Patellar Tendon Graft Harvesting
David A. McGuire
Stephen D. Hendricks
INDICATIONS/CONTRAINDICATIONS
The patellar tendon graft is indicated in most patients undergoing reconstruction of a torn anterior cruciate ligament (ACL). Situations in which an autogenous patellar tendon may be contraindicated include the multiply operated knee where reharvest of previously harvested patellar tendon would be needed, patients with an arthritic patellofemoral joint, or patients with previous patellar trauma such as a fracture. In addition, individuals whose occupation requires repetitive kneeling or working on their hands and knees may pose a relative contraindication. In these patients, other graft sources such as hamstring tendons or allografts should be considered.
PREOPERATIVE PLANNING
Certain preoperative steps should be taken when an autogenous patellar tendon graft is considered. Radiologic imaging will help identify those patients with a degenerative patellofemoral joint or significant patellar baja or alta. If patella alta is identified, there are several techniques available to deal with a graft that is longer than required. The knee also should be examined for any signs of patella maltracking or instability. A suitable graft table and required instrumentation should be available to prepare the graft efficiently for fit and insertion ease.
SURGERY
Patient Positioning
The patient is positioned supine with the leg hung free. A standard arthroscopy prep and drape of the knee is used. A tourniquet is placed around the thigh, and a leg holder is placed at the level of the tourniquet. Anesthesia is typically general, although an epidural is an alternative.
Technique
The bone patellar tendon bone (BTB) graft can be harvested through two small vertical incisions (Fig. 15-1). The vertical incisions are cosmetic, and may lead to less morbidity and pain than a single long incision. Because the tibial drill guide will be positioned through the tibial harvest incision, the location of this incision is important to the placement of the tibial tunnel. With this in mind, the tibial incision begins 2 cm distal to the joint line and 1 cm medial to the tibial tubercle and extends 2.5 cm distally. The patellar incision begins at the distal pole of the patella and extends 2.5 cm proximally over the midline of the patella. Although we prefer the two-incision technique, a single skin incision can be used.
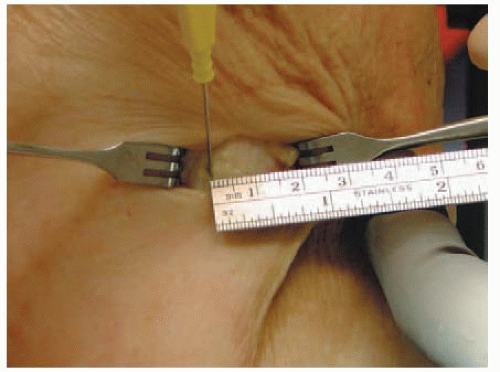
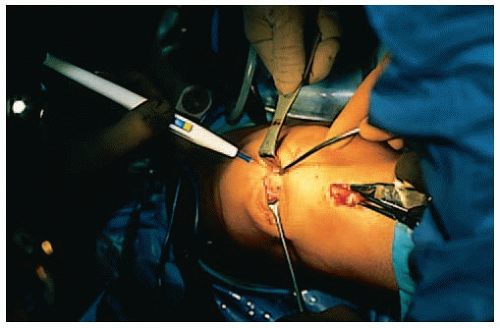
The tibial bone plug is harvested first. Lateral retraction of the skin will allow clear visualization of the tendon attachment site. The central 10 mm of the patellar tendon attachment is measured, and the medial/lateral borders are marked with electrocautery (Fig. 15-2). Using a stoppered plunge blade (Plunge Blade, Linvatec, Largo, FL), the tibial bone plug is created (Fig. 15-3). With the saw blade angled to approximately 45 degrees, the cuts are made to a depth of 8 mm (Fig. 15-4). The stoppered plunge blade will limit the cut depth to 8 mm and therefore eliminate the risk of overpenetration. Using a side-to-side rocking motion, the side cuts are carried distally for 2.5 cm. A horizontal saw cut is made to connect the distal ends of the parallel side cuts.
