Opening Wedge Osteotomy—Proximal Tibia and Distal Femur
Giancarlo Puddu
Vittorio Franco
Massimo Cipolla
Guglielmo Cerullo
Enrico Gianni
INDICATIONS/CONTRAINDICATIONS
Osteoarthrosis of the knee has many causes. Degenerative changes of the articular cartilage can occur through tension, compression, or shear. These changes are very much related to the forces exerted on the bearing surfaces. Genetic factors are known to play a part. Specific trauma and trauma from the overload caused by obesity or occupational factors are etiologically important. In essence, the biophysical cause of osteoarthrosis is an overload or a concentration of forces beyond the ability of the cartilage and subchondral bone to cope.
In any discussion of osteoarthrosis of the knee and its treatment, the operation of knee replacement (arthroplasty) versus knee realignment (osteotomy) is always pertinent. Historically, osteotomy preceded replacement by about 10 years. As replacement became a reality in the 1970s, the indications for each operation became clearer. While the annual number of osteotomies has remained stable, the proportional rate of total arthroplasties has increased dramatically since the early 1960s.
It follows that alignment of the lower extremity plays an important role in osteoarthrosis of the knee. Malalignment into a varus position overloads the medial condyles of the femur and tibia; valgus malalignment, similarly, overloads the lateral condyles. The rationale behind the osteotomy is to correct the angular deformity at the knee and therefore to decrease the excessive weight-bearing load across the affected compartment, which is the most involved by the degenerative process. Since alternative treatments for severe osteoarthrosis of the knee in the 1960s were limited, tibial osteotomy at the beginning was used for osteoarthrosis, rheumatoid arthritis, and secondary arthrosis, regardless of the etiopathogenesis and the magnitude of the angular deformity. After several years’ experience, Coventry (1), Insall (3), and others narrowed the indications for tibial osteotomy. By the late 1970s, high tibial osteotomy was felt to be for the younger, more active patient in whom total knee replacement was thought to be unwise.
Now we think that the patients selected for proximal tibial/distal femur osteotomy should have mostly unicompartmental osteoarthrosis with axial malalignment. However, fracture and other trauma, congenital and acquired deformities, and idiopathic osteonecrosis are also reasons for osteotomy.
A patient is typically a candidate for high tibial osteotomy when the orthopaedic surgeon can clinically detect a varus standing alignment associated with a medial compartment arthritis in a stable knee; a medial compartment cartilage damage associated with anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), posterolateral corner, or combined ligament deficiencies; a painful knee after
a medial meniscectomy; articular cartilage defects requiring a repair technique; an osteochondritis dissecans lesion; or a patient who requires a meniscal allograft.
a medial meniscectomy; articular cartilage defects requiring a repair technique; an osteochondritis dissecans lesion; or a patient who requires a meniscal allograft.
A typical candidate for distal femur osteotomy is young or middle-aged, athletic patient who has developed a disabling painful knee due to an early arthritis of the lateral compartment after lateral meniscectomy. Also candidate to the antivalgus procedure is the patient with chondral damages of the lateral femoral condyle associated with an ACL or PCL acute tear or chronic laxity; the patient with congenital valgus deformity often associated with overweight and lateral compartment arthritis; and the patient with a cyst of the lateral meniscus or with a discoid meniscus followed by a subtotal meniscectomy.
There is no definite patientage below which one should have an osteotomy, or above which one should have an arthroplasty. The age of 65 years is cited most often, but activity level, lifestyle, and general health must be considered. As long-term studies of arthroplasty demonstrate, age considerations may change. But the fact remains that osteotomy patients are generally younger than those who undergo knee arthroplasty.
Osteotomy is best done for unicompartmental osteoarthrosis in knees with generally well-maintained range of motion (ROM) (at least 90 degrees of flexion; less than 15 degrees of flexion contracture). Osteotomy should probably not be done in patients with rheumatoid arthritis, patients with very unstable knees, or those whose knees have greater than 20 degrees of varus deformity or 15 degrees of valgus deformity, according to Insall (2). These knees are complicated by an associated severe ligamentous laxity and subluxation; the latter is a relative contraindication. In fact, even if the correction of the mechanical axis in such a great deformity can result in a relaxed collateral ligamentous complex, often the knee finds a new functional stability so that many authors, including ourselves, do not routinely perform retightening of the ligamentous structures.
A patient who has varus deformity and ACL insufficiency may be treated with an ACL reconstruction in addition to the proximal tibial osteotomy. A technically demanding procedure, the osteotomy associated with the ligament reconstruction addresses the underlying disorder and corrects the problems. Because this is not a routine procedure, it will not be discussed here. However, the symptoms of pain and instability must be separated as clearly as possible, because when pain prevails, especially in sedentary patients, correction of alignment, with consequent relief of medial compartment pain, can be a satisfactory treatment.
The varus arthritic symptomatic knee very often shows articular cartilage lesions, Outerbridge (4) grades III and IV, that affect the involved medial compartment. Full-thickness chondral defects rarely heal without a direct intervention. Together with the modern proposals of treatment of the articular cartilage tears (autologous chondrocyte implantation and osteochondral autografts), the methods based on bone marrow stimulation are still in action. Historically, the first technique of marrow stimulation proposed was the Pridie drillings, introduced by the author in 1959. Presently, Steadman’s (7) microfracture arthroplasty seems a more effective and safer option, as it is completely arthroscopic, and has the advantage, compared with the former, of not inducing local thermal necrosis. When performed together with the HTO, microfractures fully complement the surgical treatment, satisfying the necessity of a direct treatment of the intra-articular pathology, without increasing the risk of complications or lengthening time of surgery.
Overweight is a controversial topic. Obesity has a negative effect on the outcome of surgery in many orthopaedic operations. Most would agree that excess weight could make a patient a better candidate for osteotomy than for arthroplasty, but it is also true that obesity itself represents a negative factor in view of the possible general postoperative complications. When a patient is overweight, the weight should be brought to near normal before surgery, since osteotomy has a worse long-term outcome when the patient is obese.
Another contraindication to osteotomy is severe bone loss (more than a few millimeters) of the medial or lateral tibia or femur. When medial or lateral compartment bony support is insufficient, congruent weight bearing on both tibial plateaus following the osteotomy is impossible. In this situation tibiofemoral contact will teeter on the relatively prominent intercondylar tibial spines.
Severe varus or valgus deformity may be associated with lateral or medial subluxation of the tibia, respectively. Subluxation of more than 1 cm is an absolute contraindication to osteotomy, and some authors suggest that osteotomy should not be performed if any translation or subluxation is present.
Studies on the biomechanics of the dynamic gait accurately addressed the issue of varus or lateral thrust of the knee during ambulation. The term adductor moment was used to describe the amount of lateral or varus thrust of the knee observed during gait. Patients with high adductor moment have
worse results following osteotomy than those with a low adductor moment. Furthermore, patients with a high adductor moment are more likely to have a recurrent varus deformity following valgus osteotomy. When osteotomy is chosen for those patients in spite of a high adductor moment, overcorrection of the deformity may be helpful.
worse results following osteotomy than those with a low adductor moment. Furthermore, patients with a high adductor moment are more likely to have a recurrent varus deformity following valgus osteotomy. When osteotomy is chosen for those patients in spite of a high adductor moment, overcorrection of the deformity may be helpful.
Osteotomy of the proximal tibia or distal femur is designed to relieve pain caused by medial or lateral tibiofemoral osteoarthrosis. Slight degenerative changes of the patellofemoral joint are not a contraindication to osteotomy. However, following proximal tibial osteotomy with a medial opening wedge, the anterior tibial tubercle is lowered to about one half of the angular correction; therefore, the condition of “patella baja” is a contraindication to this kind of operation.
PREOPERATIVE PLANNING
The goal of knee osteotomy is to realign the mechanical axis of the limb, thereby shifting weightbearing forces from a diseased compartment to a more normal compartment.
The alignment of the limb is best measured by full-length radiographs of the lower extremity.
The mechanical axis is determined by drawing a line from the center of the femoral head through the center of the knee to the center of the talus. The anatomic axis is depicted by drawing a line through the center of the shaft of the femur and through the center of the shaft of the tibia. In the normal knee, the two lines cross each other in the center of the joint, making an angle of 5 degrees (physiologic valgus), and the mechanical axis passes through the center of the joint, or slightly varus (about 1 degree medially).
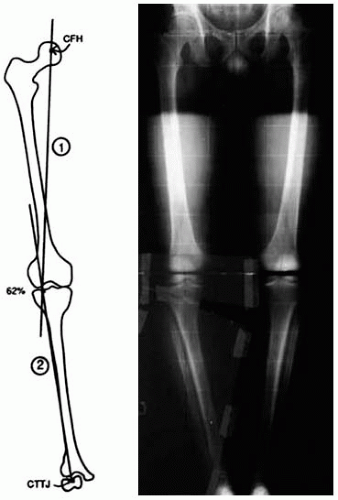
The deformity is measured by using these parameters as the reference points of “normality.” With a varus knee we want to move the mechanical axis through the neutral alignment (approximately the center of the knee) up to a more lateral point at about two thirds (63%) of the tibial plateau to get 5 degrees of mechanical valgus alignment and thereby overcorrect the anatomic valgus from the “normal” 5 degrees to 9 or 10 degrees (Fig. 30-1). Extensive experience has shown that overcorrection is absolutely essential if one wants to optimize a long-standing result from valgus osteotomy. It is inconvenient to correct to normal valgus that brings the extremity back to the position from which it originally became deformed, and that does not properly unload the medial compartment. In the normal knee, approximately 60% of the weight-bearing forces are transmitted through the medial compartment and approximately 40% are transmitted through the lateral compartment. Even in severe valgus deformity (up to 30 degrees valgus), the medial plateau load never falls below 30%.
There is a controversy about full-length radiographs made with the patient supine compared with those made with the patient standing. Originally these radiographs were made with the patient supine. Then, some surgeons noted that, in this position, the amount of deformity was underestimated in certain patients who had osseous defects or ligamentous laxity, and this was presented as a cause of undercorrection by the osteotomy. For these reasons, most authors currently recommend that radiographs be made with the patient standing. However, two problems remain. First, because the patient can take the weight off the painful limb when standing and thus negate much of the benefit of this position, it could be better to take the radiographs with the patient standing on only the affected limb. Second, when there is severe ligamentous laxity, to plan the operation on radiographs made with the patient standing can lead to overcorrection, a potentially greater problem than undercorrection.
When we have a reasonable doubt from the physical examination, we calculate the joint line convergence angle (JLCA), which is formed by a line tangent to the distal femoral condyles and a line tangent to the tibial plateau. A single-leg weight-bearing full radiograph and a double-leg full radiograph, always in standing position, are obtained to measure the lower limb alignment. The difference in the JLCA between the two radiographs represents the component of malalignment associated with ligamentous laxity. To prevent overcorrection, the soft tissue laxity is subtracted from the overall valgus correction.
A young patient with a symptomatic congenital varus could be an early candidate for a valgus osteotomy, but the correction must not be an overcorrection, because in such patients it is sufficient to restore the physiologic alignment of the knee.
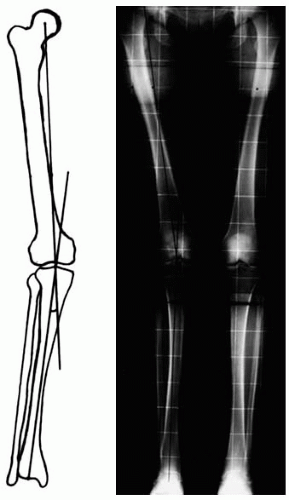
With the valgus knee, we want to reposition the mechanical axis to neutral alignment at approximately 0 degrees in the center of the joint. This means 5 degrees of anatomic and physiologic valgus (Fig. 30-2). The biomechanics of varus and valgus deformities of the knee differ. In fact, the intrinsic valgus angle between femur and tibia determines an asymmetric overload of the medial compartment, at about 60% of the whole, already in the normal knee. Thus, the overbalance of the knee toward a varus alignment will result in a functional disaster because of the additional overload of the medial compartment and the consequent, dramatic acceleration of the degenerative changes of the more normal side.
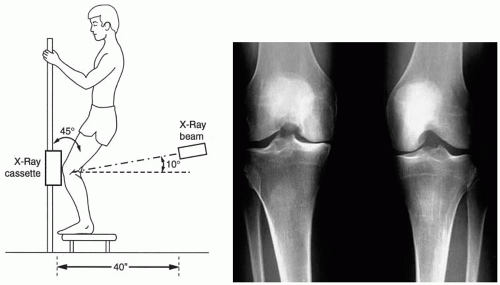 FIGURE 30-3 The Rosenberg view. Comparative posteroanterior weight-bearing knee radiograph at 45 degrees of flexion facilitates the diagnosis if the standard standing AP view is not sensitive enough. |
The osteotomy we propose here is based on the opening wedge technique. Special plates with a spacer “tooth” were designed for this aim. We need to know the size of the base of the wedge, calculated in millimeters, to choose the plate and fix the osteotomy to the planned angle. Different widths of the tibia, at the level of the osteotomy cut, correspond to different wedge sizes, for the same degree of angular correction.
To complete evaluation of the knee, we look at the different radiographic views, including the standard lateral and the axial views of the patellofemoral joint.
The Rosenberg view, comparative posteroanterior weight-bearing radiograph at 45 degrees of knee flexion, facilitates the diagnosis in case the standard anteroposterior (AP) view is not sensitive enough (Fig. 30-3). The Rosenberg examination has a strong predictive value when the deformity is associated with a cruciate insufficiency, and therefore the chondral wear prevails in the posterior part of the tibial plateaus.
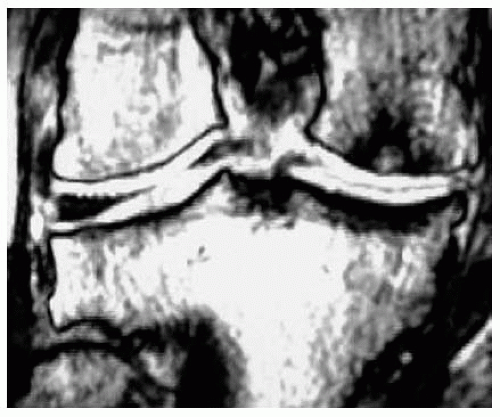
Most authors don’t recommend computed tomography (CT) scans or magnetic resonance imaging (MRI) in studying a candidate for knee osteotomy; but we think that the stress reaction of the subchondral bone, detectable by MRI (Fig. 30-4), could be the only sign of a degenerative process at its earlier stage.
SURGERY
Dedicated Surgical Instrumentation
The object of valgus osteotomy is to obtain a new mechanical axis overcorrected up to 5 degrees of valgus. Our purpose with varus osteotomy is to reposition the lower limb to align to the physiologic 0 degrees of the neutral mechanical axis.
We present here our technique to perform the opening wedge osteotomy. To achieve more reproducible results with the fewest technical difficulties, the senior author (GP) developed a complete but simple and easy system of dedicated instruments and plates.
We get the valgus correction of the knee by means of proximal tibia osteotomy and the varus correction by means of distal femoral osteotomy. In varus deformity the tibiofemoral joint line is usually parallel to the floor. Proximal tibia osteotomy has been demonstrated to transfer load effectively from the medial to the lateral compartment. In valgus deformity, the joint line has a valgus tilt with a correspondent obliquity from superolateral to inferomedial direction. Although tibial varus osteotomy may realign a valgus limb, it cannot correct the joint-line tilt because the procedure is performed distally to the joint. The mechanical consequence of this, in patients with severe valgus deformities (more than 10 to 12 degrees according to various authors), is the effect of transferring the load transmission medially not more than the lateral portion of the tibial spine. The resultant increased valgus tilt of the joint line leads to greater shear forces and lateral subluxation during gait. However, distal femoral varus osteotomy may realign a valgus limb and correct valgus tilt of the joint line when used to treat lateral tibiofemoral osteoarthrosis with valgus deformity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree