Fig. 57.1
Indication for tibial tubercle osteotomy for patellofemoral correction or to achieve sufficient access to the anterolateral aspect of the knee
Especially in revision surgery, when the patellar mobility is limited due to scarring and a patella baja situation is often found, it may be difficult to obtain sufficient exposure and access to the anterolateral compartment of the knee.
Normally, the Insall-Salvati index given by the length of the patella and the patellar tendon is about one [7]. A patellofemoral index of less than 0.8 means a low position of the patella (patella baja or infera) and above 1.2 high position (patella alta). The Caton-Deschamps index is another well-established index and gives the quotient between the size of the cartilage surface of the patella and the distance between the inferior pole of the articular surface of the patella and the tibial articular surface [3]. Biomechanical studies have shown that lowering the patella, which is frequently the case in open wedge high tibial osteotomy, leads to an increase of loading of about 300 % at 30°, 60° and 90° of knee flexion. Highest loading is seen at 60° of flexion [12].
The incidence of a patella baja after primary TKR is about 10 % [9]. In contrast to a true patella baja, a pseudo-patella baja can be created during surgery. A real patella baja may occur due to shortening of the patellar tendon after primary TKR (Fig. 57.2). A pseudo-patella baja is created due to joint line elevation during surgery. It may occur during both primary and revision TKR caused by increased distal femoral bone loss and inadequate reconstruction with spacer or due to extended soft tissue release while balancing the knee. A thicker polyethylene liner is required to gain stability in these cases (Fig. 57.3a, b).



Fig. 57.2
Patella baja seems to be a major problem in revision total knee replacement due to contraction of the extensor mechanism. The short patellar tendon does not allow sufficient access, and tibial tubercle osteotomy might be indicated for temporary better exposure to the knee or to avoid patellar tendon avulsion

Fig. 57.3
A pseudo-patella baja is shown caused by the high polyethylene liner
The risk of having a patella baja is much higher in revision TKR than in primary TKR. It has been shown that a better clinical outcome can be achieved when the joint line is preserved within 4–5 mm of the healthy knee [6].
A patella baja clearly leads to increased loading and pressure within the patellofemoral joint, which was recently shown by increased bone tracer uptake in single photon emission computerised tomography/computerised tomography (SPECT/CT) [11]. In these cases with clearly increased loading, a proximalisation of the tibial tubercle might be beneficial. This needs to be confirmed in clinical studies.
Furthermore, in some revision cases, in particular with long tibial stems, it may be impossible to remove the previous implant without tibial tubercle osteotomy.
57.2 How to Perform a Tibial Tubercle Osteotomy
Different techniques have been described for tibial tubercle osteotomy. Some authors recommend a step cut osteotomy while others are more in favour of a bevel cut osteotomy (Fig. 57.4).
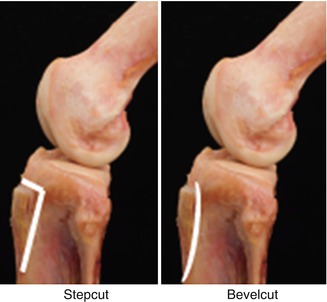
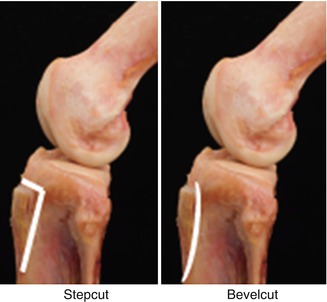
Fig. 57.4
Lateral view of the knee showing the bevel cut and step cut tibial tubercle osteotomy
Stability of different fixation techniques has been studied. Davis et al. biomechanically investigated the fixation stability of common techniques for tibial tubercle osteotomy and their fixation [4].
The following groups were analysed:
1.
Bevel cut osteotomy and fixation using two 4.5 mm cortical screws
2.
Bevel cut osteotomy and fixation using three 18 gauge steel cerclage wires
3.
Step cut osteotomy and fixation using three 28 gauge steel cerclage wires
4.
Step cut osteotomy and fixation using four 18 gauge steel cerclage wires
This study showed that two bicortical screws (1634 ± 359 N) provide the greatest static fixation strength for repairing tibial tubercle osteotomies. However, in this study, the size of the tibial tubercle osteotomy was larger (12 cm in total length, 8 cm in length inferior to the tibial tubercle) in length than normally recommended. Furthermore, the step cut osteotomy provided greater stability than the bevel cut osteotomy. Other studies also reported higher rates of tibial tubercle displacement when cerclage wires were used in comparison to screws [2]. The use of no. 5 Ethibond suture for repair has also been described [5]. In conclusion, 3.5 mm bicortical screws are recommended for tibial tubercle refixation after osteotomy. There is an open discussion whether the osteotomy should be performed from medially or laterally. Vascular supply to the tibial tubercle seems to come from both sides. Technically it is easier to perform it from the lateral side. In our experience, osteotomes and not the saw should be used for tibial tubercle osteotomy; however, there is only sparse evidence.
When performing an osteotomy, sufficient bone should be taken from the tibial tubercle to allow secure refixation of the tibial tubercle. A very small osteotomised tibial tubercle may fail after refixation, but a very large one may weaken the proximal tibia. Arnold et al. recommended an osteomised tibial tubercle of more than 5 cm [1]. In a recent study investigating 422 patients after TKR, which was implanted using the anterolateral approach including step cut tibial tubercle osteotomy, Wishart et al. analysed the tibial tubercle osteotomy performed on radiographs and correlated these findings with complications related to the tibial tubercle osteotomy. They found that the length of the tibial tubercle osteotomy and the proximal barrier of the step cut were significantly correlated. It was recommended to have a length between 5 and 5.5 cm and a proximal barrier of at least 15 mm [13]. The complication rate in this study was 3 %. The most important complications were displacement or fracture of the tibial tubercle, skin necrosis, screw displacements and hematomas (Fig. 57.5).










