Pan Metatarsal Head Resection
Dennis E. Martin
Global forefoot arthroplasty techniques are most commonly associated with rheumatoid arthritis and the profound orthopaedic foot deformities it may produce. However, they can also be effectively applied to a host of other etiologies that can result in complex, multisegmental digital and metatarsal pathology. Examples include psoriatic arthritis, diabetic ulcerations, and Charcot digital neuroarthropathy, as well as traumatic and iatrogenic mishaps. These aggressive forefoot techniques are infrequently demanded and generally not recommended for isolated digital and/or metatarsal anomalies.
Since its original description by Hoffman (1) in 1911, the technical recommendations have remained relatively unchanged. This is quite surprising considering the wide use and popularity of the procedure throughout the last century. Advances in medicine and technology have led to only subtle modifications of Hoffman’s technique. Improvements in metallurgy have afforded increased safety and greater versatility in the use of internal and external fixation devices if required during the surgical correction. This speaks very highly of the effectiveness and dependability of the procedure in treating the variety of etiologies generating a forefoot derangement.
There is still some debate on how to best address the first metatarsophalangeal joint (MTPJ) and its respective metatarsal head. Since Hoffman’s original description through the current era, the debate has involved advocates of straight resection arthroplasty, implant arthroplasty, and MTPJ arthrodesis. In many instances, the presenting pathology dictates the more appropriate technique. Therefore, familiarizing oneself with all three options is important for being able to offer the most comprehensive treatment plan for the variety of scenarios that may present.
Recommendations for the most reliable incision approach are also inconsistent. Plantar transverse curvilinear, dorsal transverse curvilinear, three dorsal longitudinal, and five dorsal longitudinal approaches have all been employed successfully and are supported in the literature (Fig. 63.1). Though this decision often defaults to surgeon preference, the type and extent of the deformities may necessitate one technique over the others. Frequently, combinations of dorsal linear and plantar transverse incisions are required. The plantar transverse method may be used to resect and remove deeply depressed metatarsal heads and/or remove redundant tissue and nodule formation (Fig. 63.2). Digital deformities, when relevant, are addressed through separate dorsal linear entries.
The technique described by Hoffman included resection of all metatarsal heads through a plantar approach combined with manual manipulation and closed reduction of any lesser digital subluxations. He recommended resecting each metatarsal segment to a level that would allow for adequate soft tissue relaxation and complete reduction of any MTPJ contracture. The procedure predictably diminished pain and significantly improved the multitude of structural deformities within the forefoot. However, despite the improved alignment of all MTPJs, active control and functionality of the digits showed little improvement following the aggressive, global resection arthroplasty. In addition, recurrence of deformities was seen in many of these patients over a period of several years.
Over the century, subsequent surgeons have proposed several modifications in an effort to address these complications. Primarily, these efforts focused on improving stability at the first MTPJ and to a lesser degree the interphalangeal joints (IPJs) of the lesser digits. Arthrodesis of the first MTPJ does appear to lend increased structural stability throughout the entire forefoot, resulting in prolonged maintenance of correction and delays in the recurrence of any lesser digital deformities. On the other hand, improvements in restoring an active range of motion and ground purchase to the lesser digits have been minimal in these cases.
Arthrodesis of the proximal interphalangeal joint (PIPJ) of the lesser digits can provide a modest amount of intradigital stability. However, it offers only little resistance to any subluxatory forces developing at the newly created MTPJ. Poor lesser digital ground purchase, along with the eventual, secondary recurrence of deformities, continues to be a disappointing and frustrating consequence regardless of the technical modification.
EVALUATION AND DIAGNOSIS
Generally speaking, the clinical presentation will include a combination of structural and functional pathology involving two or more lesser metatarsal segments with or without great toe deformity. The global malformations occurring in the rheumatoid forefoot have been the most commonly addressed in the literature. These patients typically present with painful, rigid contractures throughout the lesser digits and corresponding MTPJs (Fig. 63.3). The great toe is frequently involved, though not in all cases. In many instances, the disability is enhanced by the formation of large soft tissue nodules underneath one or more of the metatarsal heads. The remainder of the chapter concentrates on this particular patient population. However, the principles and techniques discussed can be used as an accurate guide when assessing and treating the various other etiologies associated with structural and functional derangement of the forefoot.
Though pain at the sites of deformity constitutes one of the primary patient complaints, ulcerations, an unstable gait, and poor-fitting shoe gear are common reasons for presentation. The most important decision the surgeon must make is whether the pathology demands the pan metatarsal head resection technique. It can be technically challenging and postoperatively demanding on the patient, a list of predictable complications is well documented, and the procedures produce permanent, and in most instances irreversible, consequences to the structural
and functional anatomy of the foot. This is a salvage procedure and should be respected as such. Conservative care should be strongly evaluated and exhausted prior to considering surgical intervention. If the MTPJ contractures can be relocated by less extreme techniques or by closed reduction, then global metatarsal head excisions should be avoided.
and functional anatomy of the foot. This is a salvage procedure and should be respected as such. Conservative care should be strongly evaluated and exhausted prior to considering surgical intervention. If the MTPJ contractures can be relocated by less extreme techniques or by closed reduction, then global metatarsal head excisions should be avoided.
The clinical criterion for patient selection is generally agreed upon throughout the literature. A key concept when considering surgical intervention is the nonreducible nature of the contractures. When structural and functional adaptations are severe, the degree of soft tissue relaxation required may only be afforded by resection arthroplasty techniques. Other candidates would include those that have had previous isolated metatarsal head/shaft resection and are now experiencing rigid dislocation symptoms at the adjacent digit (Fig. 63.4). In this instance, any surgical alternative that involved isolated removal of only the involved metatarsal head would be less desirable. Deformities at the remaining untreated digits are predictable and should be anticipated. Severe metatarsal length discrepancies of any origin can be effectively addressed with this technique.
Pathology at the first MTPJ, including hallux abducto valgus, is often coexistent. The degree of deformity and amount of degenerative cartilage loss should guide the surgeon during
procedure selection. The preoperative exam should include evaluation for any additional instability at the metatarsal-cuneiform joint and along the medial arch. Hypermobility at any of these segments makes arthrodesis of the first MTPJ a logical option when no other contraindications exist. When the situation demands it, a Lapidus metatarsal-cuneiform arthrodesis can be considered for pathologic midfoot hypermobility.
procedure selection. The preoperative exam should include evaluation for any additional instability at the metatarsal-cuneiform joint and along the medial arch. Hypermobility at any of these segments makes arthrodesis of the first MTPJ a logical option when no other contraindications exist. When the situation demands it, a Lapidus metatarsal-cuneiform arthrodesis can be considered for pathologic midfoot hypermobility.
A complete examination of the lower extremity vascular, neurologic, and dermatologic systems should be included in the patient workup. Considering the multisystem involvement of diseases like rheumatoid arthritis and diabetes, these patients often present greater perioperative risk. The status of the peripheral vascular system in particular can impact the treatment decision process. The aggressive nature of these techniques demands adequate circulation throughout the entire foot and into the digits. The often slow and prolonged rehabilitation adds the additional risk of venous complications, including thrombosis. When in doubt, preoperative noninvasive vascular studies with digital pressures should be obtained.
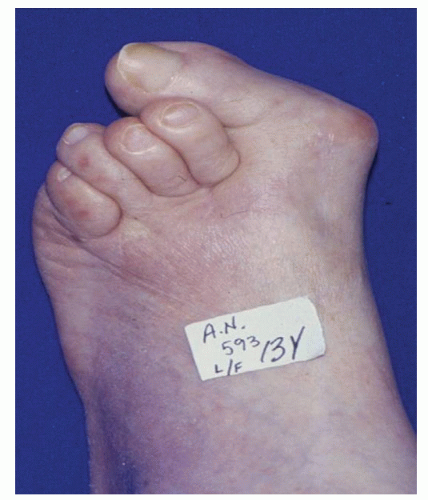 Figure 63.3 This is a severe structural derangement to entire forefoot with hallux valgus deformity.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|







