Chapter 113 Patellar Resurfacing in Total Knee Arthroplasty
Native Patellofemoral Joint
Kinematics
Kinematics of the knee joint characterizes the relative motion that exists between femur, tibia, and patella. The patella is considered a sesamoid bone implanted within the tendon of the extensor mechanism. Arguably, the most important function of the patella is its role in facilitating extension of the knee by enhancing quadriceps efficiency through increasing the distance of the extensor apparatus from the axis of flexion and extension.128 The patella exerts a mechanical advantage by acting as a fulcrum, thus anteriorly displacing the line of pull and increasing the moment arm of the quadriceps muscle force in relation to the center of rotation of the knee. In doing so, the patella may enhance the force of extension by as much as 50% throughout the entire range of motion.285 In addition, the patella allows for the distribution of the reaction force on the femur by increasing the contact area during knee flexion. It also acts as a guide for the extensor mechanism by centralizing the divergent pull from the four muscles of the quadriceps and transmitting these forces to the patellar tendon. Together with the anatomic shape of the patellofemoral articulation, this protects the extensor apparatus from dislocating.
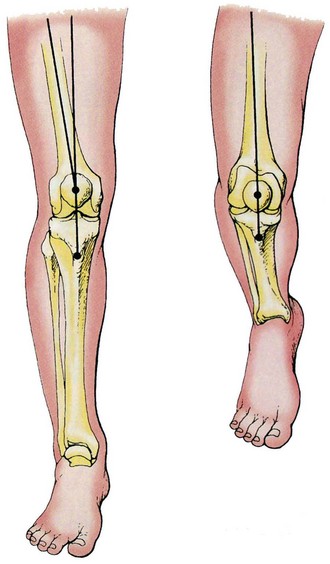
When the knee is extended, the tightening quadriceps pulls the patella upward until the upper border reaches beyond the femoral trochlea groove. So long as the line of gravity falls behind the center axis of the knee joint when standing upright, the quadriceps must contract to neutralize the rotatory effect of gravity on the knee, which would otherwise force it into flexion. As soon as the line of gravity falls within or in front of the knee, which usually occurs in full extension or hyperextension, the quadriceps becomes relaxed. The quadriceps apparatus, being oblique in its angulation toward the patella and patellar tendon, creates a line of pull with an outwardly directed horizontal component when contracted. The angle between the line of pull and patellar tendon is often referred to as the Q angle, which measures on average between 10 and 20 degrees (Fig. 113-1).91 In coronal and axial planes, this gives rise to a tendency of the patella to slip outward over the lateral femoral condyle, giving a resultant force in the lateral direction.92,316 To offset this propensity, the lateral condyle projects farther forward, whereas the fibers of vastus medialis that secure the patella medially extend farther distally compared with those of the vastus lateralis.285 In addition, the tibia derotates during the first 30 degrees of flexion, essentially reversing the screw-home mechanism and significantly reducing the Q angle, which in turn also decreases the lateral vector.35,92,111,203 Because of a lack of mechanical engagement and the presence of lateral force vectors, the patella is most vulnerable in the early flexion range. Even at 30 degrees of knee flexion, the patella will not have fully engaged into the trochlea groove and the effect of the Q angle may not have neutralized. Walker316 has conceded that in the midrange of flexion, the condition for lateral stability of the patella is that the angle of inclination of the lateral trochlear groove is larger than the Q angle.
Contact Areas
With the knee in full extension, the patella is usually out of contact with the trochlear groove. Depending on the length of the patellar tendon, the patella is drawn into the trochlea from a slight lateral position and gains contact with the femur between 10 and 20 degrees. The contact begins with the inferior margin of the patella and moves proximally as flexion proceeds. Beyond 30 degrees, the patella settles into the deepening trochlear groove, where it is further stabilized by the quadriceps and patellar tendon force. During flexion and extension, the patella presents an excursion of 5 to 7.4 cm in the sagittal plane, whereas the distance between the lower pole of the patella and tibial tuberosity remains constant.35,93,276
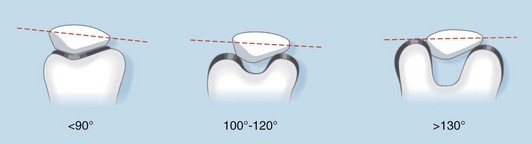
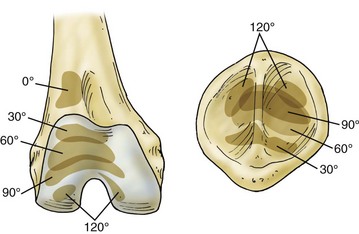
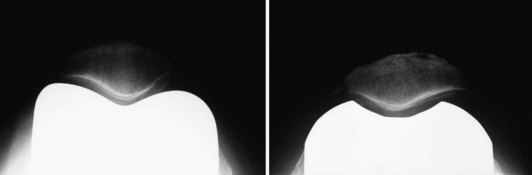
The patellofemoral contact area extends from the medial margin of the medial facet to the lateral margin of the lateral facet as a broad band of contact moving from distal to proximal.3,110,112,301 At 60 degrees of flexion, the contact is across the center, at 90 degrees of flexion the contact is toward the superior pole and, beyond 90 degrees, the patella, lying across the medial and lateral condyles, is forming two separate contact areas131,140 (Figs. 113-2 and 113-3). Ficat and Hungerford92 have described this movement of the patella in the coronal plane during flexion as a “gentle curve with its concavity facing laterally.” Studies of the tracking pattern of the natural patella have confirmed that the patella rotates as much as 15 degrees in relation to the femur at flexion angles beyond 50 degrees, tilts in a mediolateral direction in the axial plane, and undergoes medial displacement of up to 4° during early knee flexion, and lateral displacement of up to 8° during high flexion beyond 60°.156,247,309,310
In the transverse or axial plane, as seen on skyline radiographs, the patella is perfectly congruent with the trochlea, ensuring its medial and lateral stability. Longitudinal sectioning of the patella has confirmed that the patella adopts almost a flat surface in the sagittal plane, making it perfectly unconstrained as far as its anatomic form is concerned.142,166 The form of the patella provides stability against lateral subluxation but does not impede it from rocking around its transverse axis to the point at which the resultant of the PFJ reaction force is perpendicular to the contact surface.
As with the location of patellofemoral contact areas, the size of the contact areas is highly dependent on knee position. From 20 to 60 degrees of flexion, the average contact area increases linearly from approximately 150 to 480 mm2.3,302 It then remains almost constant up to approximately 90 degrees of flexion, after which a linear reduction occurs.112,139 Because of the drastically changed contact pattern beyond 100 degrees, when the patella leaves the trochlea, straddling the intercondylar notch, contact areas may fall well below 100 mm2 at full flexion (see Fig. 113-3). Subsequently, only a certain proportion of the retropatellar surface will be in contact with the femur at any one time. Matthews and associates196 have shown that on average only 19% of the patella-bearing surface is engaged at 30 degrees of flexion, 29% at 60 degrees, 28% at 90 degrees, and 13% at 120 degrees.
Biomechanics
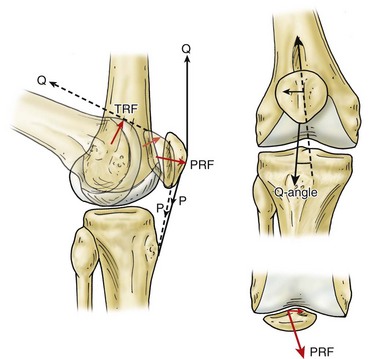
Much attention has been given to define the force transmission in the PFJ. For ease of calculation, it is sufficiently accurate to consider that these forces lie in a sagittal plane. The patellofemoral reaction (or compressive) force (PRF) is acting perpendicular to the articulating surface of the patella and is equal and opposite to the resultant of the patellar tendon and quadriceps forces (Fig. 113-4). With increasing flexion, the line of reaction moves upward, leading to an increase in PRF for the following reasons. As the angle between the patellar tendon and quadriceps becomes more acute, the resultant force vector increases. With knee flexion, effective lever arms of the femur and tibia increase, requiring greater quadriceps power to resist the flexion moment of the body weight (BW). Close to extension, the PRF is only about one third of the quadriceps force, whereas beyond 60 degrees of flexion, the patellar force is about 1.25 times the quadriceps force.316
The most important variable in the calculation of static forces is the distance between the line of body weight (center of gravity) and PFJ. Changes of posture in the sagittal plane (leaning forward or backward) will alter this distance and lead to substantial differences in static force transmission, whereas changes in the coronal plane will exert little influence.16,66 In full extension, the center of gravity usually falls anterior to the knee and moment arms become 0; hence, no forces will be acting on the PFJ. In this situation the body is instinctively balanced by compensatory deviations of its different parts creating a condition of unstable equilibrium. Whenever the line of body weight is moved away from the PFJ in a posterior direction, muscle activity and tension in the patellar and quadriceps tendon increase to maintain position, resulting in higher PRFs.
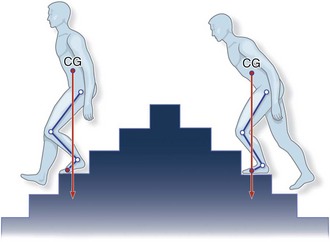
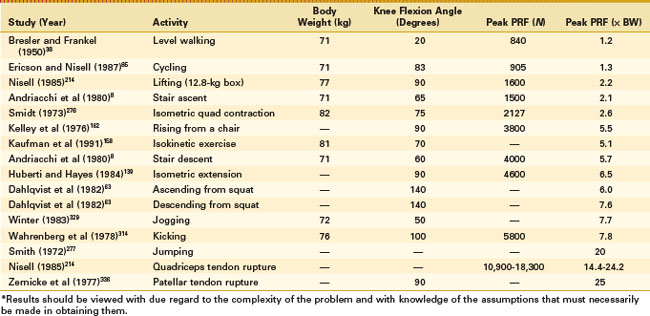
During normal activities requiring flexion under load, hip flexion is also present, thus bringing the center of gravity forward and shortening the femoral lever arm. This relationship is exemplified by the patient with quadriceps weakness who can rise from a chair by leaning forward, bringing the center of gravity closer to the knee. Similarly, there are significant differences in patellofemoral compressive forces when ascending and descending stairs (Fig. 113-5). Predicted force values for stair ascent range from 1.8 to 2.3 × BW, compared with those for stair descent of 2.9 to 6 × BW8,223 (Table 113-1). The increased values on descending are a result of the center of gravity being moved further backward behind the PFJ, as the body adopts a more upright position to maintain balance.17,18,261 Force transmission in the PFJ is therefore dependent on the relationship between the center of gravity of the body and knee flexion angle, and calculations should not be based on the length of the femur and position of the hip joint per se.16
The quadriceps tendon abuts onto the proximal aspect of the femoral trochlea in midrange of knee flexion, allowing compressive forces to become divided between the tendofemoral and patellofemoral contact areas.18,93,102,214 This phenomenon, described as the “turn-round” of forces, represents an elegant way of maintaining relatively constant unit load under a mechanical situation in which total load is increasing112 (see Fig. 113-4). The efficacy of the turn-round of the divided forces is dependent on the length and altitude of the patella, and it takes effect between 50 and 90 degrees of flexion.16 According to measurements obtained by Hehne,131 the contact area of the quadriceps tendon is significantly larger compared with the contact area of the PFJ. At 90 degrees, the quadriceps contact area was one to two times larger, at 120 degrees two to three times larger, and at 140 degrees three to four times larger than the patellofemoral contact area. Huberti and Hayes139 have calculated average tendofemoral reaction forces (TRFs) at 120 degrees of flexion as approximately 550 N, whereas PRFs at the same degree of knee flexion measured on average 1600 N, indicating a TRF-to-PRF ratio of 1 : 3. This may partly explain the higher frequency of chondromalacia in patella alta, because tendofemoral contact may be eliminated or substantially decreased, creating an increase in PRF.148,168
Static measurements of PRFs show an almost linear increase, with values ranging from 0.2 × BW at 10 degrees to 12.9 × BW at 135 degrees.* In vivo PRFs vary and are dependent on the type of activity performed. Predicted force values range from 0.6 × BW for level walking to 7.7 × BW for jogging and 20 × BW for jumping.158,214,223,277,329
Reaction forces during cycling are generally lower than those generated through daily activities and most other athletic activities. Ericson and Nisell85 were able to show that the magnitude of joint forces is almost independent of body weight, but increases with workload and reduced seat height. TRF rose to 295 N at 108 degrees of knee flexion, whereas PRF peaked at 83 degrees with 905 N. Anterior knee pain (AKP) during cycling is therefore more likely to occur if the seat position is kept low, because this will increase knee flexion angles throughout all stages of the revolution.73 Cycling should be considered a recommended activity for most patients following knee arthroplasty, especially those who are obese, but proper attention should be given to the level of workload and seat height (see Table 113-1).
When considering the magnitude of PRF, it has to be remembered that this force acts through an area that varies with knee flexion.190,301,316 Thus, an increase in PRF does not necessarily assume an increase in patellofemoral pressure. The patellofemoral contact area is small near full extension of the knee, indicating that patellofemoral pressure is higher for the same magnitude of PRF. Subsequently, patellofemoral pressure near extension may be relatively high, although the compressive force appears to be comparatively low.214
To obtain a rough estimate of the resulting contact pressures in the PFJ, the mean pressure is calculated by dividing patellofemoral force values by the patellofemoral contact area. Calculated patellofemoral contact pressure values, dependent on activity and knee flexion angle, range from 1.28 to 12.6 N/mm2.139,196 A man of 71 kg (696 N) climbing stairs would generate a patellofemoral compressive force of 1754 N equivalent to 2.5 × BW and experience patellofemoral pressures between 3.73 and 6.87 N/mm2. Women have smaller knees and hence shorter patellar tendon moment arms than men. Subsequently, the PRF increases by up to 20% for the same knee-extending moment, which would explain the somewhat higher frequency of patellofemoral disorders in women.214
Denham and Bishop66 have shown that the PRF exceeds the tibiofemoral reaction force in angles above 25 degrees. At almost full knee flexion, these values rise to almost 150% of the forces passing through the tibiofemoral joint. It is therefore not surprising that the cartilaginous cover of the patellofemoral articulation is the thickest in the body and allows the transmission of forces to the subchondral bone in such a way that the pain threshold of the richly innervated bone is not surpassed.92 The articulating surfaces are able to adapt to the changing surface contours because of the viscoelastic properties of cartilage, which allow for its deformation under load and subsequent increase in pressure-transmitting area. This process is time-dependent and pressure values will thus be different for short-term and long-term loading. The measured values of patellofemoral pressure should therefore be regarded as reference values only, because pressure-transmitting areas of the PFJ increase with increasing load and duration of loading.16,110,131,196,302 This may explain why peak stresses of up to 20 times body weight can be tolerated without causing lasting damage, because they are applied for only very short periods of time, whereas long-term application of such loads would invariably lead to cartilage breakdown.
History of Patellar Resurfacing
The earliest types of total knee arthroplasties were pure tibiofemoral replacements, primarily designed to treat severe axial deformities and intractable knee pain in patients affected by tuberculosis or rheumatoid arthritis.106,273,319 The procedure was seen as an alternative to arthrodesis and performed in patients of extremely low demand, for whom any improvement in pain relief or mobility level was considered a success.321
The PFJ remained largely ignored until the end of the 1960s, with most hinged knee arthroplasties failing to provide an anterior femoral flange as an articulating surface to accommodate for physiologic patellar tracking.132,273,319 In these earlier designs, the patella usually impinged with the anterior ridge of the proximal margin of the femoral component, which was not countersunk to the level of the retained part of the proximal trochlea.86,191,234,321 This incongruity between prosthetic femoral and native patellar surface created an articulation of poor geometry, which often led to patellar erosion and deformity, prompting some surgeons to promote patellectomy actively as part of the surgical procedure.335 Through the increase in patellofemoral complications and extensor mechanism failures, clinicians became aware of the shortcomings of available knee implants in providing for normal patellofemoral function. Design changes were introduced based on proximal extension of the femoral component and creation of a trochlear groove in an attempt to emulate the anatomic shape of the femur, whereas the patella itself maintained its “Cinderella” status.62,206,263,270 A case in point was the Duocondylar prosthesis, which did not provide for the PFJ and yielding mixed results, with many patients suffering anterior knee discomfort. Changes in the design through the addition of a trochlear flange improved clinical outcome results dramatically by allowing the natural patella to articulate with the femoral component throughout the entire range of flexion.
Continuing disenchantment with the unpredictability of clinical results, however, encouraged some clinicians to experiment with replacement of the retropatellar surface.3,120,123 Hanslik,123,124 in 1969, reported the use of a modified version of the McKeever patellar prosthesis made of high-density polyethylene, which was combined with the hinged arthroplasty by Young.335 Hanslik was critical of the replacement designs available at that time and stressed the importance of patellar preservation for enhancing the functional outcome. Between 1969 and 1973, 46 TKAs with a patellar prosthesis were implanted, mostly for end-stage osteoarthritis. Short-term results indicated that the great majority of patients were walking unaided, with only slight or no pain.
The first recorded patellar resurfacing combined with a nonconstrained condylar-type replacement arthroplasty was performed by Groeneveld and colleagues in 1970118–120 (Fig. 113-6). They adopted the low-friction principle popularized by Charnley when combining a femoral mould arthroplasty with tibial polyethylene disks and a three-pegged anatomic polyethylene patellar component. At 2-year follow-up, 64% of patients with a replaced patella had excellent or good results compared with 46% in whom the patella was left unresurfaced. The authors expressed uncertainty about the long-term survival of the patellar implant and thought that patellar resurfacing should be reserved for cases of persistent pain and only used in combination with a patella-friendly femoral component.
Gunston and MacKenzie121 developed a patellofemoral arthroplasty designed to work in conjunction with the polycentric knee system in response to the inability to alleviate AKP, despite patellectomy. A stainless steel patellar button articulating with a grooved polyethylene track placed into the trochlea was used between 1973 and 1976 in several knees, with satisfactory initial results. Gunston was, however, aware that the additional prosthetic components would increase the possibility of complications and therefore urged it not to be used indiscriminately.
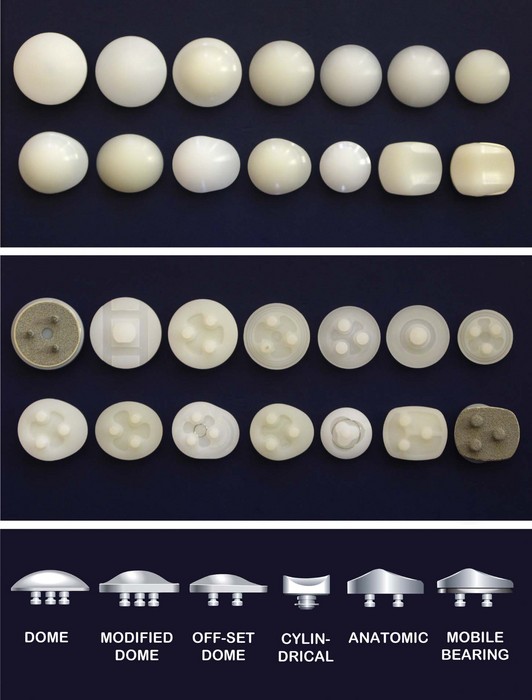
At the Hospital of Special Surgery, Insall, Ranawat, Scott, and Walker started to develop the duopatellar and total condylar prosthesis, the first complete prosthetic system allowing for optional resurfacing of the patella.152,235,318 A dome-shaped polyethylene patellar design was chosen because of its simplicity and to prevent binding in the femoral groove. Their first tricompartmental total condylar replacement was implanted in October 1974 by Ranawat et al.3,150,235 Other designs followed and, by the beginning of the 1980s, almost all available knee replacement systems had provisions for patellar resurfacing.117,141,173,318
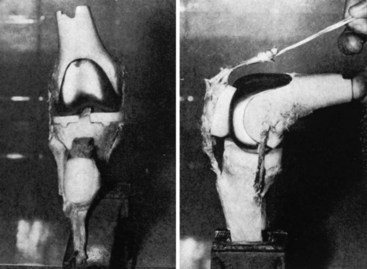
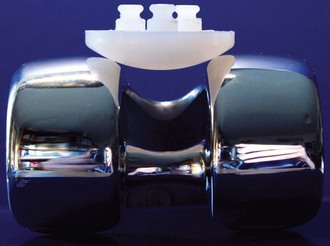
Many different patellar surface designs became established, but despite the relative clinical success of cemented, all-polyethylene patellar components, metal-backed patellar implants were introduced in the early 1980s. Metal backing was initially applied to polyethylene acetabular and tibial components to improve load transfer and bending resistance, in addition to allowing for the application of porous metal surfaces for biologic anchoring.20,243,317 Concerns about the failure of cemented prosthesis through loosening and bone resorption, erroneously thought to be caused by an adverse biologic response to methylmethacrylate, added to the enthusiasm for cementless fixation and the use of porous-coated patellar implants.141,327 The principal advantages of metal backing, however, were applied to the patella without clinical justification.236 Problems of polyethylene deformation and wear, fatigue fracture, and component dissociation through locking mechanism failure led to the rapid demise of the metal-backed patella, which by the end of the decade was almost universally abandoned22,236,258,292 (Fig. 113-7).
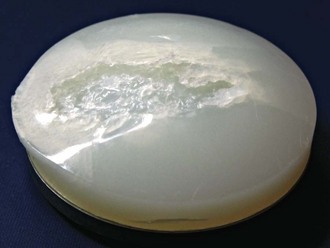
Figure 113-7 Retrieved patellar component showing severe polyethylene wear and delamination.
(Courtesy Professor Wolfgang Plitz, Laboratory of Biomechanics, Ludwig-Maximilian University, Munich, Germany.)
All-polyethylene dome-shaped patellar components have since experienced a renaissance and have been used in conjunction with the vast majority of currently available knee arthroplasties. Their obvious disadvantages appear to be outweighed by their simplicity in design, ease of application, and relative forgiveness. Improvements in patellofemoral implant design and geometry have led to a reduction in PFJ-related complications but have so far been unable to eradicate them completely.59
Patellar Implant Design
Matthews and colleagues have assessed the load-bearing characteristics of the patellofemoral joint and remarked that “high patellofemoral load values, small patellofemoral contact areas, and resultant high stress magnitudes indicate the need for caution in the design and development of a patellofemoral component for total joint replacement prosthesis.”196 These comments remain applicable even today, with retrieval analysis of patellar components and the significant failure rate of metal-backed patellar designs underscoring the extreme mechanical environment in which these implants are expected to perform (Fig. 113-8).
It should be remembered that patellar tracking, contact area, and pressure distribution are significantly different between native and prosthetic knees.146,288 The configuration and mechanical features to be considered in the design of the prosthetic PFJ should include functional range of motion in multiaxial planes, stability, fixation, dimensions, load transfer areas, and materials.117 A successful patellofemoral articulation must be designed to function under high-stress conditions, over a long period of time, because ground reaction, gravitational, ligamentous, and muscular forces all act to produce significant compressive, shear, and torsional loads. Thus, both design and materials used must at least be compatible with mechanical forces generally encountered during daily activities.
Patellar and femoral components in TKA are inextricably linked and function as a unit. The configuration of this unit has been a matter of ongoing debate, indicating that the ideal combination is yet to be determined. For example, increasing the congruency of the patellofemoral articulation reduces peak stresses on the surface level of the components but, in turn, increases shear stresses at the patellar fixation site. From a wear point of view, an increase in component conformity would appear advantageous.21 Overconstraining the joint, however, is incompatible with secure fixation and freedom of motion. It is therefore reasonable to suggest a compromise solution that provides partially conforming surfaces that may satisfy reasonable motion, laxity, and stability between patella and femur. This concept of partial patellofemoral conformity has been incorporated successfully into most knee implant systems, but some mobile-bearing devices have defied science and have performed well, despite highly congruent surface geometries.43,153,161
The myriad of patellar components currently available reflects the lack of consensus with respect to the ideal design (see Fig. 113-8). Persistent attempts to implement design changes are often influenced by reported complications, such as the high failure rate of metal backing. Such changes are often based more on the absence of a satisfactory alternative than an indication that continued refinements are leading to improved results. Currently, central fixation lugs are less common because of the increased risk of patellar fracture associated with this particular design.58,267 Fixation lugs placed peripherally are subject to less stress than lugs placed centrally, especially if oriented in a transverse direction.55,170
Articular surface geometries of patellar components vary greatly but can be classified into four basic shapes—convex or dome-shaped, modified dome-shaped with peripheral concavity (also known as Mexican hat, sombrero type), cylindrical or saddle-shaped, and anatomic164 (see Fig. 113-8). Every implant design bears particular advantages regarding conformity, stability, forgiveness, and wear pattern, with none ultimately being superior. However, advantages attributed to a particular design, such as the dome-shaped patella, should not be generalized to all domes because the behavior of a specific patellar component is directly dependent on a number of variables, with the surface geometry of the mating femoral component being the most important.* Apart from component positioning and alignment, other factors, such as patient demographics and clinical function, will influence the performance and longevity of the PFJ.129
Dome-Shaped Patella
The great majority of currently available patellar components are of the all-polyethylene dome-shaped type (Fig. 113-9; see also Fig. 113-14). Dome-shaped components usually articulate congruently with the trochlear groove in extension but may be exposed to high stresses and point contact in flexion, when the patella comes into contact with the convexities of the femoral condyles. Some of these problems have been addressed successfully through design adaptations of femoral condylar and trochlear geometries. Extension of the trochlear groove concavity onto the inner portion of the femoral condyles has allowed for an increase of patellofemoral congruency in flexion. In addition, the round-on-round shape of the articulation permits patellar tilt to occur without excessive edge loading, a problem associated with modified dome-shaped and anatomic patellar devices. However, failure of cemented, all-polyethylene dome-shaped patellar components is not uncommon; this has been attributed to the exposure of increase shear stresses in vivo, especially in malpositioned components.22,98,137,331
Modified Dome-Shaped Patella
In an attempt to increase the contact area in flexion, the standard dome patella was modified by adding a concave circumferential extension, allowing it to match the curve of the femoral condyles in the frontal plane more closely (Fig. 113-10). The modified dome-shaped patella, also known as Mexican or sombrero hat, improves the articulation with the convexities of the femoral condyles in the intercondylar notch beyond 90 degrees of flexion by increasing metal to plastic contact. Hsu and Walker136 have compared the wear pattern of the all-polyethylene dome and modified dome-shaped patellar components in an experimental study. They found that increasing the conformity in the frontal plane increases the life of the component on a wear simulator by more than 20 times. The authors, however, raise concern that the amount of conformity that is acceptable must be considered in relation to patellar motion path, which is affected by rotation, tilt, and sideways shift.247,309
Anatomically Shaped Patella
Prostheses with an anatomic surface profile have lateral and medial facets and bear certain theoretical advantages. They maximize the contact area, thereby minimizing contact pressures, and create a more conforming articulation, thus decreasing the risk of subluxation.43,44,141 A variety of anatomically shaped patella implants have been available over the years, including a mobile-bearing variant (Fig. 113-11; see Fig. 113-8). Unfortunately, however, anatomically shaped patellar prostheses are more sensitive to malpositioning and hence more difficult to implant.185 Thus, only a few anatomic patella implants remain commercially available, with most being discontinued in favor of more forgiving designs.
Cylindrical Patella
The cylindrical or saddle-shaped patellar component occupies a fringe position in TKA and is offered by only a few manufacturers (Fig. 113-12). The initial idea was developed by Freeman et al in the late 1970s99,100; they attempted to combine a high level of congruency and large contact area throughout the flexion range, with freedom of motion in the coronal plane but without compromising component stability. Because of the design specifics, the patella becomes highly dependent on a close-matching geometry of the femoral component in the sagittal plane, hence requiring a femoral trochlea of single radius.167 The diameter of the patellar component is reduced to 25 to 30 mm, allowing the implant to be recessed into the patella, similar to the inlay technique (see later). Subsequently, the remaining patellar rim participates in articulating with the femoral component and further contributes to stress dissipation. The patellar implant possesses a central peg with a collar and can be used with or without cement. If left uncemented, the implant retains the ability to self-center and to rotate, as has been observed in revision situations for reasons unrelated to the patella.14 Although fibrous ingrowth may eventually halt this process, the implant is likely to have adopted favorable alignment by this time.308 Despite its relative rotational constraints, the design concept has provided patellofemoral survival rates of 96% to 98.4% at 10 years.188 Concerns that preservation of cartilage at the patellar rim may negatively affect pain perception has so far not been confirmed.188
Mobile-Bearing Patella
A different biomechanical concept was conceived with the anatomically shaped, mobile-bearing, metal-backed patella43,44 (see Fig. 113-11). The design rationale is based on the same principle as that of rotating platform tibial components. The clinical performance record of mobile-bearing patellae has been surprisingly good. Although not generally affected by complications otherwise associated with metal-backed prostheses, failures caused by fracture, wear, and dissociation of the polyethylene element have been described.138 Reported survival rates of up to 99.5% at 12 years are attributed to the high conformity and low stresses permitted by the mobile-bearing articulation.153 The absence of significant backside wear in mobile patellar bearings has led some clinicians to believe that these devices may not actually rotate in service. It has been speculated that the advantages of mobile-bearing patellae may be their ability to compensate for variations in surgical alignment by rotating into a preferential position after engagement with the femoral component, and simply to remain there.200
Metal-Backed Patellar Components
Metal backing became fashionable in the early 1980s. It has since largely been abandoned, with the exception of some uncemented fixed-bearing designs (e.g., Townley TKO System, Biopro, Port Huron, Minn; Foundation Knee, DJO Surgical, Austin, Tex; Natural Knee II, Zimmer, Warsaw, Ind) and rotating platform anatomic designs (e.g., LCS, DePuy Orthopaedics, Warsaw, Ind; AMC, Corin USA, Tampa, Fla; ROCC, Biomet, Warsaw, Ind; Buechel-Pappas, Endotec, Orlando, Fla). Adding a stiff metal layer to the back surface of the polyethylene patella was thought to improve load transfer and protect the fixation interface.20,317 To accomplish the addition of metal backing to the patellar component without increasing its overall thickness, substantial reduction in polyethylene thickness is required.21 These changes in implant design create an increase in contact stresses because of the rigidity of the metal substrate. Subsequently, polyethylene deformation through cold flow, fracture, and dissociation of the polyethylene layer from the metal backing have been observed in retrieved components96,180,292 (see Fig. 113-7).
Kinematics and Biomechanics of the Patellofemoral Joint in Total Knee Arthroplasty
The mechanical environment of the replaced PFJ differs from the natural knee. The contact area of the prosthetic PFJ measures, at best, no more than 40% of the contact area established for the native knee.164,295,332 Measurements obtained experimentally vary widely and depend on the technical setup and level of compressive force applied during testing. For dome-shaped designs, contact areas range from 13 to 162 mm2, with the highest values usually observed between 90 and 120 degrees of knee flexion.207 Values for anatomic, cylindrical, and modified dome-shaped patellar components also vary but, because of the increased level of conformity, are generally higher when compared with their dome counterpart.127,193,287
One of the major challenges for the resurfaced patella is its resistance to wear, despite being biomechanically disadvantaged by having a small contact area through which high contact pressures are transferred. Patellar components are exposed to compressive and shear forces during knee flexion, increasing their risk of damage and failure, especially in patients of high demand and with increased postoperative flexion.79,217 Up to 75 degrees of knee flexion, the contact area between the prosthetic patella and femur is relatively large and contact pressures generally low. Beyond this point, bifurcation of patellofemoral contact creates two distinctly separated contact areas on the medial and lateral extremities of the articulating surface of the patella, straddling the intercondylar notch131 (Fig. 113-13). The transition from a one-point to a two-point contact is associated with an overall decrease in contact area, whereas patellofemoral compressive forces and contact pressure increase almost exponentially. The direct influence of this transition in contact area on the wear pattern can be observed in retrieved patellar components, which often demonstrate deformation and development of characteristic facets at the margin of the polyethylene patellar surface.136,198,200 Such changes may be described as a wearing-in phenomenon, as it demonstrates the ability of the patellar component to accommodate nonconformity by creeping in ways to reduce contact stresses (see Fig. 113-15).
We know that in level walking, the PFJ is exposed to compressive forces of up to 1.2 × BW, whereas activities such as descending stairs and rising from a chair may create forces up to 5.7 × BW.38,162 The intensity of these stresses is directly influenced by the contact stress at the surface of the bearing, which is in part largely a function of implant design and surface conformity. During level walking, an activity most frequent for most patients, lower patellofemoral forces and more central contact areas indicate that failure of the patellar component is unlikely to occur. In contrast, the higher ranges of flexion seen when ascending and descending stairs and rising from a chair accompanied by high patellofemoral forces, and therefore are more likely to lead to patellar component wear and subsequent failure8 (see Figs. 113-5 and 113-13).
Matsuda and coworkers193 have assessed patellofemoral contact stress and contact area in TKA by comparing the native knee with a dome-shaped nonconforming patella, anatomically conforming patella, and unresurfaced patella. Values for patellofemoral peak contact stress and contact area remained almost at the level of the native knee if the patella was left unresurfaced. Following patellar resurfacing, patellofemoral contact stress rose beyond yield strength for ultra–high-molecular-weight polyethylene (UHMWPE), with an average increase of 200%, whereas the patellofemoral contact area decreased on average by 60%. There was no statistically significant difference between conforming and nonconforming patellar components; thus, neither design assumed superiority. It was concluded that although the effect of metal action on cartilage was uncertain, the option of leaving the patella without a prosthetic component remains an attractive one, especially if the patella is well preserved. In a similar study, McLain and Bargar198 reported a threefold rise in anterior patellar strain at knee flexion angles beyond 30 degrees in TKAs with dome-shaped patellar components when compared with the native knee.
Stiehl and associates290 have assessed patellar kinematic pattern and demonstrated that patellar axis rotation, which compares the angle between the patellar tendon and sagittal axis of the patella, increases with flexion in TKAs beyond the levels observed in normal knees. The contact position between the dome-shaped and anatomically shaped patellar components showed greater variability compared with the normal knee, with the average contact position for the resurfaced patella lying more superior and tilt angles being significantly increased. The kinematic behavior of an anatomically shaped or unresurfaced patella more closely resembled the native knee, compared to that observed with dome shaped patellar designs.
The effects of the three-dimensional movement path on domed, modified domed, anatomic, and rotating patellar designs were investigated by Kim and associates163 in a cadaver model. They exposed specimens to mediolateral tilt, shift, and rotation and measured changes in contact area. Under optimal tracking conditions, contact areas of the dome-shaped patella were significantly smaller compared with the modified dome and anatomic designs. When exposed to three-dimensional movements, however, the contact areas of the dome-shaped patella were significantly greater, indicating enhanced forgiveness regarding patellar malpositioning, whereas modified dome-shaped and anatomic components appeared more sensitive to patellar malalignment (Fig. 113-14).
The level of conformity between femoral and patellar components influences the joint’s ability to tolerate natural variations in motion, potentially limiting the patella’s ability to follow its natural movement path.247,289,290,309 If such motion is insufficient, shear forces will arise. Toleration of these variations in motion hence requires a level of nonconformity in order to establish “equilibrium of forces.” High conformity within the patellofemoral articulation clearly limits flexibility in terms of component positioning. Malalignment is known to impart additional shear forces on the patella and its fixation site increasing the risk of subsequent component failure. This has been shown by MacCollum and Karpman,185 who reported complications in 18 of 75 fixed-bearing anatomic patellar components, which included subluxation in 10, fracture in 5, tendon rupture in 2, and implant loosening in 1.300,306
Potential advantages of low contact stresses in conforming designs may be offset by an increase in constraint, resulting in deleterious effects on patellar wear and fixation. This typically leads to a compromise in which the conformity and therefore contact area are reduced to avoid overconstraining the joint. However, the question of how much contact area to sacrifice and how to best achieve that compromise remains unanswered. As a general trend, most clinicians shy away from anatomic patella implants and, for ease of application, prefer the more forgiving dome-shaped designs.235,252
Material Science of Ultra–High-Molecular-Weight Polyethylene in Patellar Implants
Because of the great disparity between moduli and strength of cobalt-chrome alloys on one hand and UHMWPE on the other, wear is primarily observed on the polymeric side of the prosthetic patellofemoral articulation (Fig. 113-15; see Fig. 113-7). Notwithstanding its limitations, UHMWPE has evolved as the material of choice for the patellar component, based on the low-friction principle of Charnley. Mechanical properties of UHMWPE are far from being ideal, with yield strength being affected by the level of molecular weight, degree of cross linking, and sterilization method. Uniaxial yield strength of UHMWPE, which equals the lowest stress at which the material undergoes plastic deformation, is estimated at 21 to 23 MPa (1 MPa = 1 N/mm2), according to manufacturer’s guidelines.21,59,248,284 Some manufacturers have expressed concern if such stresses are applied on a regular basis. For machinery applications, repeated maximum contact stresses of no more than 10 MPa have now been recommended, a value identical to the yield strength estimated for articular cartilage.245 These values are based on room temperature, whereas the strength of UHMWP may be reduced by up to 25% at body temperature; therefore, values of 5 MPa may be more appropriate for use in vivo.43
In vitro contact stress analysis has confirmed that all-polyethylene dome-shaped patellar components produce contact pressures from 20 to 30 MPa in extension, increasing to 36 to 100 MPa at 90 to 120 degrees of knee flexion, therefore exceeding the yield strength of UHWMPE by up to 400%.145,164,200,332 Anatomically shaped rotating platform patellar components produced significantly lower values, mostly remaining below the yield strength of UHMWP.59 Wear simulator studies have further confirmed that congruent patellar components (modified dome-shaped and anatomic) exhibit significantly lower rates of creep and wear than dome-shaped designs, again indicating that conformity is critical to wear resistance and protection against post–yield deformation134,136 (see Fig. 113-15).
Viscoelastic properties of surface cartilage allow for its deformation under load and subsequent increase in pressure- transmitting area. Because of differences in elastic modulus between cartilage and UHMWPE, the prosthetic patella, however, has limited ability to change its surface contact area through variations in patellofemoral load.26,131,136,200 Xu and associates332 were able to demonstrate the effect of patella resurfacing on contact area and pressure in cadaveric knees. The mean contact area between 30 and 120 degrees of flexion in the nonresurfaced PFJ ranged from 70 to 150 mm2, whereas peak patellar contact pressures did not exceed 12 MPa. Once resurfaced, the mean contact area decreased almost 10-fold to 10 to 15 mm2, creating a dramatic increase in patellar contact pressure values of 50 to 100 MPa. Steubben and associates287 have carried out biomechanical studies assessing patellar surface contact area, compressive forces, and contact pressure using different prosthetic models.54,207 They found that patellofemoral contact pressure values at knee flexion angles beyond 45 degrees exceeded polyethylene yield strength in all tested components, with peak measurements of up to 75 N/mm2 (75 MPa). Results were not a true function of contact area and contact pressure, signaling the importance of design features in the dissipation of contact forces across the PFJ.
Greenwald and colleagues have measured the distribution of patellofemoral surface stresses by mapping areas above and below the tensile yield strength of polyethylene.116,287 All implants—whether dome-shaped, modified dome-shaped, or anatomic—demonstrated material yielding over their range of flexion. The results indicated the importance of appreciating the location of the yield areas within a given patellar component, because rim-loaded contact areas above yield are more likely to deform and wear. It may thus be conceivable that polymer integrity is not determined primarily on the size of the contact area, but rather on the extent of the surface within this region, which exceeds yield conditions.
Subsequently, contact stresses above the yield strength do not necessarily lead to catastrophic failure, as demonstrated by the large number of relatively undamaged retrievals. As highest values of contact stress are experienced during flexion, variations in a patient’s activity may not expose the patellar component to large cyclic loads frequently enough to accumulate damage. McNamara and coworkers200 have considered the constraining effect of the surrounding polyethylene as responsible for this phenomenon. Yield in polyethylene is characterized by plastic deformation rather than brittle failure, which explains why nonconforming patellar components are capable of wearing in.26 Such surface adaptation has been demonstrated to produce characteristic facets at the margin of the patellar component, increasing the contact area particularly in flexion when there is least congruency between the patella and condyles136 (see Figs. 113-9 and 113-15). Although reduction in contact stresses of 23% to 58% through increased conformity have been reported, contact stress values remain above the UHMWP yield strength.59,127 Elbert and associates79 were surprised that despite reduction in overall component thickness, stress values did not increase. In their opinion, changes in geometry and contact area dominate the response of the deformed component, overriding the effect on the stresses of the decreased thickness. Analysis of Von Mises stress, a yielding criterion based on a combination of principle stresses occurring within the material, has revealed that most stresses above yield strength occur 1 to 2 mm below the articulating surface area in the newly manufactured component; however, in retrieved components, Von Mises stress remains near yielding through the depth of the implant.207,328 Because of subsurface stresses, permanent deformation may be expected to continue, even when the component has worn in. Collier and associates59 have noted that all-polyethylene patellar components do not solve this problem because of distinct biomedical and biomechanical disadvantages of UHMWPE as a bearing surface. In the absence of a suitable alternative however, UHMWPE is here to stay, at least for the foreseeable future.
Femoral Component Design
The patella, whether native or prosthetic, cannot be considered separately because it works in direct partnership with the femoral component. Contact areas are highly dependent on the congruency of the PFJ articulation at all angles of knee flexion, whereas motion constraints of the patella are terminated by the surface geometry of the femoral component and by the balance of soft tissue forces. Bartel and associates20 have demonstrated the importance of conformity in prosthetic design to increase contact area and decrease contact stress. Current femoral prostheses display a wide variation in design features in regard to length, depth and orientation of the trochlear groove, sagittal radius, and axial geometry.75,297,334 Anatomically shaped femoral components appear to be particularly suitable if articulating against the nonresurfaced patella, which will be referred to as patella-friendly from this point on161,296 (Fig. 113-16). They provide for increased conformity between the native patella and femur and demand minimal biologic patellar remodeling.43,161,325 Nonanatomic designs are those in which the trochlear groove is concave spherical and designed to accommodate a nonanatomic patella, usually of dome-shaped design. Proximal extension of the femoral flange will help capture the patella during early flexion, whereas extension of the concave shape of the trochlear groove onto the inner aspects of the femoral condyles will allow for increased metal to plastic contact at higher flexion angles (see Figs. 113-10 and 113-14).54,56,227,264,297
The effect of valgus alignment of the trochlear groove compared with symmetrical designs on shear stresses has been investigated with mixed results. Asymmetrical trochlear groove designs are thought to provide earlier patellar capture through prominence of the lateral flange and to decrease the predominant valgus force vector, thus reducing patella shear.75 In some reports, reduction in lateral shear forces of up to 10% were observed, whereas others saw no effect or even a shift toward the generation of medial shear forces.56,227,297 The exact clinical advantages of asymmetrical designs have remained largely theoretical, with no compelling clinical proof of their effectiveness.318
The importance of femoral component design and its influence on patellofemoral performance have been highlighted by Theiss and associates297 based on the clinical results of two arthroplasty designs with distinct differences in trochlear geometry. A 14-fold decrease in patella-related complications was observed when using a patella-friendly design with an extended anterior flange and a deeper and wider trochlear groove. It was concluded that the more proximal capture of the patella in a deeper groove, with more gradual proximal to distal transition, appears advantageous in reducing patella morbidity. Yoshii and associates334 used an experimental model and demonstrated that specific femoral design changes, including deepening and distal extension of the trochlear groove, improve patella tracking compared with an unmodified femoral component.
Lateral forces acting at the patellofemoral articulation increase with knee flexion14 (see Fig. 113-4). The magnitude of the lateral forces, which are dependent on valgus alignment, Q angle, and soft tissue balance may, if excessive, cause patellar subluxation and contribute to component failure. Steubben and associates287 have investigated the resistance offered to lateral subluxation of the resurfaced patella by defining the intrinsic lateral stability of various patellofemoral designs. They found that the forces required to cause lateral displacement were at or above those measured for the native knee, and highly dependent on the interaction of condylar and patellar surface geometry. Their results highlighted that appropriate design changes can significantly increase resistance to patellar subluxation.
Unresurfaced Patella
Following bicompartmental knee arthroplasty, the nonresurfaced patella becomes exposed to the metallic surface of the femoral component. Because of differences in the modulus of elasticity, the articular surface of the patella must adapt to the geometry of the opposing surface by bedding in.161 This process of remodeling, which has been termed stress contouring, produces a gradual adaptation of the retropatellar surface and subchondral bone plate to the trochlear shape.280 Keblish and associates161 have noted that minimal remodeling is required if the patella is exposed to an anatomic design with a constant radius of curvature and uniform femoral geometry, whereas excessive remodeling is observed in nonanatomic designs (Fig. 113-17). The remodeling process is time-dependent and not seen on axial radiographs much before 2 years after implantation.
Tanzer and associates296 have studied the effect of femoral component designs on the contact and tracking characteristics of the unresurfaced patella in TKA. They noted substantial alterations in patellofemoral contact areas, contact pressures, and tracking at higher flexion angles when the native patella was articulating with a prosthetic femoral component. Although the percentage of patellofemoral contact area compared with the native knee is markedly reduced with increasing knee flexion, with measured values of 79% at 60 degrees, 69% at 90 degrees, and 65% at 105 degrees, it remains well above those measured for the prosthetic patella.
The surface geometries of some prosthetic femoral components, particularly those of posterior-stabilized design, appear incompatible with the native patella, because the apex of the retropatellar ridge may impinge on the prosthetic intercondylar notch beyond 90 degrees of knee flexion. Patellar deformation and wear are likely consequences and, in the case of significant patellar tilt, displacement of the patella into the notch becomes possible.198 Distal extension of the trochlea and shortening of the intercondylar notch have been shown to safeguard patellar support beyond 90 degrees of knee flexion.334 Such design modifications are therefore important if one considers leaving the patella unresurfaced. Most current femoral components present a surface geometry designed to articulate with a designated patellar component but are ill equipped to accommodate the native patella. Specific efforts are required to improve patellar kinematics by creating a femoral component that conforms to the normal trochlear and intercondylar notch topography, and that takes the geometry of the native patella into account.325 Only then would we be in a position to offer prostheses dedicated to be used with the native patella, compared with the mostly inadequate femoral designs currently available.
Effect of Cruciate Retention or Substitution
Moment arms affecting the patellar are dependent on the distance between the PFJ and the axis of flexion and extension of the femoral component. They are increased if the axis is deviated posteriorly from its physiologic position. Femoral rollback facilitates this process and represents a characteristic feature of normal knee kinematics. Increased rollback effectively lengthens the patellar moment arm thus increasing the efficacy of the extensor mechanism. D’Lima and associates75 have investigated the influence of various degrees of posterior femoral rollback on patellofemoral compressive forces. Femoral rollback resulting from PCL preservation produced reductions in patellofemoral compressive forces of up to 7% throughout knee flexion, whereas the effect in PCL-substituting devices only became noticeable after cam-post engagement, with a maximum effect recorded at 85 degrees of knee flexion. Miller and colleagues,205 in an earlier study comparing PCL-retaining with PCL-substituting arthroplasties, failed to note femoral rollback when the PCL was retained. They stipulated that the absence of the anterior cruciate ligament may render the PCL ineffective, which may explain the appearance of paradoxical movements (reverse rollback)75 observed on fluoroscopic investigation.68–70 Although PCL substitution kept patellofemoral forces close to the level of the native knee, a lateral release became necessary in 50% of knees, raising potential concerns about an increase in patellofemoral stress through ligamentous tension. This concept has also been expressed by Ranawat and Sculco233,235 who raised concern that femoral rollback, through a cam and post mechanism, as in posterior-stabilizing designs, or through a functional posterior cruciate ligament (PCL), may increase tensile forces across the patella in flexion. Overstuffing will tighten the extensor mechanism, and increase anterior patellar strain and PRF, with the likely consequences of loss of flexion, patellar implant failure, and fracture.78,204,235,303 Overall patellar thickness following resurfacing should therefore not exceed preoperative values. With regard to clinical outcomes, Waters and Bentley320 have assessed the occurrence of postoperative anterior knee pain in 327 cruciate-substituting and 147 cruciate-retaining TKAs, but found no significant difference.
Patellectomy and Alternatives
In the first half of the 20th century excision of the patella was heralded by most surgeons as the treatment of choice for debilitating and intractable anterior knee pain, patellar dislocation, and fracture.41,322 Most cases were usually affected by rheumatoid or osteoarthritis but removal of this “somewhat mysterious bone,” as described by Bruce and Walsmley in 1942,42 was also used for various other disabilities because of the apparent innocuous nature of the procedure. Some surgeons even went as far as removing the patella as part of a suitable alternative to displacement of the patella in arthrotomy of the knee; it is fair to say that especially those cases not affected by fracture or degenerative disease of the patella often ended up being worse.186 The general consensus on the appropriateness of patellectomy was so deeply entrenched in the surgical ranks that it prevented Bruce and Walmsley from completing their study on the subject. Both authors recognized the unjust globalized approach to patellectomy and its widespread abuse when they concluded their investigations by saying that “The whole question requires further study, however, and the outbreak of hostilities prevented this part of the investigation being pursued to a definite conclusion.”42 This conclusion, however was soon to come, in part through new scientific evidence but more so through discouraging clinical results disclosed in long-term follow-up studies.71,151
Anterior knee pain was a design-related complication common with early hinge arthroplasties. However, rather than addressing the problem by improving the design, the initial response was to promote patellectomy as part of the arthroplasty procedure.273,335 Insall and associates150 reported on four different prosthetic models used in the early 1970s, none of which made any provision to accommodate the patella. Out of 178 patients, 35 received a patellectomy at the time of arthroplasty and complaints of pain after patellectomy were as frequent from those patients as from patients in whom patellectomy was not performed.
Apart from failing to alleviate anterior knee pain reliably, removal of the patella creates added biomechanical disadvantages by decreasing the lever arm and extensor torque of the quadriceps mechanism, leaving most patients with measurable weakness.2,71,157,175,293 Haxton128 demonstrated that this decrease in lever arm is particularly noticeable in the more extended knee positions, when the patella would normally move out of the intercondylar fossa onto the femoral trochlea. Although patellectomy improves the efficiency of the extensor mechanism at higher flexion angles, in the daily flexion range, between 0 and 90 degrees, extensor power is greatly reduced.101,122 Increases in TRF and subsequent joint degeneration have also been reported following patellectomy.102 The surgeon contemplating patellectomy must thus be aware that the biomechanical effect of the loss of the fulcrum is the increased strength requirements of the quadriceps to provide extensor stability. Seriously disabled patients may not be able to develop sufficient quadriceps strength to provide this necessary extensor force.6
Today, patellectomy in knee arthroplasty patients has largely been abandoned as a routine measure and remains reserved for the treatment of severe comminuted fractures, advanced osteonecrosis, and tumors.2,238,240 In the treatment of comminuted fractures, total patellectomy is reserved for patients with loose patellar implants who present significant extensor lag and for whom reconstruction is unattainable.115 The general consensus has been to preserve the patella, even in revision situations in which severe bone loss may compromise its integrity. In situations in which less than 10 mm of bone remains, preservation of the patellar remnant avoids the need for reconstitution of the extensor mechanism and retains some of its residual lever arm.83
If patellectomy is performed, the technique of Compere has proven popular, with longitudinal shelling out of bone fragments and formation of a tube by suturing the medial and lateral edges of the rectus tendon together.61 Alternative measures are the use of biconvex, all-polyethylene patellar components, trabecular metal inlays, or bone grafting of the patellar defect.125,213,240 The biconvex patella requires at least 10 mm of bone stock and a 70% circumferential rim of bone equal to the thickness of the peripheral edge to provide for adequate cement fixation. Trabecular metal components allow for cementless fixation because of their osteoconductive properties. Medium-term results, despite a reported incidence of fracture through the patella remnant in up to 15% of cases, are promising. Trabecular metal facilitates excellent bonding to the patellar shell, even with less than 10 mm of bone remaining but, as with cancellous bone grafting, sufficient peripatellar blood supply is required to promote bone ingrowth.211 However, inferior results are to be expected if most of the fixation surface is composed of soft tissue and if the blood supply to the patella is substantially compromised.250
Surgical Technique
The Q angle, however, remains the most significant factor influencing patellar tracking. Any increase of the Q angle beyond normal limits will lateralize patellar tracking and could lead to patellar subluxation. Maltracking of the patella is often the manifestation of a technical error or a combination of minor errors and, according to Pagnano and Kelly,219 should be considered a red flag. Proceeding directly with a lateral retinacular release may improve patellar tracking but should only be considered once the surgeon is satisfied that there are no errors in rotational, translational, or angular alignment of the arthroplasty components.
Femoral Positioning
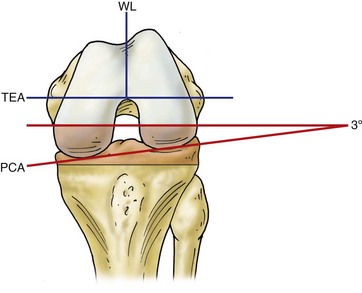
The patella is particularly sensitive to malrotation of the prosthetic implants of the femur and tibia.10,107 It is generally accepted that placing the femoral component in approximately 3 to 5 degrees of external rotation, relative to the posterior condylar axis, improves patellar tracking and proximal engagement.212 External rotation moves the trochlear groove toward the natural position of the patella, thereby relaxing the lateral retinacular structures and reducing the lateral force vector acting on the patella. Second, it also corrects any mismatch in the flexion-extension gap created through cutting the proximal tibia perpendicularly to its long axis, rather than emulating its natural varus alignment. This can be achieved through the relative thickness of bone removed from the posterior femoral condyles, but care must be taken to establish a rectangular flexion gap; otherwise, knee stability in flexion may be compromised. Any instrumentation for distal femoral preparation that references femoral component rotation on the posterior condyles would, if left unadjusted, place the femur in internal rotation relative to the transepicondylar axis. Posterior condylar referencing therefore requires the surgeon to dial in a degree of external rotation to achieve parallel cuts to the transepicondylar axis (TEA), which has created what is referred to as external femoral rotation. Whiteside and coworkers211 have found the patellar tracking pattern and contact areas to be most normal when the femoral implant is externally rotated by approximately 5 degrees in relation to the PCA.10 External rotation angles beyond 5 degrees, however, appear to have a detrimental effect on the spatial position of the patella in the trochlea.13 Because of the variability in the relationship between the posterior condylar axis (PCA) and TEA, this technique carries certain dangers. Although the main difference between the two axes is 3 degrees of internal rotation, the range is 0 to 10 degrees, with higher values for valgus knees.219 The risk of femoral malrotation is thus higher in the valgus knee, especially if a somewhat hypoplastic posterior lateral femoral condyle has been used as a reference for rotational alignment when making anteroposterior cuts. The situation is usually compounded because the internally rotated femur necessitates subsequent internal rotation of the tibial component to establish rotational tibiofemoral congruency, thus creating excessive external rotation of the tibial tuberosity and patellar maltracking.
Because the TEA represents the functional flexion-extension axis of the knee, it has been established as the ideal reference point for femoral component orientation.24,144,230 Studies have confirmed improved patellar kinematics and a significant reduction of patellofemoral shear forces when the femoral component is placed parallel to the TEA as compared with internal or external rotation.75,205
As an alternative reference to the TEA, the anteroposterior axis, or Whiteside’s line (WL), drawn from the base of the trochlear groove to the center of the intercondylar notch, may be used to establish femoral rotational alignment.12 Current technique encourages clinicians to use TEA and WL to place the femoral component in neutral rotation with respect to those landmarks (Fig. 113-18).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree