In North America, a screening examination either in a school or at a routine primary care visit often leads to referral to a specialist. Many of these patients, therefore, have no symptoms
and are completely unaware of their potential spinal deformity. Evaluating a patient with scoliosis requires the physician to assess the patient for all conditions (
Table 17-1) that are associated with scoliosis. While most adolescents presenting with scoliosis will be diagnosed as idiopathic, a careful history and physical examination are required in order to be certain no other causes exist that may affect their management.
Physical Examination.
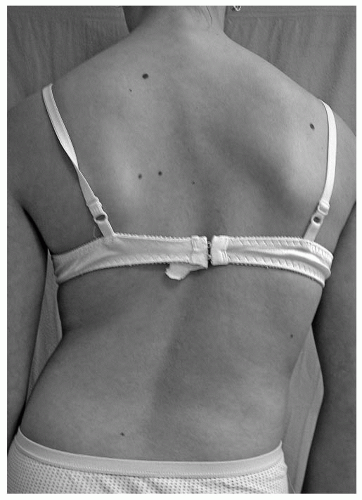
Physical examination of a patient with scoliosis includes evaluation of trunk shape, trunk balance, the neurologic system, limb length, skin markings, and skeletal abnormalities. Assessment of pubertal development includes assessment of the stages of breast development and the presence of axillary/pubic hair (Tanner stages). This can be done discreetly without fully undressing the patient. Girls can be asked to wear a two-piece swimsuit for the physical examination (the instruction regarding this can be given at the time of fixing the appointment). This reduces the patient’s anxiety and apprehension, yet allows assessment of breast and overall development.
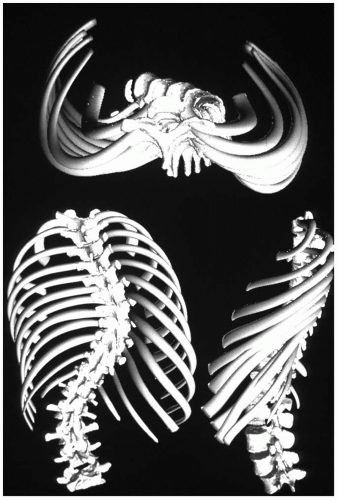
With the patient standing, the back and the trunk are inspected for asymmetry of shoulder height, scapular position, and shape of the waist viewed from both front and rear. Potential pelvic tilt (an indicator of limb-length difference) is determined by palpating the iliac crests and the posterior inferior iliac spines bilaterally in the standing patient with both hips and knees fully extended. Lateral translation of the head can be measured in centimeters of deviation from the gluteal cleft by dropping a plumb line from C7. Deviation of the chest cage (trunk shift) should also be assessed because patients can have full head compensation (return of the head and neck back to midline) yet have marked lateralization of the trunk (
Fig. 17-7).
Forward Bend Test.
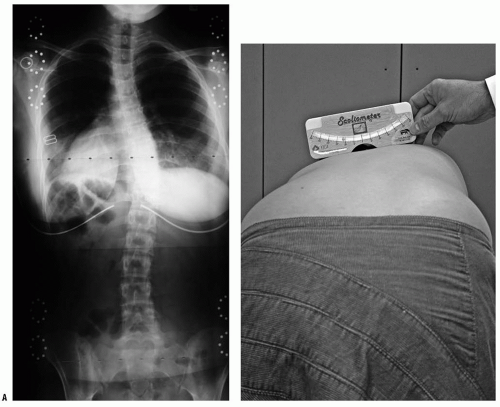
The forward bend test, first described by Adams in Britain (
109), has the patient bend forward at the waist with the knees straight and the palms together. This examination should be performed from behind (to assess lumbar and midthoracic rotation) and from the front (to assess upper thoracic rotation), as well as from the side (to assess kyphosis). Any asymmetry of the upper thoracic, midthoracic, thoracolumbar, and lumbar regions should be quantitated with a scoliometer (
110) [to determine the angle of trunk rotation (ATR)] or by measuring the height of the prominence in centimeters (
Fig. 17-8). This prominence reflects the rotational deformity of the spine associated with scoliosis (
111,
112). Although there is not always an exact correlation, in general an ATR of 5 to 7 degrees is associated with a radiographic Cobb angle measurement of 15 to 20 degrees. [This is only an approximate guideline-occasionally patients may have little trunk rotation and yet have significant radiographic scoliosis, and
vice versa (
113).]
An inability to bend directly forward at the waist or a decreased range during forward/side bending may be caused by pain, lumbar muscle spasm, and/or hamstring tightness; any of these should suggest underlying pathology. These findings plus abnormalities in straight-leg-raise testing suggest irritation of the lumbar roots caused by spondylolysis, disc herniation, infection, neoplasm, or other factors.
Neurologic Examination.
The neurologic examination should evaluate balance, motor strength in the major muscle groups of all four extremities, and sensation. Watching the patient’s gait, toe-and-heel walk, tandem walk, deep squat, and single-leg hop allows rapid assessment of balance and motor strength. The presence of a cavus deformity of the feet, especially if it is unilateral, suggests an abnormality of the neurologic system/spinal cord. Testing for reflexes should include deep tendon reflexes of the upper and lower extremities as well as the Babinksi test for long tract signs. Abdominal reflexes are obtained by lightly stroking the abdominal wall with a blunt instrument (end of reflex hammer) adjacent to the umbilicus with the patient supine and relaxed. The expected brisk and symmetrical unilateral contraction of the abdominal musculature pulling the umbilicus toward the side being stroked indicates normalcy. When the reflex is persistently abnormal (reflex absent on one side and present on the other), intraspinal disorders, particularly syringomyelia, should be considered. The lower cranial nerves and the upper extremity examination should not be ignored because cervical-level pathology (particularly syringomyelia) presents here (
81,
114).
Further Assessment, Limb Length.
Additional components of a comprehensive scoliosis examination include inspection of the skin (both on the back and elsewhere) for
cutaneous evidence of an associated disease. Café-au-lait spots and/or axillary freckles suggest possible neurofibromatosis, whereas dimpling or a hairy patch in the lumbosacral area may suggest an underlying spinal dysraphism. Excessive laxity of skin or joints may be related to a connective tissue disorder such as Marfan syndrome or Ehlers-Danlos syndrome.
Limb length should also be measured in the supine position if pelvic tilt is noted during the standing examination. A spinal curvature that results from a limb-length difference is usually compensatory and serves to rebalance the trunk over the pelvis. A short right leg results in a compensatory right lumbar curve. There is no rotational deformity of the spine with these curves, and in the lumbar region the prominence noted on the forward bend test is on the concave side of the curve (the long leg makes the iliac crest and the lumbar spine more prominent on that side). This is the opposite of what is seen in true lumbar scoliosis, where the rotational prominence noted on the bending test is found on the side of the curve convexity. The presence of the bending test rotational prominence on the “wrong” side in a lumbar curve is almost always diagnostic of spinal asymmetry caused by limb-length discrepancy rather than true scoliosis. The prominence disappears if the pelvis is leveled with an appropriately sized block underneath the short leg.
Radiographic Assessment.
The ideal screening radiographs for scoliosis are upright (standing) posteroanterior (PA) and lateral projections of the entire spine exposed on a single cassette. The radiograph must be taken with the patient standing because diagnostic and treatment standards developed over
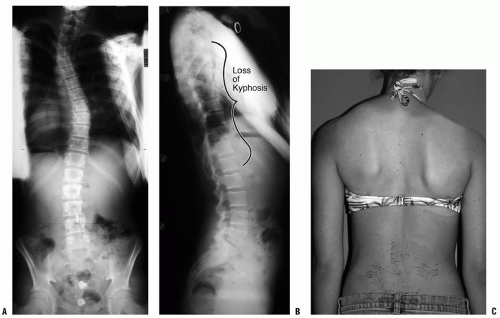
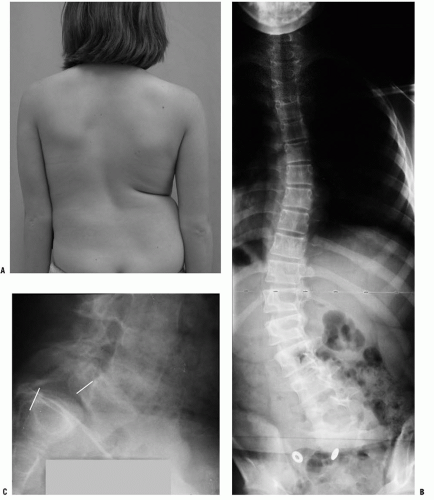
the years are based on films in the upright posture. In very young patients, or in those with severe neuromuscular involvement, radiographs taken in the sitting or even supine position may be the only ones possible. The magnitude of the curve is greater when the patient is upright (compared to supine), and this is of particular importance in infantile and congenital curves when radiographs are taken before and after walking age. “Curve progression” may mistakenly be noted with the first upright-position radiograph as compared to prior supine views, when in fact one has simply documented that gravity causes a curve to be more severe. The sagittal balance varies with the method of arm positioning (the arms must be flexed for the spine to be clearly visualized). With the arms held straight forward, the trunk shifts posteriorly, and therefore the best position for viewing relaxed standing is with the arms flexed as little as possible to clear the spine (
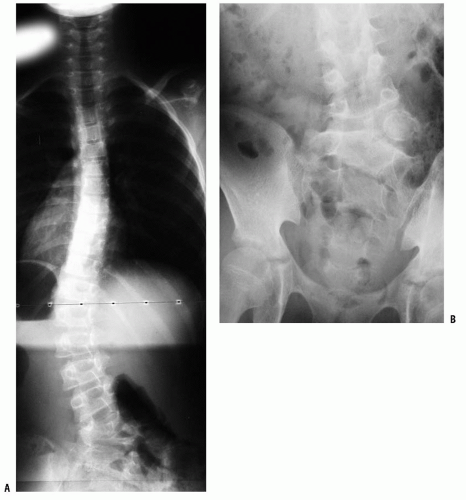
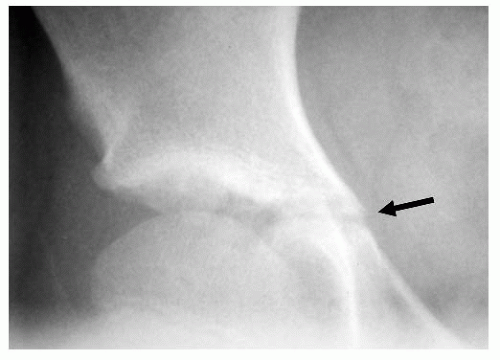
115). A lateral view of the lumbosacral junction is often performed in lumbar scoliosis to assess for spondylolysis/spondylolisthesis as a possible cause (
Fig. 17-9).
Radiographic techniques that are used for minimizing radiation exposure of sensitive tissue (e.g., breast, thyroid, ovaries, and bone marrow) include taking only the required number of x-rays, utilizing rare earth radiographic enhancing screens with fast film, and a posterior-to-anterior exposure (
116,
117 and
118). The lifetime risk for developing breast or thyroid cancer has been suggested to increase by 1% to 2% in patients who are exposed to multiple x-rays during the course of treatment of scoliosis; however, these data relate to the 1960s and 1970s, before new radiation-reducing techniques became available. The greatest reduction in breast and thyroid exposure is associated with the PA exposure [compared to the anteroposterior (AP)]; this reduces breast/thyroid exposure three- to sevenfold (
118). AP projection can shield the breasts; this is, however, not recommended because this projection increases thyroid exposure (shielding the thyroid obstructs the view of the upper spine). A new x-ray detection system that requires roughly one-eighth the radiation has been developed by Charpak, which has the potential to substantially reduce radiation for this population (
116,
117). Doctors counsel their patients by assuring them that during the radiographic procedure, the exposure to the x-rays required to treat the disorder correctly will be minimal and that the benefit of undergoing the procedure outweighs the risk of not knowing the type and severity of the scoliosis.
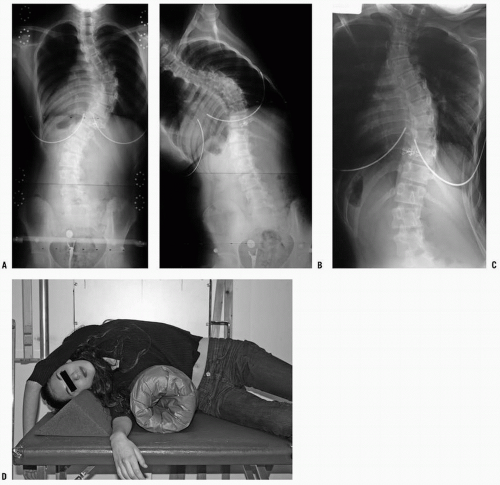
When surgical treatment is being considered, lateralbend radiographs (to assess curve flexibility) are required. Radiographs of side bending allow one to determine the degree of curve flexibility, and to decide what levels to include in the instrumented and fused segments. Controversy remains regarding the best method of obtaining AP films of side bending. Supine-position side-bending views (patient maximally bent to the right and left) are standard at many institutions, whereas others believe that a standing-position bend film is a better indicator, particularly in the lumbar spine. Lateral bending over a bolster provides somewhat greater correction and has been proposed as a more accurate predictor of the correction obtainable with the more powerful modern surgical instrumentation methods (
87,
119) (
Fig. 17-10). In curves >60 to 70 degrees, longitudinal traction films may also be helpful in evaluating curve flexibility (
120,
121). There is no universal standard for how to obtain radiographs of bending. Additionally, there is little agreement on how to make use of the information gained. Flexible minor curves may be spared arthrodesis in many cases, and this flexibility information has been utilized (yet not necessarily standardized) in surgical decision making. More severe cases of scoliosis, that is, curves that do not straighten to <50 to 60 degrees, have been suggested as benefiting from an anterior release procedure prior to posterior instrumentation.
The Stagnara oblique view, taken perpendicular to the rib prominence rather than in the PA direction, provides a more accurate picture of large curves that have a large rotational component. From this angle, the true magnitude of the scoliosis can be measured more accurately (
14,
122). Similarly, an oblique lateral may show the true sagittal alignment at the apex.
Reading Scoliosis Films.
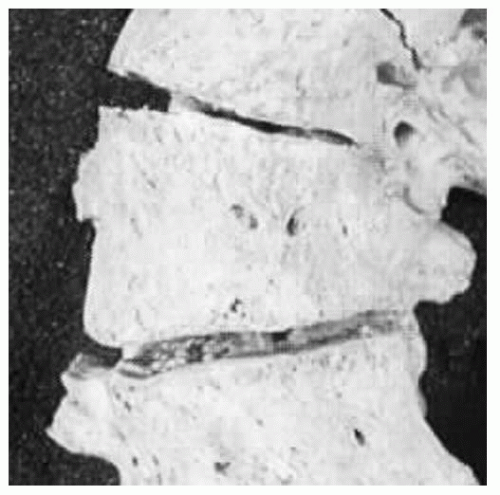
Assessment of the standing PA film begins by looking for soft-tissue abnormalities, congenital bony abnormalities (wedge vertebrae, etc.), and then by assessing curvature (coronal plane deviation). Bone assessment includes looking for wedged or hemivertebrae (
Fig. 17-11) and bar formation bridging a disc space as well as midline irregularities such as spina bifida or a bony spike suggesting diastematomyelia. The pedicles should be inspected in order to verify that they are present bilaterally and that the interpedicular distance is not abnormally increased, which would suggest an intraspinal mass (
123,
124). Absent pedicles or vertebral body lucency are associated with lytic processes, such as tumor or infection. If a curve is noted, the symmetry and the levelness of the pelvis are analyzed. A limb-length discrepancy can be estimated by determining height differences between iliac wing and hip joint, assuming the patient had hips and knees fully extended when the film was exposed.
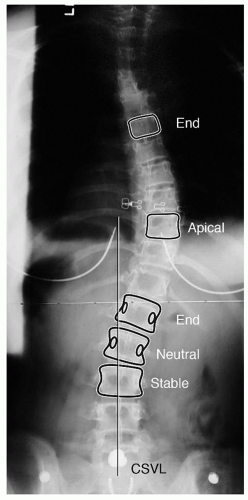
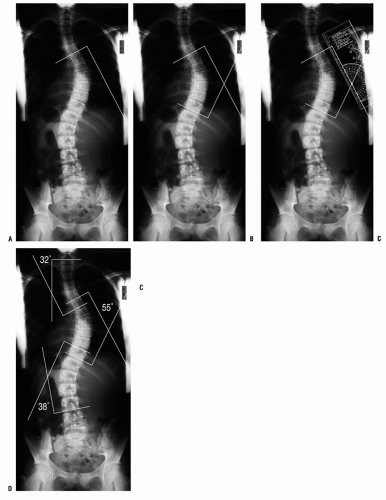
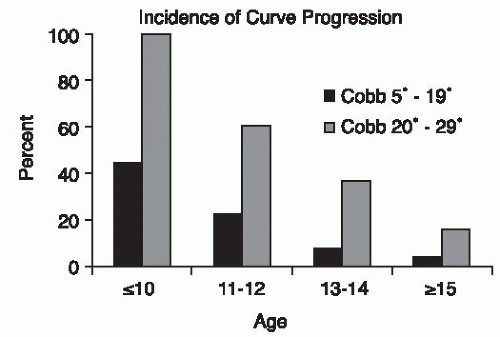
Curve measurement using the Cobb method (
125) allows quantification of the curve. A protractor or digital software tool allows for accurate measurements. The caudal and cranial end vertebrae to be measured are the vertebrae that are the most tilted, with the degree of tilt between these two vertebrae defining the Cobb angle (in a normal spine this angle is 0 degrees). One should outline the superior end plate of the cranial end vertebra and the inferior end plate of the caudal end vertebra. If measuring by hand, construct a perpendicular to each of these lines and then measure the angle at which the lines cross. When more than one curve exists, a Cobb angle measurement should be made for each curve (
Fig. 17-12). The wide variation of inter- and intraobserver error (approximately 5 degrees for any curve measurement) should be understood by the surgeon and the anxious parents (and patient) (
126). Therefore, a 6-degree difference is accepted by most surgeons as the criterion for determining curve progression in idiopathic scoliosis.
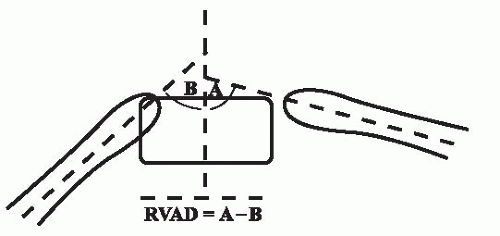
Vertebral rotation, maximal at the apex of a curve, is demonstrated on radiographic film by asymmetry of the pedicles and a shift of the spinous processes toward the concavity. Two methods are available for quantifying this rotation, one suggested by Nash and Moe (
127) and the other by Perdriolle (
128). Vertebral rotation is not routinely measured clinically, however, and both methods have substantial inaccuracies, which limit their usefulness (
129).
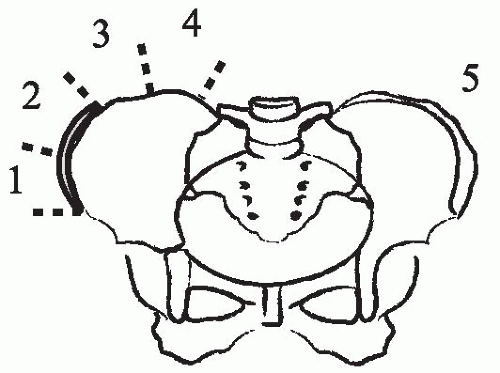
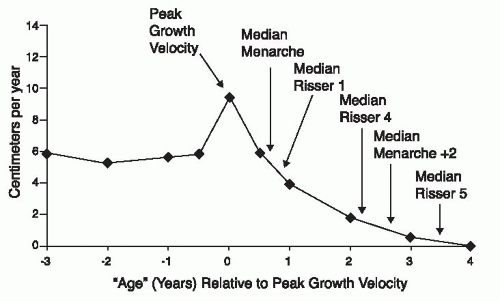
Skeletal maturity should be assessed radiographically in order to estimate remaining spinal growth, an important predictor of risk for curve progression. The most widely used method in patients with scoliosis, although probably the least reliable, is that of Risser (
130), who noted that the iliac crest apophysis ossifies in a predictable fashion from lateral to medial, and that its fusion to the body of the ilium mirrors the fusion of the vertebral ring apophysis, signifying completion of spinal growth. The lateral-to-medial ossification of the iliac crest apophysis occurs over a period of 18 to 24 months, finally capping the entire iliac wing. Risser classified the extent of apophyseal ossification in stages, ranging from Risser 0, indicating absence of ossification in the apophysis, to Risser V, indicating fusion of the fully ossified apophysis to the ilium (spinal growth complete) (
131). Risser I through IV are assigned to the intermediate levels of maturity as seen in
Figure 17-13.
Risser originally described this finding on AP radiographs, which place the iliac apophysis close on the x-ray film. This is in contrast to the common current practice of PA projections and may explain some of the difficulties in reading this sign
(
132). Despite the common reporting of the Risser sign as a measure of maturity, the appearance of the iliac apophysis generally occurs after the most important period of rapid growth (
97,
99). Little and Sussman (
133) have suggested that the Risser sign is no more accurate at predicting scoliosis progression than chronologic age.
The status of the triradiate cartilage of the acetabulum also provides a landmark for assessing growth potential. The triradiate growth cartilage usually closes before the iliac apophysis appears (Risser 0), at about the time of maximal spinal growth (
134,
135) (
Fig. 17-14). Skeletal age can also be measured using the Greulich and Pyle atlas (
136) to compare hand radiographs against illustrated standards, although these readings become less accurate (large standard deviations) in the juvenile age group. Some authors have recommended using the maturation of the olecranon to determine skeletal age (
137). Sanders has recently reported on the “digital skeletal age,” which provides information about growth potential particularly useful during the Risser 0 phase (
138). This system uses the progressive development of the epiphysis of the metacarpal and phalanges to determine skeletal age.
Specialized Imaging Studies.
Most idiopathic scoliosis cases do not require imaging beyond plain radiography. Specialized imaging methods that can be used to evaluate cases with unusual features include MRI, CT, and bone scintigraphy, each with specific indications and advantages.
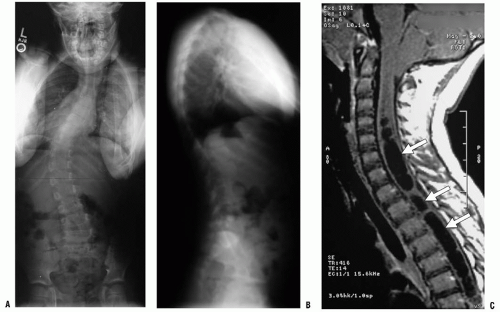
MRI has almost completely replaced myelography in the study of the neural elements in spine disorders. An exception is the patient who has had prior placement of stainless steel implants (making MRI visualization nearly impossible) and who continues to have symptoms or develops new ones that have to be studied.
MRI study of the spine is indicated for all patients with idiopathic scoliosis in the infant and juvenile age groups (
92,
93,
139,
140) and also for those with congenital bony anomalies if surgical correction is planned (
141,
142). Left thoracic curves have been shown to have an increased association with spinal cord anomalies and may be an indication for MRI study (
140,
143). It has also been suggested that all male patients should have a screening MRI, although no studies exist to substantiate this. Indications are not clear for routine MRI prior to corrective surgery in patients with typical idiopathic scoliosis (for whom clinical neurologic examination has shown normal results) (
144). Several prospective studies have been completed (
145,
146 and
147) of routine MRI screening for preoperative assessment (spine and brain) of all patients with idiopathic scoliosis. There is no evidence that an MRI is helpful in an otherwise normal adolescent with scoliosis. Clearly, however, patients with an abnormality in the neurologic examination (
140) or with cutaneous findings (suggestive of dysraphism or neurofibromatosis) should have an MRI study of the spine and/or brain. Additionally, Ouellet et al. (
148) have suggested that a hyperkyphotic sagittal alignment of the thoracic spine should raise suspicion of a syringomyelia and trigger an MRI study. Severe angular and rotational deformities may be difficult to analyze with an MRI because the spinal canal deviates into and out of the planar cuts of the sagittal and coronal images. CT myelography that produces a dye column may be better for revealing stenosis or an intraspinal filling defect in extremely severe cases of scoliosis.
The workup of patients with substantial back pain with no obvious cause may require a bone scan and/or MRI to evaluate for possible tumor, infection, or spondylolysis. The bone scan is an excellent screening test for studying the patient with scoliosis who is experiencing pain. The test allows one to screen for conditions ranging from osteoid osteoma to hydronephrosis. A single-photon emission computed tomography type of bone scan (computerized tomographic enhancement) is very useful in identifying spondylolysis and its varying presentations (unilateral, bilateral, cold scan, hot scan, etc.). If an area of increased activity is noted on the bone scan, additional imaging (either MR or CT) may be required. An MRI may also be used as a screening tool for patients who are in pain, although cortical lesions (spondylolysis) may be harder to identify, and benign osteoid osteomas have been overinterpreted as malignancies. A screening MRI should include the entire length from the brain stem/posterior fossa to the sacrum. Individual MRI sequences for the brain, cervical, thoracic, and lumbar regions are not required. A limited number of images, primarily in the sagittal and coronal planes, are sufficient to identify a tumor, Chiari malformation, syringomyelia, or tethered cord. All aspects of the evaluation of a patient with scoliosis (history, physical examination, imaging studies) should be focused first on identifying possible nonidiopathic causes of the deformity, and only secondarily on characterizing the specific features of the curve. If one assumes an idiopathic etiology, an underlying spinal cord abnormality or associated syndrome will be very difficult to identify. One cannot recognize what one does not look for.