially increases the laterally directed forces on the patella . However, when measured statically, there has been no difference in genu valgum between PFPS subjects and controls . Genu valgum may play a more important role in the cause of PFPS during dynamic movement and is described in a later section. External tibial torsion can occur during development as a compensation for femoral anteversion . This leads to the feet pointing outward when the knees are facing forward. The Q angle is larger in these individuals because of the lateral location of the tibial tuberosity. This static malalignment has been seen in some individuals with PFPS. Eckhoff and colleagues reported that PFPS patients who had failed conservative treatment had approximately 6° more tibial external rotation than did those who had successful conservative treatment. Although the majority of PFPS patients have good outcomes with conservative rehabilitation, the studies by Eckhoff and colleagues illustrate that some patients have skeletal static malalignment that will not respond to conservative rehabilitation and may require surgical intervention .
It is often stated that hyperpronation of the foot is a causative factor for PFPS . In theory, increased pronation causes the tibia to internally rotate during the weight acceptance phase of gait, thereby preventing the tibia from fully externally rotating during midstance. This prevents the knee from fully locking via the screw-home mechanism. To compensate, the femur internally rotates to allow the knee to fully lock. Femoral internal rotation during quadriceps contraction may cause a greater lateral force on the patella as it is compressed against the lateral trochlear groove . While some studies have shown increased pronation in PFPS subjects , other studies show no such increase . Despite the inconclusive findings of these studies, there is sufficient evidence that treating PFPS with foot orthotics improves patient outcomes . The exact mechanism as to why foot orthotics are an effective treatment is still being investigated.
In conclusion, studies show that a small percentage of patients with PFPS have symptoms that are likely caused primarily by a static malalignment resulting in increased stress to the patellofemoral joint. For a large majority of PFPS patients, however, no static malalignment is present.
Dynamic malalignment
Examining for the static malalignment described above has a place in clinical and scientific evaluation. However, many of those malalignments change once movement is initiated. Furthermore, additional malalignment may exist during movement as a result of poor muscular control of the segments. For example, several investigators have shown that the static Q angle has no direct relationship to PFPS . Rather, it is the “dynamic Q angle” that causes dysfunction, according to these investigators. The concept of poor dynamic alignment took form when clinicians observed a consistent pattern of excessive contralateral pelvic drop, hip adduction and internal rotation, knee abduction, and tibial external rotation and hyperpronation when patients performed a single-leg squat or step down ( Figs. 3 and 4 ). Several investigators have described this movement pattern and its link to PFPS . It was previously thought that abnormal tracking of the patella was due to the abnormal movement of the patella within the trochlear groove. Recently, thinking has changed to the concept that abnormal patellar tracking may be due to abnormal movement of the femur beneath the patella. Dynamic MRI has shown that, during weight-bearing, PFPS subjects had greater femoral internal rotation than controls had . This supports the idea that poor control of the femur may contribute to PFPS symptoms in some subjects.
The observed pattern of poor dynamic alignment has been quantified using kinematic analysis. The fact that a disproportionate number of females suffer noncontact anterior cruciate ligament (ACL) injuries has driven researchers to examine biomechanical differences between males and females during certain movements. Both noncontact ACL injury and PFPS are more prevalent in females and the underlying movement patterns that result in these injuries are similar. The difference is that noncontact ACL injuries occur when a load too large for the ligaments to handle is suddenly applied to the lower extremity. In PFPS, the movement pattern causes increased loading of the tissues of the patellofemoral joint gradually, resulting in the overuse injury.
Three-dimensional video analysis shows that females compared to males have a greater peak knee abduction angle and less knee flexion during a side cutting maneuver , greater knee abduction during a bilateral drop-landing , and greater hip adduction and hip internal rotation during running and cutting. Zeller and colleagues showed that females compared to males had greater foot dorsiflexion, foot pronation, hip adduction, hip flexion, and hip external rotation during a single-leg squat. Lephart and colleagues had slightly different results when examining a single-leg landing. They found that females compared to males had greater hip internal rotation and less knee flexion and knee internal rotation.
Though slight differences in tasks and analysis prevent an absolute consensus on kinematic gender differences during functional tasks, the pattern of poor dynamic alignment in females is supported by objective data. The excessive frontal and transverse plane motion seen in females during functional tasks has been attributed to weakness in the hip abductors and external rotators . During single-leg activities, the gluteus medius is essential in maintaining the position of the pelvis so that the lower extremity is properly aligned. It has been reported that 18.9% of the energy expended during running is used to control movement in the frontal plane . Gluteus medius weakness allows the contralateral pelvis to drop, which puts the stance leg in an adducted position. This is accompanied by excessive internal rotation of the femur and tibia, as well as hyperpronation of the subtalar joint . Weakness in contralateral hip, abdominal, and low back muscles has also been theorized as a factor in poor dynamic alignment .
Recent research has supported this theory that proximal muscle weakness is associated with lower-extremity injury . Recreational runners with a variety of overuse injuries, including PFPS, were found to have significant hip abductor weakness on the injured side compared with the uninjured side and compared with uninjured controls . Ireland and colleagues showed that females with PFPS were significantly weaker in isometric hip abduction and external rotation than uninjured females. They suggested that this weakness may be a cause of the poor dynamic alignment pattern commonly seen in these patients. However, the investigators did not assess lower-extremity motion. In a separate study on hip strength and lower-extremity injury in collegiate athletes, Leetun and colleagues reported that subjects who became injured during the season displayed weakness in hip abduction and external rotation during preparticipation examinations. They were also weaker in hip external rotation and abduction as well as in some of the core muscle endurance assessments. Both of the aforementioned studies hypothesize that the proximal weakness might explain why females display poor dynamic alignment and this may be a factor in both PFPS and noncontact ACL injury. Another study showed that healthy subjects with increased femoral anteversion had lower gluteus medius and vastus medialis oblique electromyographic activity during a clamshell exercise than those with normal hip rotation . This may provide one explanation for how a static malalignment can influence muscle activity during a dynamic task. Although objective data on the prevalence of proximal muscle weakness in PFPS patients is not found in the literature, observations from clinical practice suggest that at least 50% of patients presenting with PFPS have observable weakness of the hip and/or core muscles. Additional research is needed to further understand the role of the hip and core musculature in the development of PFPS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





