Abstract
Objective
In this study, we consider two localization techniques used in injections of botulinium toxin in children: electrical stimulation and ultrasound. The hypothesis of this work was that injections performed without stimulation would be less painful.
Patients and methods
Monocentric prospective study, with 107 sessions of lower limb injections. Two groups of children were compared: localization by ultrasound only (60 children), detection by stimulation only or by stimulation combined with ultrasound (47 children). Pain assessment was performed by the child or an accompanying party using the Visual Analog Scale (VAS) and by a health care team using the Face, Legs, Activity, Cry, Consolability (FLACC).
Results
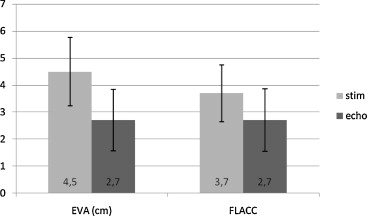
A significant difference between the two groups was found in both self-report and by means of the behavioral observational pain scale. Indeed, VAS average and FLACC average were significantly higher with detection by stimulation than with ultrasound alone: 4.5 cm ± 2.54 versus 2.7 cm ± 2.27; P < 0.001 for VAS scale and 3.7 ± 2.1 versus 2.7 ± 2.3; P < 0.05 for FLACC scale.
Conclusion
When compared to ultrasound detection, localization by electrostimulation appears to increase the overall pain caused during injections of botulinum toxin in children.
Résumé
Introduction
L’objectif de cette étude était d’évaluer la douleur lors des injections de toxine botulique chez l’enfant en fonction de la technique de repérage utilisée. L’hypothèse était qu’en l’absence d’électrostimulation, le geste était moins douloureux.
Patients et méthodes
Étude prospective monocentrique, portant sur 107 séances d’injections des membres inférieurs. Deux groupes de patients ont été comparés : repérage par échographie seule (60 enfants) et repérage par stimulation seule ou stimulation associée à l’échographie (47 enfants). L’évaluation de la douleur a été effectuée avec l’échelle visuelle analogique (EVA) par l’enfant ou son entourage et avec la Face, Legs, Activity, Cry, Consolability (FLACC) par l’équipe soignante.
Résultats
Il existait une différence significative entre les groupes que ce soit pour l’échelle d’auto- ou d’hétéro-évaluation. En effet, l’EVA moyenne et la FLACC moyenne étaient significativement plus élevées dans le groupe électrostimulation que dans le groupe échographie seule : 4,5 cm ± 2,54 versus 2,7 cm ± 2,27 ; p < 0,001 pour l’EVA et 3,7 ± 2,1 versus 2,7 ± 2,3 ; p < 0,05 pour la FLACC.
Conclusion
Le repérage par électrostimulation semble augmenter la douleur globale du geste par rapport à l’utilisation de l’échographie.
1
English version
1.1
Introduction
Botulinum toxin is a treatment of spasticity that has been more and more widely used over the past twenty years. Since 2009 in France, it has become an indicated symptomatic treatment of spasticity of the upper and/or lower limbs in children aged more than 2 years . Scientific proof of its effectiveness in reducing localized spasticity has been provided repeatedly in terms of improved active function of the upper and lower limbs (level of evidence 2) and as a means of attenuating the painful implications of spasticity (level of evidence 2) . As a result, botulinum toxin is now the standard treatment for children with cerebral palsy . Unfortunately, intramuscular injections are at times painful and consequently difficult to carry out in children.
Accurate targeting of a spastic muscle requires localization prior to product injection. Several localization techniques can be applied. More often than not in France, as counseled in official recommendations (Accord Professionnel) , localization is carried out by electrical stimulation , which is nonetheless at once painful and possibly time-consuming . As an alternative, localization by ultrasound has been developing over the last few years. Recent studies have shown its interest as concerns the intramuscular injections performed in treatment of spasticity in children. One of the advantages of localization by ultrasound consists of its rapidity . Moreover, a study by Py et al. shows that in comparison with anatomical localization, ultrasound techniques produces more significant improvement from an analytical as well as a functional standpoint. By the same token, clinical experience has shown that localization by ultrasound appears less painful than localization by electrostimulation. However, scarcely any studies have objectified this clinical fact, and we have found no published work comparing the different localization techniques in terms of the pain they may cause. Our hypothesis is that when electrostimulation is not applied, intramuscular injection is perceived as less painful. The objective of this study has consequently consisted of assessing the levels of pain occasioned by injections of botulinum toxin in children according to the localization technique employed, namely electrostimulation or ultrasound.
1.2
Material and methods
1.2.1
Patients
This is an open monocentric prospective study covering the period from May 2011 to October 2012. The inclusion criteria were: any child less than 18 years of age undergoing a botulinum toxin injection as treatment for spasticity of the lower limbs. The exclusion criteria were: more than 18 years of age, anatomical localization, insufficient data, injection at the level of the upper limbs.
We only included injections carried out on the lower limbs; injections carried out on the upper limbs were excluded so as to obtain localization of targeted muscles presenting as much homogeneity as possible and thereby avoid introducing a bias through which muscle localization would depend on perception of the injection as painful.
For each child treated, an assessment sheet was filled out. The recorded data included: mode of pain assessment (self-evaluation or hetero-evaluation) and demography, as well as the localization technique applied, the type of toxin used, the concentration, the total dose, the number of muscles, the number of injection sites, and the methods of distraction and premedication.
The localization technique was chosen independently of clinical context according to the availability of the ultrasound apparatus on the day of injection.
The ethics committee of the Angers university hospital gave its approval to this observational study.
1.2.2
Course of a session
Local analgesia with EMLA ® cream, a mixture of lidocaine and prilocaine, was systematically applied at the sites of the planned injections, not less than 40 minutes before the latter were carried out. Analgesia by an equimolar mix of oxygen and nitrous oxide was conjointly applied, initially at a rate of 9 L/min, and secondarily at a rate adjusted according to the respiratory volume of the child. The injection was started subsequent to at least 3 minutes of inhalation aimed at achieving optimal sedation.
Antalgic medication by paracetamol at a dose of 15 mg/kg could accompany the above-mentioned analgesia prior to the injection, as could anxiolytic treatment by hydroxyzine at a dose of 0.5 mg/kg or of midazolam at a dose of 0.3 mg/kg. Use of these means of treatment was decided upon according to the age of the child and the degree to which the physician was familiar with him or her. The different medical procedures, methods of distraction and therapeutic drugs were all indicated in the patient’s medical records.
1.2.3
Techniques of injection and localization
Injections were performed by an experienced injector accustomed to applying the two localization techniques. The products used were the botulinum toxin Dysport ® (Ipsen Ltd) or Botox ® (Allergan Inc.). The doses administered were generally 20 units Allergan ® (UA)/kg for Botox ® and 30 units Speywood (US)/kg for Dysport ® .
In ultrasound localization, the apparatus used was the Medical Systems Ultrasound Vivid 7 pro ® . The probe was 9 L. To apply this localization technique, two physicians were needed, one to inject the botulinum toxin and the other to hold the ultrasound probe and guide localization of the targeted muscle. In order to avoid any positioning in a blood vessel, only once the needle had been correctly visualized in the targeted muscle and only after aspiration was the product injected. In localization by electrical stimulation, the electrostimulator was CEFAR Tempo ® , with Ambu ® Neuroline Inoject concentric needle electrodes of which the length and the gauge were adjusted to the muscle and build of the child. The same types of needles were used for botulinum toxin injection, regardless of the localization technique being implemented. When the injecting physicians judged that localization by ultrasound or by electrostimulation alone did not adequately discriminate the targeted muscle, they were allowed to additionally apply the other technique.
1.2.4
Means of pain assessment
Assessment was based on two scales involving self-evaluation or hetero-evaluation: the visual analog scale (VAS) used by the child or the accompanying party and the behavior-based FLACC scale.
1.2.4.1
Assessment by means of the visual analog scale (VAS)
VAS measurement was carried out using a vertical ruler; the child was asked to characterize his pain with phrases ranging from “none at all” to “as bad as possible”. He or she was instructed to set a benchmark (or a finger) at a height corresponding to the pain . On the back of the ruler, ratings were scaled from 0 to 10. Overall assessment of the pain experienced during the session was given by the child just after it ended. The parents were likewise asked to evaluate the pain their child had felt, particularly when, on account of age or communication disorders, it was impossible for the child himself to provide the assessment. When the parents were not present, evaluation was carried out by a third party attending the sessions and familiar with the child. If both the child and another person assessment had been performed, then, we used the VAS scale of the child in our analysis.
1.2.4.2
Assessment by means of the FLACC scale
Pain assessment was also carried out by a medical team using the behavior-based scale known as FLACC (Face, Leg, Activity, Cry, Consolability ). When there were several injections during a session, evaluation pertained to the most painful moment.
1.2.5
Analysis of the data
The variables were expressed in means with standard deviations for the quantitative values and in percentages for the qualitative values. As the distributions of the quantitative variables were not always Gaussian, we also calculated the median, the minimum and maximum values and the confidence interval. The total population was divided into groups according to localization technique:
- •
localization by ultrasound only (echo);
- •
localization by electrostimulation only or conjointly with ultrasound (stim).
The Mann–Whitney and Wilcoxon tests were used to compare distribution of VAS and FLACC variables between the two groups. For comparison of the distribution of covariables (child’s age, number of sites injected, product volume injected, different pre-analgesic techniques), we used the Wilcoxon tests for the quantitative variables and the χ 2 or Fisher’s exact test for the qualitative variables. If the P value was less than 0.05, it was considered as statistically significant. SAS 9.2 for Windows was used for the processing of statistical data.
1.3
Results
1.3.1
Patients
One hundred and fifty-five sessions of intramuscular botulinum toxin injection took place from May 2011 to October 2012. The 40 injection sessions involving the upper limbs were eliminated from consideration, as were 5 sessions with patients more than 18 years of age, 2 in which the data were insufficient, and 1 because localization had been exclusively anatomical. The 107 remaining sessions were analyzed.
Localization by ultrasound only (echo) was carried out in 60 children (56% of the sessions analyzed), and localization by electrostimulation (stim) in 47 (44%). The second group consisted in localized by electrostimulation only in 30 children (28%) and localization by ultrasound associated with electrostimulation in 17 (16%).
Patients’ characteristics are described in Table 1 .
| Echo | Stim | P | |
|---|---|---|---|
| n | 60 | 47 | |
| Age in months: av (SD) | 93.73 (53,77) | 119.23 (63.49) | 0.055 |
| Nb muscles: av (SD) | 5.33 (2.14) | 5.04 (2.18) | |
| Nb sites: av (SD) | 4.98 (2,33) | 5.51 (2.42) | 0.278 |
| Duration in min: av (SD) | 25.65 (6,80) | 27.81 (7.30) | 0.167 |
| Toxin %: Botox | 91.7 | 91.5 | |
| Units: Botox/Dysport | 145/1200 | 139/625 | |
| Volume in mL: av (SD) | 1.84 (1,49) | 1.44 (0,74) | 0.510 |
| Analgesics | |||
| Nitrous oxide | 54 | 44 | 0.728 |
| EMLA | 60 | 47 | 1 |
| Midazolam | 11 | 4 | 0.146 |
Average age of the children was 104.93 months (standard deviation SD: 59.33; median: 100; [27–226]; confidence interval CI: 11.24), that is to say 8.7 years. An average of 5.21 (SD: 2.15; median: 5; [1–10]; CI: 0.41) muscles were injected at 5.21 (SD: 2,38; median: 4; [2–12]; IC: 0.45) sites per session. Average session duration (for n = 47 sessions) was 26 minutes (SD: 7; median: 30; [15–45]; CI: 2). The botulinum toxin Botox ® (Allergan) was most often used (91.6%). Average injected volume (for n = 103) was 1.67 mL (SD: 1.24; median: 1.3; [0.3–7.5]; CI: 0.24). Forty-three percent of the subjects were girls.
The equimolar mix of oxygen and nitrous oxide (Entonox or MEOPA) was used in 92% of the cases and EMLA ® in 100%. Associated oral treatments were less frequent: midazolam in 14% of the cases, hydroxyzine in 4.7% and paracetamol in 3.7%.
The groups in which localization was obtained by either ultrasound or electrostimulation did not significantly differ in terms of age, number of injection sites, average duration of injection, volume injected or pre-analgesic techniques applied. As regards hydroxyzine and paracetamol, frequency of use was too low to carry out statistical analysis.
1.3.2
Pain assessment
1.3.2.1
VAS results
As shown in Fig. 1 , the VAS average for the 105 sessions assessed using the VAS scale was 3.5 cm/10 (SD: 2.5; median: 3; [0–10]; CI: 0.5). The therapeutic threshold of 3 was reached in 56% of the cases (59 sessions). In 15 sessions (14%), the VAS score corresponded to 0 cm (no pain). The VAS average was significantly higher in the electrostimulation group than in the ultrasound group: 4.5 cm ± 2.54 versus 2.7 cm ± 2.27; P < 0.001.
VAS assessment by other persons than the child ( n = 96) resulted in a VAS average of 3.4/10 ([0–9.5]), while VAS assessment by the children themselves ( n = 46) resulted in a VAS average of 3.5/10 ([0–10]).
1.3.2.2
FLACC results
During the sessions, the FLACC average came to 3.1/10 (SD: 2.3; median: 3; [0–9]; CI: 0.4). The therapeutic threshold of 3/10 was reached in 53% of the cases (57 sessions). The average FLACC score was significantly higher in the electrostimulation group than in the ultrasound group: 3.7 ± 2.1 versus 2.7 ± 2.3; P = 0.0012 (< 0.05).
1.4
Discussion
Our findings show that whether pain is measured by self-evaluation or by hetero-evaluation, it is significantly lower when toxin injections are carried out using ultrasound localization. To our knowledge, this is the first study to assess the role of the localization technique chosen with regard to perception of the pain induced by botulinum toxin injections in children.
The “low painfulness” of this technique has already been pointed out by Berweck et al. .
During muscle localization procedures, the pain provoked by electrostimulation is well known and has been observed by all the physicians having applied the technique. However, it was hardly obvious that lessened pain during the localization phase would lead to a significant decrease in perception of pain with regard to the injection taken as a whole. In fact, the overall procedure of intramuscular botulinum toxin injection involves numerous additional algesic elements, such as the puncture, product injection itself, and the anxiety engendered by the hospital environment. In this respect, recent studies by Brochard et al. have shown that the most painful phase was not “localize”, but “injection”. Use of ultrasound has an impact on “localize” alone, not on “injection”. And yet, our study demonstrates that a less painful localization technique, in this case ultrasound, indeed affects the child’s perception of pain with regard to the procedure taken as a whole.
As regards quantitative pain assessment during the sessions organized for our sample, the VAS average came to 3.5/10, while the FLACC average was 3.1/10. These figures correspond to pain of moderate intensity , and they are close to those already reported, particularly by Brochard et al. . In our study, the pain treatment threshold of 3/10 was reached in 56% of the cases evaluated using the VAS and in 53% of the cases evaluated using the FLACC. The study by Brochard et al. reports comparable values with 49% of the cases exceeding the therapeutic threshold on the CHEOPS pain scale. These results show that pain treatment with present-day protocols is still insufficient, and they underline the interest of ongoing attempts to develop a less painful technique.
Whether our assessments are based on the VAS or on the FLACC scale, the relevant results are comparable and confirm the pertinence of the FLACC in external evaluation of induced pain perception. Correlation of the FLACC evaluations and the VAS evaluations produced by parents has already been reported by Voepel-Lewis et al. .
During each session, an average of 5.21 muscles received injections, a figure corresponding to French pediatric experience (the Botuloscope study) , which has shown an average of 4.1 muscles receiving an injection. On the other hand, in our study, the number of injection sites is lower (5.21 sites per session) than in the Botuloscope study, in which an average of 2.1 injections is reported for each muscle, that is to say an extrapolated 8.61 sites per session. At times, ultrasound localization allows for injection of several muscles at a single injection site. For example, the soleus muscle and the underlying gastrocnemius muscle can receive one injection at a single site by inserting a needle more deeply and through visualization of the perimysium separating the two muscles.
Our results do not include comparative evaluation of procedure effectiveness according to the localization technique applied; that was not the objective of our study. Other authors have shown that ultrasound localization can result in greater efficacy using botulinum toxin than that achieved through clinical localization .
Use of ultrasound obviously necessitates an available ultrasound apparatus, which is expensive and requires a sizable investment when centers do not possess the device. In French pediatrics, ultrasound localization is performed only 2% of the time .
The main limit of this study is the lack of randomization, which would have enabled us to distribute the patients between the two groups according to the localization technique applied. In point of fact, a localization technique was chosen by the injecting physician according to the availability of an ultrasound apparatus. Another methodological limit consisted of the impossibility of blinded evaluation. Indeed, our localization technique can hardly be hidden from the patient or the caretaker assessing the pain felt by the child during the procedure. Moreover, our study was not designed to evaluate comparative effectiveness from the standpoint of the efficacy of a procedure according to the localization technique applied. Complementary studies are necessary.
1.5
Conclusion
In our study, localization using electrostimulation intensified the pain provoked by injections of botulinum toxin in our group of children. Ultrasound is an interesting technique that could help to diminish the pain experienced during the localization phase and might lead to decreased perception of pain throughout the session. Complementary studies in adult populations would be useful, and they could help to compare the effectiveness of therapeutic procedures according to the localization technique applied. Were ultrasound apparatuses to become less expensive to acquire, and were more PRM physicians to be trained, use of the technique could grow more widespread.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
La toxine botulique est un traitement de la spasticité qui connaît un essor depuis une vingtaine d’années. En France, depuis 2009, son indication s’est élargie dans le traitement symptomatique de la spasticité des membres supérieurs et/ou inférieurs chez l’enfant de plus de 2 ans . Les preuves scientifiques de son efficacité sur la réduction locale de la spasticité sont maintenant établies avec une amélioration de la fonction active aux membres supérieurs et inférieurs (niveau de preuve 2) et un effet sur la douleur, en atténuant les conséquences douloureuses de la spasticité (niveau de preuve 2) . La toxine botulique est donc devenue le traitement de référence dans la prise en charge de la spasticité des enfants paralysés cérébraux . Malheureusement la réalisation de ces injections intramusculaires est parfois douloureuse rendant ce geste difficile chez les enfants.
Afin de cibler précisément le muscle spastique, un repérage est nécessaire avant l’injection du produit. Il existe plusieurs techniques de repérage à notre disposition. En France, le repérage se fait majoritairement par électrostimulation , comme le conseille les recommandations (Accord professionnel) . Néanmoins, la stimulation électrique est douloureuse et peut demander du temps . Depuis quelques années, le repérage par échographie se développe. Des études récentes montrent son intérêt dans les injections intramusculaires pour le traitement de la spasticité chez les enfants. En effet, cette technique aurait l’avantage d’être rapide . De plus, l’étude de Py et al. montre que ce repérage améliore plus significativement la spasticité tant sur le plan analytique que fonctionnel par rapport à un repérage anatomique. L’expérience clinique montre que le repérage échographique semble moins douloureux que le repérage sous électrostimulation. Cependant, peu ou pas d’étude objective ce fait clinique. Ainsi nous n’avons pas trouvé à ce jour d’étude comparant les différentes techniques de repérage sur le plan de la douleur provoquée. L’hypothèse de ce travail est qu’en l’absence d’électrostimulation, le geste d’injection intramusculaire de toxine est perçu comme moins douloureux. L’objectif de cette étude a donc été d’évaluer la douleur lors des injections de toxine botulique chez l’enfant en fonction des techniques de repérage utilisées à savoir par électrostimulation ou par échographie.
2.2
Patients et méthodes
2.2.1
Patients
Il s’agit d’une étude prospective ouverte monocentrique portant sur la période de mai 2011 à octobre 2012. Les critères d’inclusion étaient : tout enfant de moins de 18 ans bénéficiant d’injection de toxine botulique pour le traitement de la spasticité au niveau des membres inférieurs. Les critères d’exclusion étaient : âge supérieur à 18 ans, technique de repérage par le mode anatomique, données insuffisantes, injection au niveau des membres supérieurs.
Nous avons uniquement inclus les injections effectuées au niveau des membres inférieurs, les injections effectuées au niveau des membres supérieurs ont été exclues afin d’avoir une localisation des muscles cibles des plus homogènes possibles et ainsi de ne pas introduire un biais lié à la localisation du muscle dans la perception douloureuse du geste.
Pour tout enfant traité, une fiche d’évaluation a été remplie. Les données concernant l’évaluation de la douleur (hétéro- et auto-évaluation), la démographie, ainsi que la technique de repérage utilisée, le type de toxine utilisée, la concentration, la dose totale, le nombre de muscles, le nombre de sites d’injection, et les méthodes de distraction et de prémédication y ont été renseignées.
La technique de repérage était choisie indépendamment du contexte clinique en fonction de la disponibilité de l’appareil d’échographie le jour de l’injection.
Le comité d’éthique du CHU d’Angers a donné un avis favorable pour cette étude observationnelle.
2.2.2
Déroulement d’une séance
Une analgésie locale par la crème EMLA ® (mélange de lidocaïne et de prilocaïne) était systématique au niveau des sites d’injection prévus. Elle était effectuée au moins 40 minutes avant les injections. Une analgésie par MEOPA était également associée au débit de 9 L/min initialement puis secondairement adaptée au volume respiratoire de l’enfant. Le geste débutait après au moins 3 minutes d’inhalation permettant une sédation optimale.
Une médication antalgique par paracétamol à la dose de 15 mg/kg pouvait être associée avant le geste. Il pouvait être proposé un traitement anxiolytique par hydroxyzine à la dose de 0,5 mg/kg ou de midazolam à la dose de 0,3 mg/kg. Ces traitements étaient décidés en fonction de l’âge de l’enfant et de la connaissance de l’enfant par le médecin. L’ensemble des actes, méthodes de distraction et thérapeutiques médicamenteuses était noté dans le dossier.
2.2.3
Techniques d’injection et de repérage
Les injections étaient réalisées par un injecteur expérimenté ayant l’habitude des deux techniques de repérage. Les produits utilisés étaient les toxines botuliques Dysport ® (Ipsen Ltd.) ou Botox ® (Allergan Inc.). Les doses étaient généralement de 20 unités Allergan ® (UA)/kg pour Botox ® et 30 unités Speywood (US)/kg pour Dysport ® .
Pour le repérage échographique, l’appareil utilisé était le Medical Systems Ultrasound Vivid 7 pro ® . La sonde était une 9 L. Pour cette technique de repérage, deux médecins étaient nécessaires, l’un injectant la toxine botulinique et le second tenant la sonde échographique afin de guider le repérage du muscle cible. Le produit n’était injecté que lorsque l’aiguille était correctement visualisée dans le muscle cible et après aspiration pour vérifier l’absence de positionnement dans un vaisseau sanguin. Pour les repérages par stimulation électrique, l’électrostimulateur était le CEFAR Tempo ® , avec des électrodes aiguilles concentriques Ambu ® Neuroline Inoject dont la longueur et la gauge étaient adaptées au muscle et à la corpulence de l’enfant. Ces mêmes types d’aiguilles étaient utilisés lors des injections de toxine botulique indépendamment de la technique de repérage. Lorsque le repérage seul par échographie ou par électrostimulation semblait, pour les médecins injecteurs, ne pas discriminer correctement le muscle cible, le médecin pouvait ajouter l’autre technique de repérage.
2.2.4
Moyens d’évaluation de la douleur
L’évaluation s’est basée sur deux échelles permettant une auto- et une hétéro-évaluation : l’échelle visuelle analogique (EVA) évaluée par l’enfant ou l’accompagnant et l’échelle comportementale FLACC.
2.2.4.1
Évaluation par EVA
L’EVA était mesurée au moyen d’une réglette présentée verticalement et on demandait à l’enfant de désigner sa douleur entre « pas mal du tout » et « très très mal ». La consigne est : « place le repère (ou le doigt) aussi haut que ta douleur est grande » . Sur le verso de la réglette, la cotation se fait de 0 à 10. Cette évaluation de la douleur globale de la séance était demandée à l’enfant à la fin de celle-ci. Il était également demandé aux parents d’évaluer la douleur ressentie par leur enfant, notamment lorsque l’évaluation était impossible par l’enfant du fait de son âge ou de ses troubles de la communication. Lorsque les parents n’étaient pas présents, l’évaluation était effectuée par un tiers présent pendant la séance et connaissant l’enfant. Si l’évaluation avait pu être effectuée à la fois par l’enfant et par l’entourage, alors, dans notre analyse, nous n’avons retenu que l’EVA de l’enfant.
2.2.4.2
Évaluation par FLACC
L’évaluation de la douleur a également été effectuée par l’échelle comportementale FLACC (Face, Leg, Activity, Cry, Consolability ). Celle-ci était réalisée par l’équipe médicale. Lorsqu’il y avait eu plusieurs injections lors de la séance, l’évaluation avait été réalisée sur le moment le plus douloureux de la séance.
2.2.5
Analyse des données
Les variables ont été exprimées en moyennes avec écarts-types pour les valeurs quantitatives et en pourcentages pour les valeurs qualitatives. Les distributions des variables quantitatives n’étant pas toujours gaussiennes, nous avons également calculé la médiane, les valeurs minimales et maximales et l’intervalle de confiance. L’ensemble de la population a été séparé en 2 groupes selon la technique de repérage :
- •
repérage par échographie seule (écho) ;
- •
repérage par électrostimulation seule ou associée à l’échographie (stim)
Les tests de Mann–hitney et Wilcoxon ont été utilisés pour la comparaison des distributions des variables EVA et FLACC entre les 2 groupes. Pour la comparaison de la distribution des covariables (l’âge de l’enfant, le nombre de sites injectés, le volume de produit injecté, et les différentes techniques de préanalgésie), nous avons utilisé les tests de Wilcoxon pour les variables quantitatives et le test du χ 2 ou le test de Fisher pour les variables qualitatives. La valeur de p est considérée comme significative si inférieure à 0,05. Le logiciel SAS version 9.2 pour Windows a été utilisé pour le traitement des données statistiques.
2.3
Résultats
2.3.1
Patients
Cent cinquante-cent séances d’injection de toxine botulique intramusculaire ont été réalisées de mai 2011 à octobre 2012. Les 40 séances où les injections avaient été effectuées au niveau des membres supérieurs ont été exclues, 5 séances ont été exclues car concernant des patients âgés de plus de 18 ans, 2 pour données insuffisantes, et 1 car le repérage avait été effectué anatomiquement uniquement. Au total, 107 séances ont été analysées.
Le repérage par échographie seule (écho) a été effectué chez 60 enfants (56 % des séances analysées), le repérage par électrostimulation (stim) chez 47 enfants (44 %). Ce dernier groupe comprend les repérages par électrostimulation seule chez 30 enfants (28 %) et les repérages par échographie associée à l’électrostimulation chez 17 enfants (16 %).
Les différentes caractéristiques des patients sont décrites dans le ( Tableau 1 ).