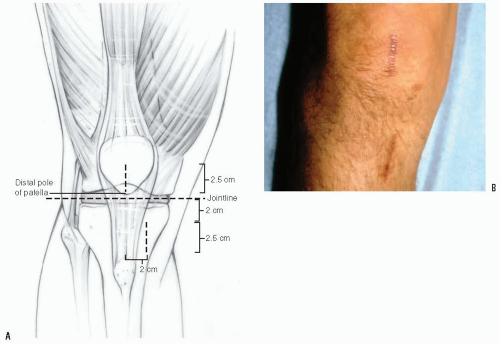 FIGURE 15-1 A: The BTB tendon can be harvested through two 1-in incisions. The two small incisions are more cosmetic than one large one. B: Incisions closed and healed. |
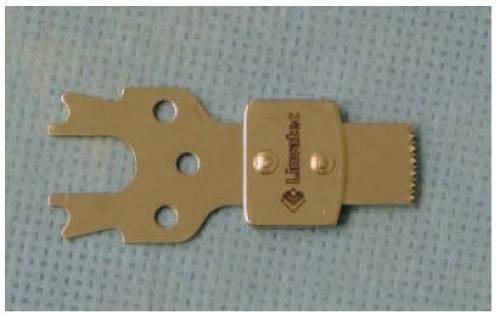 FIGURE 15-3 The plunge blade has a stopper 8 mm from the saw blade teeth, preventing penetration of the saw blade beyond that depth. |
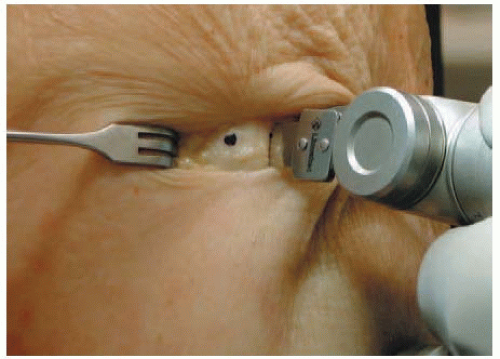
Beginning distally at the tibial bone plug and working proximally toward the patella, a double-bladed tendon harvester (Parasmillie meniscotome, Linvatec, Largo, FL) is used to incise both sides of the graft simultaneously (Fig. 15-5). The fixed width of the blades (10 mm) helps maintain a constant graft width throughout tendon harvest. The tendon harvester is advanced proximally until the harvester tips make contact with the distal pole of the patella. The tips of the harvester should be visible through the patellar incision.
Using the tips of the harvester as a guide, the medial and lateral margins of the patellar bone plug are marked with electrocautery (Fig. 15-6), generating a patellar bone plug width of 11 mm. Beginning distally at the marked sites, use the stoppered plunge blade to create the side cuts for the patellar bone plug. With the blade angled to 45 to 60 degrees, the saw cuts are made to a depth of 8 mm (Fig. 15-7). Advance the cuts proximally until a bone plug length of 25 mm is obtained. Using a horizontal saw cut, connect the proximal termination of the two side cuts (Fig. 15-8).
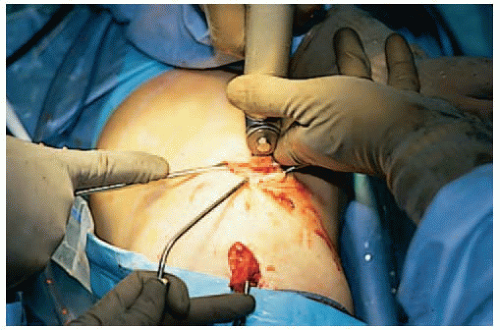
Attention is directed to the tibial bone plug. Using a ¼-inch osteotome, remove the tibial bone plug from the tibia (Fig. 15-9). Scissors may be needed to cut any remaining soft tissue connections.
Grasp the tibial bone plug with a Kocher, and advance the bone plug proximally through the tibial incision and out the patellar incision (Fig. 15-10). Using an osteotome, remove the patellar bone plug. Again, scissors may be needed to remove any remaining soft tissue connections and completely free the graft. Carefully transfer the graft to a back table for preparation.
Grasp the tibial bone plug with a Kocher, and advance the bone plug proximally through the tibial incision and out the patellar incision (Fig. 15-10). Using an osteotome, remove the patellar bone plug. Again, scissors may be needed to remove any remaining soft tissue connections and completely free the graft. Carefully transfer the graft to a back table for preparation.
 FIGURE 15-5 The Parasmillie meniscotome cleaves both the medial and lateral borders of the patellar tendon simultaneously, ensuring a constant graft width along the entire length of the harvest. |
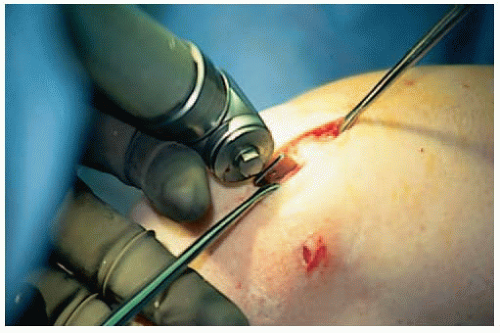 FIGURE 15-7 When in use, the stopper prevents the blade from producing cuts with variable depths. A bone plug defect with varying cut depths may lead to stress risers and patellar fracture. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree