before 6 years of age (25, 26). Clinically, the child presents with a painless limp that is caused by both the functional abductor muscle weakness and a relatively minor limb-length inequality in unilateral cases. When the disease is bilateral, the child presents with a waddling gait and increased lumbar lordosis as seen in bilateral developmental hip dislocation (2, 10, 25, 27, 28 and 29). Although pain is seldom reported as a symptom, older children may report a deep ache in the buttock muscles after prolonged exercise.
TABLE 26-1 Classification of Coxa Vara | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
were smaller, the femoral neck was shorter, and the physis was wider on the affected side than on the normal contralateral side. They found that endochondral ossification was altered in the affected hip as well as in the “normal” contralateral side. They also observed that there was a “reduction in the number and caliber of intraosseous arteries supplying the metaphyseal sides of the growth plates in the proximal femur and those supplying the subchondral region and extraosseous medial ascending cervical arteries on the surface of the femoral neck” (34).
possible. Treatment, therefore, is aimed at preventing the secondary deformities of the proximal femur created by the condition’s natural history. Borden et al. (42) identified the main objectives of current treatment approaches: correction of the varus angulation into a more normal physiologic range; changing the loading characteristics seen by the abnormal femoral neck from shear to compression; correction of limb-length inequality; and reestablishment of a proper abductor muscle length-tension relation.
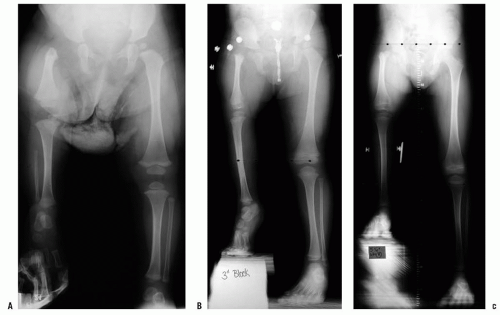
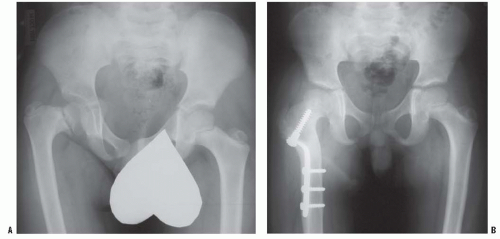
 FIGURE 26-3. The radiographic appearance of acquired coxa vara in an 8-year-old child who had fibrous dysplasia and a shepherd-crook deformity of the proximal femur. |
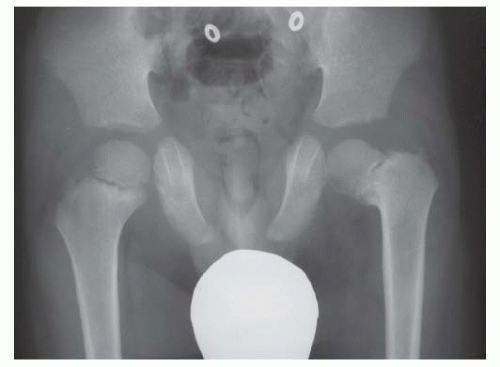 FIGURE 26-4. The radiographic appearance of coxa vara associated with cleidocranial dysostosis in a 4-year-old child. |
osteotomies, which are the treatments of choice (14, 15, 22, 23, 31, 33, 52, 53 and 54). Many intertrochanteric and subtrochanteric osteotomies have been described for correcting coxa vara, thereby indicating that no one method has proved to be totally satisfactory. Langenskiöld valgus-producing osteotomy (12) (Fig. 26-18) and Pauwel Y-shaped osteotomy (23, 55) (Fig. 26-19) are examples of intertrochanteric corrective osteotomies that have produced good results. Pauwel osteotomy is technically demanding and does not allow rotational correction of the upper femur. Borden et al. (42) describe a subtrochanteric valgus-producing osteotomy that has been used successfully in achieving and maintaining the goals of surgical treatment (Fig. 26-20).
TABLE 26-2 Radiographic Features of Developmental Coxa Vara | |||||
|---|---|---|---|---|---|
|
difficult to achieve both satisfactory correction of the varus deformity and relative lateral displacement of the distal fragment. Performing the osteotomy just distal to the lesser trochanter makes it relatively easier to displace the distal fragment laterally. However, the necessary valgus tilting of the proximal fragment may potentiate near abutment of its distal medial edge against the pelvis. When performing a valgus-producing osteotomy, it is often desirable to lateralize the distal fragment. Aligning the shaft of the distal fragment with piriformis fossa of the proximal fragment helps to assure a correct medial/lateral relationship of the two osteotomy fragments. If excessive medialization is noted, either slightly withdrawing the
blade from the proximal fragment or changing to an implant with a longer blade will help to achieve more lateralization. If alternatively relative excessive lateralization of the distal fragment is noted, the blade plate needs to be driven further into the proximal fragment and/or an implant with a shorter blade should be used.
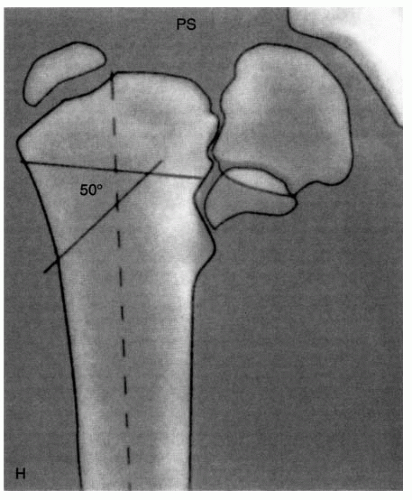
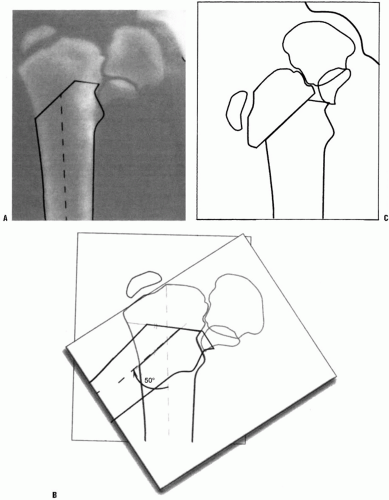
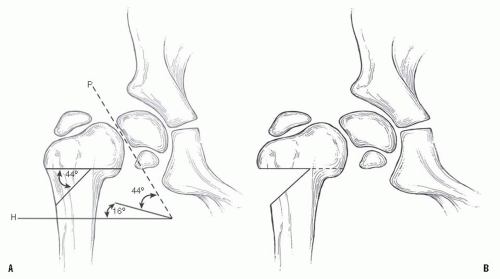
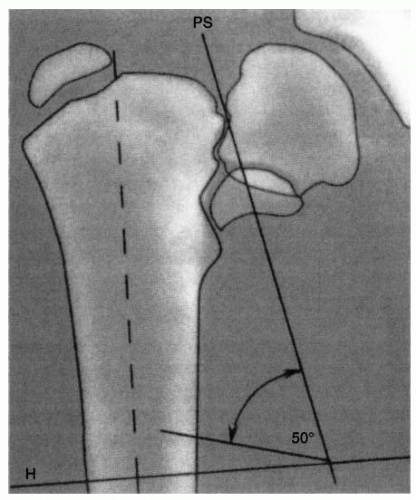 FIGURE 26-9. Valgus Osteotomy for Developmental Coxa Vara. The Pauwels osteotomy (53) is planned to place the physis perpendicular to the direction of the resultant compressive forces (16 degrees off the horizontal), eliminating the shearing forces. In addition, the diaphysis is used to enlarge the proximal end of the femoral neck. The osteotomy does not allow for correction of rotation. The planning of the osteotomy is similar to planning for other osteotomies. A radiograph centered on the femoral head and in the proper degree of rotation is used for the tracing. First, the proximal femur and its axis, the acetabulum, and the physis are outlined on tracing paper. Three lines should be drawn on this outline. First, a horizontal line is drawn several centimeters below the lesser trochanter and perpendicular to the femoral shaft (H). Second, a line is drawn through the physis intersecting H (PS). Third, a line is drawn 16 degrees from the horizontal H line. This will place the physis at 16 degrees, which is perpendicular to the direction of the resultant compressive force. The angle formed by this third line and PS is the size of the wedge to be removed for correction. In this illustration this is 50 degrees. |
 FIGURE 26-14. Amstutz and Wilson (44) discussed the various methods for correction of coxa vara, the difficulty in obtaining and maintaining the desired amount of correction, and the reasons. They thought that in the absence of good fixation in young children, an interlocking osteotomy with a long spike of cortical bone from the distal fragment mortised into a slot in the proximal fragment was best. Some cases required that the spike be placed across the physis and into the femoral head. Mobilization of the fragments was difficult, requiring adductor tenotomy, release of the abductor muscles, and subperiosteal stripping. Occasionally, Kirschner wire fixation was added. All these patients were treated in abduction with a spica cast. |
 FIGURE 26-15. Plykkanen (56) described an osteotomy attributed to Langenskiold. In this procedure, an intertrochanteric osteotomy is performed at the level of the triangular fragment. The distal fragment is abducted so that the lateral shaft of the distal fragment lies adjacent to the cut surface of the proximal fragment. The two fragments may be fixed with cerclage wires, Kirschner wires, or tension band wires. |
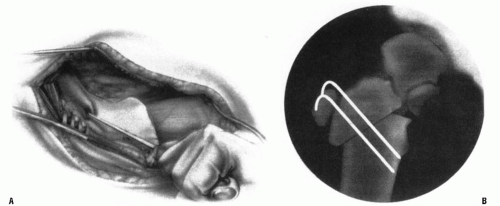
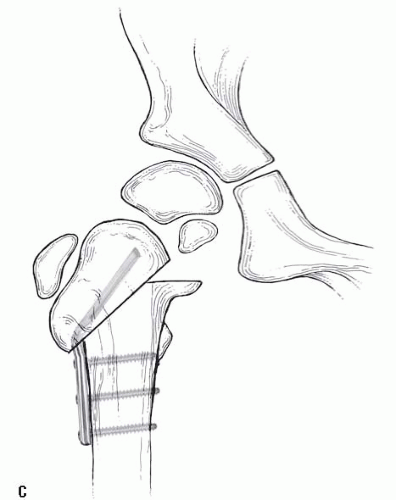
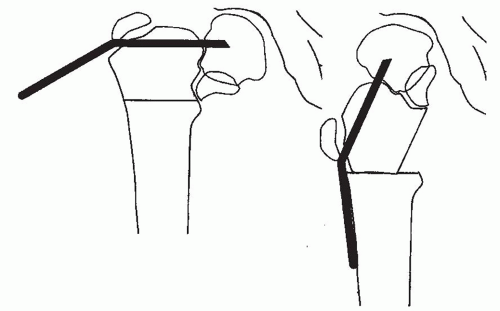 FIGURE 26-16. In the older child, the osteotomy can be accomplished with an angled blade plate as described by Borden et al. (49). For the child, the plate will either have to be custom made or have to be made by bending an available device. This may also be done with some of the newer pediatric screws and plate combinations provided that the plate permits a sufficient amount of valgus. It is often necessary to cross the physis to gain sufficient purchase on the proximal fragment. After the plate is seated, a subtrochanteric osteotomy is performed. With traction and abduction of the leg, the plate is brought into contact with the femoral shaft and secured with a clamp and then with screws. To achieve abduction of the distal fragment, an adductor tenotomy may be necessary (6). To complete the osteotomy without increasing the pressure on the hip joint, it may also be necessary to remove a portion of the distal fragment or a wedge from the lateral aspect of the proximal fragment. |
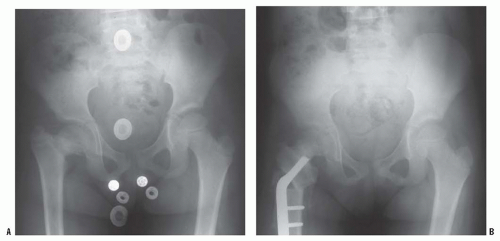
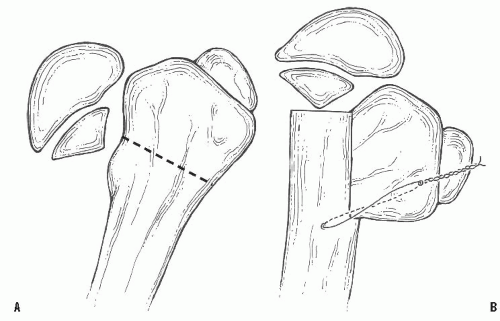 FIGURE 26-18. Langenskiöld intertrochanteric osteotomy. A: Site of osteotomy in proximal femur. B: After osteotomy with fixation in place and resulting coxa valga. |
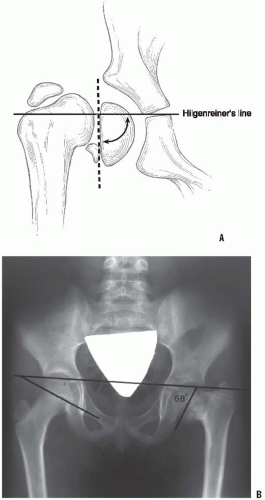
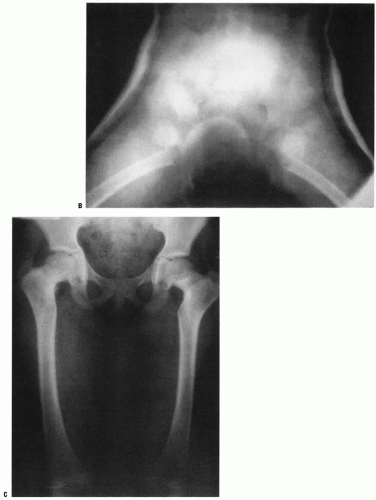
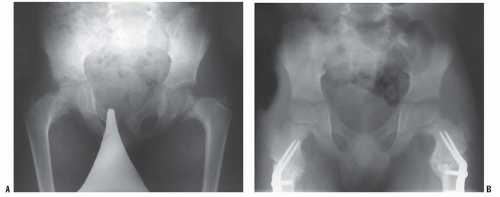
found that if the H-E angle is reduced to <38 degrees, 95% of the patients showed no evidence of recurrence (Fig. 26-22). In contrast, 93% of the osteotomies that retained a physeal angle >40 degrees required revision for recurrent varus deformity.
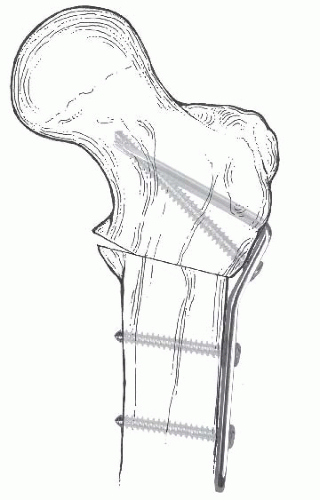 FIGURE 26-21. Internal fixation of valgus osteotomy with the Wagner bifurcated plate. The bifurcated end of the plate is driven into the proximal fragment through its intramedullary surface. |
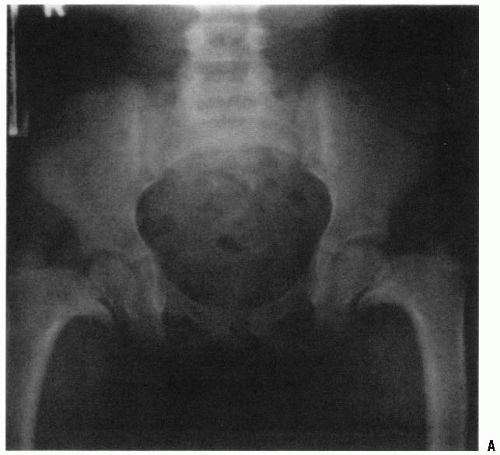
treated with a valgus intertrochanteric osteotomy, especially if it is performed before the child reaches 6 years of age. Carroll et al. (22) reviewed 37 affected hips in 26 children following a valgus osteotomy for congenital or acquired coxa vara. They reported a 50% recurrence rate that was unrelated to age at the time of surgery, the type of internal fixation, or the etiology. Of the children in whom the H-E angle was corrected to <38 degrees, 95% had no recurrence of the deformity. If the femoral osteotomy is performed before 10 years of age, 83% of the patients will have excellent acetabular development (Fig. 26-24).
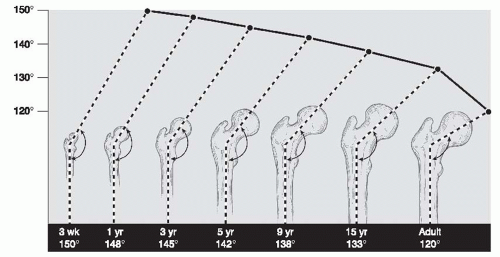
out any other possible cause for this condition (Table 26-1). Once diagnosed, the child should be followed up every 4 to 6 months with anteroposterior radiographs of the pelvis. Surgical intervention is recommended for hips with an H-E angle of 60 degrees or greater, a progressive decrease in the femoral neck-shaft angle of 90 to 100 degrees or less, or in patients with developmental coxa vara who develop a symptomatic limp or Trendelenburg gait. The authors prefer an intertrochanteric valgus-producing, and, as appropriate, rotational osteotomy of the proximal femur. The preferred fixation device is an adolescent size blade plate (130-degree angle). For larger adolescent patients, the adult size 130-degree blade plate is used. For small and/or young patients, the modified Wagner plate (Fig. 26-23) and supplemented spica cast is preferred. An adductor tenotomy is performed if contracture of the adductor muscles limits passive hip motion. If an adductor tenotomy is performed in conjunction with the valgus osteotomy, an abducting wedge-shaped foam pillow is utilized for comfort for the first 3 to 4 weeks postoperatively. Following a valgus-producing osteotomy, bone overgrowth of the fixation device is likely. The authors recommend surgically removing the implant 1 to 2 years following healing of the osteotomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree