Double-Bundle Posterior Cruciate Ligament Reconstruction
Anthony M. Buoncristiani
Fotios P. Tjoumakaris
Christopher D. Harner
INDICATIONS/CONTRAINDICATIONS
Posterior cruciate ligament (PCL) injuries are rare and infrequently occur in isolation. Although we have an increased knowledge of the anatomy and mechanism of injury, PCL reconstruction has not obtained the success of anterior cruciate ligament (ACL) reconstruction. In addition, frustrating to the surgeon is the lack of consensus regarding the optimal management of PCL injuries. Isolated PCL injuries (grades I and II) can be treated nonoperatively with protected weight-bearing and quadriceps muscle rehabilitation. However, some studies have demonstrated degenerative changes and poor objective outcomes associated with conservative treatment of PCL injuries.
The absolute indications for reconstruction of an isolated PCL tear would be for persistent instability (grade III) or a boney avulsion. However, some authors dispute the existence of an isolated PCL injury. Regardless, most PCL reconstructions occur in conjunction with a knee dislocation. Advances in the understanding of the anatomy and biomechanics of the PCL have led to an increased interest in arthroscopic reconstruction of the PCL. Anatomic studies have delineated separate characteristics of the anterolateral (AL) and posteromedial (PM) bundles within the PCL. The larger AL bundle has increased tension in flexion, whereas the PM bundle becomes more taut in extension. In addition, the smaller meniscofemoral ligaments also contribute to the overall strength of the PCL. The timing of PCL reconstruction is controversial, but an acute reconstruction is generally accepted for boney avulsion injuries or while addressing combined ligamentous injuries-especially a posterolateral corner injury. The double-bundle PCL reconstruction technique is most commonly performed in the chronic setting, when very little native ligament remains available for augmentation.
Contraindications to an acute PCL reconstruction would be in the setting of a traumatic knee arthrotomy or with a stiff knee. The double-bundle technique is not recommended if any bundle remains intact. In this scenario, we prefer a single-bundle augmentation, which is the most likely clinical presentation. We always attempt to preserve any remnant tissue whenever possible unless located directly at the insertion site of the target bundle. The grafts are passed around the meniscofemoral ligaments, which does increase the complexity of the reconstruction.
PREOPERATIVE PLANNING
A thorough history and physical examination are obtained preoperatively in a clinic setting. It is important to determine the chronicity of the injury. Acutely, there is usually a history of a direct blow to the anterior lower leg or a hyperextension injury with concomitant mild swelling. A PCL injury may also occur in the setting of a knee dislocation with involvement of the posterolateral structures (approximately 60%). Chronically, instability may be the only complaint.
On physical examination, it is important to assess the neurovascular status of the injured limb. This is especially important if there is a history of a knee dislocation, which has a higher risk of such an injury. Inspect and palpate for an effusion followed by assessing the range of motion. With the knee in a flexed position, palpate for the natural tibial step-off and evaluate the anterior border of tibial plateau in relation to the femoral condyles. In addition, a Godfrey test can be performed whereby the lower leg is elevated with the knee flexed approximately 90 degrees to assess for the presence of a “sag.” A posterior drawer with the knee in 90 degrees of flexion is also performed to evaluate the amount of posterior tibial translation (Fig. 19-1). It is important to recognize the presence of a posterolateral corner knee injury, which will accentuate the posterior drawer. The gait pattern is inspected for any varus thrust. If a posterolateral corner injury is suspected, the physical examination should include a reverse pivot shift test, a dial test, a posterolateral drawer, and varus stress testing at both 30 and 90 degrees.
Radiographs of the knee should be performed to inspect for any fracture in the acute setting or for any medial or patellofemoral compartmental arthrosis in the chronic setting. Long-leg cassette films should be obtained if any coronal instability is suspected. Posterior tibial subluxation can possibly be seen on the lateral radiograph. Otherwise, a comparative stress lateral radiograph can also be obtained. A bone scan may be useful in chronic PCL insufficiency to identify degenerative changes. A magnetic resonance image (MRI) is essential not only to confirm a PCL injury, but more importantly to assess for any concomitant posterolateral corner injury or meniscal pathology that will affect the operative plan.
SURGERY
Patient Positioning
The patient is identified in the preoperative holding area and the operative site is signed. Sciatic and femoral nerve blocks are performed by the anesthesiology staff. The patient is taken to the operating room, where spinal or general anesthesia is induced. The patient is positioned supine on the operating room table. A padded bump is taped to the operating room table at the foot with the knee flexed to 90 degrees to hold the leg flexed during the case. A side post is placed on the operative side just distal to the greater trochanter to support the proximal leg with the knee in flexion. Padded cushions
are placed under the nonoperative leg. We do not routinely use a tourniquet so that the vascular status of the extremity can be checked intraoperatively (Fig. 19-2).
are placed under the nonoperative leg. We do not routinely use a tourniquet so that the vascular status of the extremity can be checked intraoperatively (Fig. 19-2).
Examination under Anesthesia
An examination under anesthesia (EUA) is then performed. The nonoperative knee is examined followed by the operative knee. The alignment and range of motion are assessed with specific attention to terminal extension and flexion. A thorough ligamentous examination as previously described is then performed to confirm our preoperative diagnosis and assess for any other pathology. Lower grades of posterior drawer and reverse pivot shift tests may represent an intact AL or PM bundle of the PCL. Fluoroscopy is used after the EUA. Lateral views are obtained with the tibia displaced posteriorly and then reduced with an anterior force. The sloped posterior tibial fossa is identified for later tibial tunnel placement.
Surface Anatomy and Skin Incisions
The knee is flexed to 90 degrees and the vertical arthroscopy portals are delineated. The anterolateral portal is placed just lateral to the lateral border of the patellar tendon and adjacent to the inferior pole of the patella. The anteromedial portal is positioned approximately 1 cm medial to the medial border of the superior aspect of the patellar tendon (Fig. 19-3). An accessory posteromedial portal is created just proximal to the joint line and posterior to the medial collateral ligament under direct arthroscopic guidance. If meniscal repair or other surgical procedures are expected, these incisions are marked as well. The proposed incisions are then cleansed with sterile Betadine paint and injected with a local anesthetic and epinephrine. The leg is cleansed with an alcohol solution and Betadine, with care taken to preserve the incision marks. The operative leg is draped using a sterile technique. A hole is cut in the stockinette for access to the dorsalis pedis pulse throughout the case. After draping, the arthroscopy equipment is prepared and the fluoroscopy machine is later draped (Fig. 19-4).
 FIGURE 19-2 The positioning and preparation are demonstrated. The knee rests comfortably at 90 degrees of flexion without the use of assistants. |
Graft Preparation
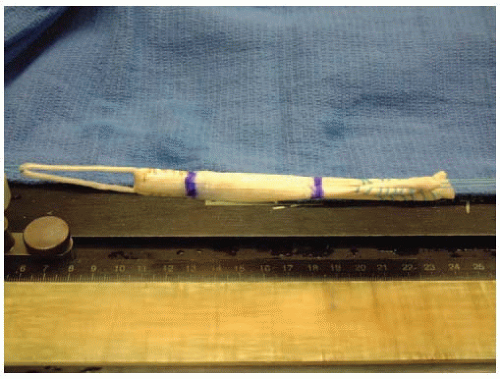
In general, two long (approximately 24 cm in length) tibialis anterior allografts are preferred over a split allograft. The soft tissue allografts are thawed in sterile saline solution. A whipstitch is placed in each of the free ends of the graft. A closed Endoloop of 30 to 40 mm in length is used without the EndoButton (Smith & Nephew, Inc., Andover, MA) (Fig. 19-5). With the standard EndoButton technique, a significant portion of the tunnel will contain only the Endoloop suture, with some graft left outside the tibial tunnel. The EndoButton is carefully removed using a wire cutter to avoid damage to the loop. This is done to minimize the amount of Endoloop and maximize the amount of graft within the femoral tunnel.
The allograft is passed through and doubled over the Endoloop, halving its length to 12 cm. A No. 5 braided suture is placed through the Endoloop and the graft is tensioned. The graft is marked 25 mm from the Endoloop end for later referencing when passing the graft into the femoral tunnel and 50 mm from this mark to represent the intra-articular portion of the graft. The width of the graft is measured on the tibial and femoral ends. The desired AL allograft width is 9 to 10 mm versus 7 mm for the PM allograft. The graft is kept in a damp sponge until needed for graft passage.
 FIGURE 19-4 Fluoroscopy is used for proper placement of the tibial tunnel. The knee can be easily visualized in this setting when placed at 90 degrees. |
Arthroscopy
A thorough diagnostic arthroscopy is performed to assess the cruciate ligaments and evaluate for other cartilage or meniscal derangements. The notch is examined for any remaining intact PCL fibers of the AL or PM bundles. If specific fibers from either bundle or the meniscofemoral ligaments are left, care should be taken to preserve these fibers during the case for augmentation. Frequently, the AL bundle is ruptured and the PM bundle remains intact.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree