Fig. 25.1
Algorithm for surgical treatment of thumb basal joint arthritis
CMC Cartilage Evaluation
Patients with minimal radiographic findings who remain persistently symptomatic despite conservative treatment are candidates for diagnostic arthroscopy [7]. The extent of the cartilage loss is usually worse than the radiograph suggests. Accurate arthritis staging requires arthroscopy [4, 5]. If the cartilage is intact (Badia Stage 1), synovectomy and capsular shrinkage may provide satisfactory results. If the cartilage loss is focal (Badia Stage 2), synovectomy and first metacarpal osteotomy is an option [8, 9]. In the author’s practice, it is uncommon to see patients or operate at Stage 1 or 2 because patients have been treated conservatively elsewhere prior to referral. Patients considering the less invasive procedures described above should be well aware of the potential for progression of the pathology and potential need for arthroplasty in the future. Patients who prefer to minimize the likelihood of additional procedures in the future can be effectively treated with sequential cortisone injections until the arthrosis progresses sufficiently to warrant arthroplasty. While it may be true that intervening at an earlier stage with less aggressive surgical options may provide better ultimate outcome and function, evidence is lacking in the literature.
Many radiographic Eaton Stage 2 [10] cases will be found to have widespread cartilage loss (Badia Stage 3) at the time of arthroscopy. Badia Stage 3 cases are treated with arthroscopic resection arthroplasty as outlined below.
Carpometacarpal Stability
Patients with symptomatic CMC instability are counseled with respect to open and arthroscopic stabilization procedures. Many patients, especially older patients, are primarily concerned with pain relief and are less interested in stabilizing procedures. Clear benefits for this have not been demonstrated in the literature. Patients with CMC instability who desire stabilization are offered arthroscopic ligament stabilization at the time of arthroscopic resection arthroplasty. The procedure is outlined below in section “Surgical Technique CMC Stabilization.”
Scaphotrapeziotrapezoid Cartilage Evaluation
Just as the CMC cartilage loss observed at the time of arthroscopy is usually worse than radiographs suggest, the same is true for cartilage loss involving the STT joint. Diagnostic arthroscopy of the STT joint can be helpful in establishing which radiographic Stage 3 cases are actually arthroscopic Stage 4. (Note: Badia’s classification did not include Stage 4, but it seems a logical addition.) At times it may be difficult to determine the significance of the STT arthrosis. Diagnostic injections are occasionally used to help identify the pain contributions of CMC versus STT when the significance of STT arthrosis is in question. Diagnostic injections are performed by first injecting the CMC with 1 ml of 1 % lidocaine under fluoroscopic control to determine the amount of pain relief and improvement in pinch strength. Ten to 15 min after the CMC injection and after assessment of the amount of pain relief and strength improvement, the STT is then injected under fluoroscopic control. Ten to 15 min later, the amount of pain relief and improvement in pinch and grip strength is again evaluated. Patients who demonstrate substantial benefit from both injections are considered candidates for pantrapezial arthroscopic resection arthroplasty.
Metacarpophalangeal Joint Pathology
Metacarpophalangeal (MP) hyperextension and arthrosis should be addressed prior to surgical treatment of the CMC. Symptomatic, unstable MP joints can be stabilized with MP tenodesis. Fusion should be considered if the MP joint is symptomatic and arthritic. The author has performed many MP tenodesis for MP hyperextension (>30°) over the years. Long-term follow-up has revealed gradual return of the MP hyperextension in a number of cases. Even with return of the hyperextension, however, patients tend to remain very happy with the results provided pain relief is good. It is important to discuss the options concerning the MP joint with the patient. If the MP is unstable but asymptomatic, counsel the patient concerning the possible need for future procedures for the MP joint (if MP pathology is not addressed at the time of the index procedure). If simultaneous MP tenodesis is performed, the disadvantage discussed with the patient includes the risk of loss of correction over time, risk of converting an asymptomatic unstable joint to a symptomatic joint, and increasing the postoperative recovery time.
Surgical Technique: Arthroscopic Resection Arthroplasty of CMC and STT Joint
The procedure can be performed with general or regional anesthesia with or without a tourniquet. When a tourniquet is not used, an anesthetic with epinephrine is infiltrated preoperatively allowing sufficient time for vasoconstriction [11, 12]. The patient is placed on an operating room table with the shoulder abducted and externally rotated. The arm is placed on an arm table with a well-padded nonsterile tourniquet placed on the brachium (if used). The brachium is taped to the arm table. The arm is suspended using 5–10 pounds of finger-trap traction through the thumb (Fig. 25.2). Routine arthroscopy is performed using a 1.9 mm, a 2.3 mm, or a 2.7 mm 30° arthroscope. The smaller scopes are used on the smaller joints and in joints considered potential candidates for joint-sparing procedures such as synovectomy and metacarpal osteotomy. Most resection arthroplasties are performed with a 2.7 mm arthroscope for better field of view.


Fig. 25.2
Operating room setup
Skin incisions are made with a #15 scalpel just through the skin. A blunt hemostat is used to gently dissect through the soft tissue and through the capsule. The radial artery, superficial branches of the radial nerve, and extensor tendons are all at potential risk. These structures are protected through proper technique of blunt dissection. However, even with appropriate technique, they may be injured. These risks should be discussed with the patients preoperatively.
The 1R (volar) and 1U (dorsal) portals are used for CMC arthroscopy. STT arthroscopy is performed using 1R (volar) and 1U (dorsal) portals placed approximately 1 cm proximal to the 1R (volar) and 1U (dorsal) portals as described for CMC arthroplasty. The portals are localized with hypodermic needles with the aid of fluoroscopy (Fig. 25.3). Needles are placed into the joints and confirmed to be parallel on fluoroscopy. These portals lay on either side of the first dorsal compartment. A second dorsal portal is utilized as necessary. The second dorsal portal (dorsal ulnar portal) is placed using inside-out technique by placing a blunt probe through the 1R portal across the CMC or the STT joint and exiting the dorsum of the hand (Fig. 25.4). A cannula is placed retrograde over the probe and inserted into the joint.



Fig. 25.3
Fluoroscopic view of portal placement. Note needles are placed parallel to the CMC and STT joints [Reprinted with permission from Cobb, T, Sterbank, P, Lemke, J. Arthroscopic resection arthroplasty for treatment of combined carpometacarpal and scaphotrapeziotrapezoid (pantrapezial) arthritis. J Hand Surg Am 2011; 36:413-414. With permission from Elsevier]

Fig. 25.4
Inside-out technique for establishing the ulnar dorsal portal for CMC or STT
A full-radius mechanical shaver (typically a 3.5 mm) with suction is used to perform synovectomy and clean the joint of debris for better visualization. Radiofrequency ablation (Serfas 3.5 mm, Stryker, Santa Clara, CA) is used to perform thermal capsulorrhaphy and to perform intra-articular joint denervation. High outflow is utilized to prevent overheating during the use of radiofrequency ablation. A 3.0 or a 4.0 mm barrel bur is used to resect 2–3 mm of bone from the distal aspect of the trapezium and proximal aspect of the first metacarpal. The STT resection arthroplasty is performed by removing 2–3 mm of bone from the distal aspect of the scaphoid and from the proximal aspect of the trapezium and trapezoid (Fig. 25.5). A 4.0 mm barrel bur (Stryker, Santa Clara, CA) is used preferentially in joints large enough to accept the larger size bur.
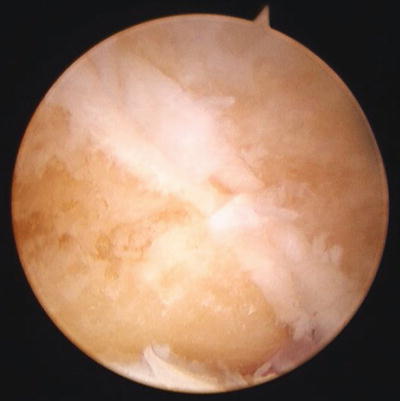
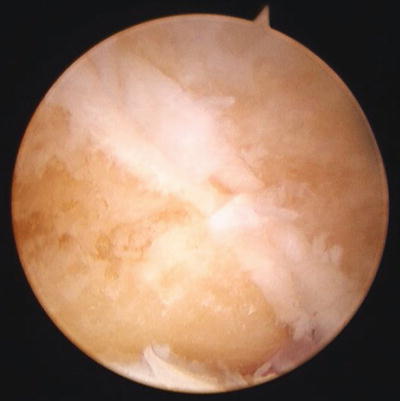
Fig. 25.5
Arthroscopic view of resected STT joint showing resection of proximal surface of the trapezium and trapezoid. The cartilage of the trapezio-trapezoid joint is shown separating the trapezium (left) and the trapezoid (right) [Reprinted with permission from Cobb, T, Sterbank, P, Lemke, J. Arthroscopic resection arthroplasty for treatment of combined carpometacarpal and scaphotrapeziotrapezoid (pantrapezial) arthritis. J Hand Surg Am 2011; 36:413-414. With permission from Elsevier]
The author’s preferred interposition material (when interposition material is used) is the Graftjacket (Wright Medical Technology, Inc., Arlington, TN). This interposition material tends to adhere effectively to the joint and seems to create less inflammatory response than other commercially available products. Early in the author’s series, no graft fixation was utilized. However, a number of grafts were extruded from the joint, requiring removal at a later date. Because of these experiences, the author devised two methods of fixation. The most commonly used fixation involves tying sutures over buttons external to the skin on the volar and dorsal aspects of the joint thereby securing the interposition material within the joint. This is performed by passing absorbable sutures on Keith needles through the volar portal, across the resected joint, and out the dorsum of the hand (Figs. 25.6 and 25.7). The suture is used to pull the interposition material into the resected joint (Fig. 25.8). A second suture is placed on the opposite side of the interposition material before pulling the interposition material through the joint. The interposition material is centered in the joint under arthroscopic visualization. The sutures are then tied over felt and buttons on the volar and dorsal sides of the joint. Since the volar sutures are exiting through the portal, they are passed through the skin adjacent to the portal. This minimizes any potential portal healing issues. The same method of fixation can be utilized for both CMC and STT joints. Alternatively, the interposition material can be secured in the joint using standard arthroscopic knot-tying techniques (Fig. 25.9). This is performed by passing a suture through any stable soft tissue attachment including the capsule or ligament. The interposition material is then pushed into the joint on the suture with a standard knot pusher which is then utilized to tie the sutures arthroscopically. Arthroscopic suture cutters are used to remove the excess suture.






Fig. 25.6
Keith needles are shown passing through cannula in volar portal
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








