and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
Bone cuts and soft-tissue releases are the principal steps in TKA. However, some knees undergoing TKA may require an additional procedure in the form of an osteotomy. An osteotomy in primary TKA is usually indicated in rigid or severe deformities to facilitate soft-tissue balance and deformity correction, to concomitantly correct an extra-articular deformity or rarely to facilitate exposure of the joint. Frequently, in varus arthritic knees undergoing TKA, the medial and posteromedial side of the tibial plateau shows adaptive changes resulting in the formation of a prominent bony flare in this area. This causes local tenting of the medial soft-tissue structures and contributes to knee deformity and medio-lateral soft-tissue imbalance. A reduction osteotomy involves excision of this medial bony flare to decompress the medial soft-tissue structures. Rarely, despite extensive soft-tissue release and a reduction osteotomy, a knee deformity may be too rigid and/or the medio-lateral soft-tissue imbalance too severe to correct. In such cases a sliding medial condylar osteotomy (SMCO) in a varus knee or a lateral epicondylar osteotomy (LEO) in a valgus knee may be required to achieve optimum limb alignment and soft-tissue balance.
Introduction
Bone cuts and soft-tissue releases are the principal steps in TKA. However, some knees undergoing TKA may require an additional procedure in the form of an osteotomy. An osteotomy in primary TKA is usually indicated in rigid or severe deformities to facilitate soft-tissue balance and deformity correction, to concomitantly correct an extra-articular deformity or rarely to facilitate exposure of the joint. Frequently, in varus arthritic knees undergoing TKA, the medial and posteromedial side of the tibial plateau shows adaptive changes resulting in the formation of a prominent bony flare in this area (Fig. 11.1a). This causes local tenting of the medial soft-tissue structures and contributes to knee deformity and medio-lateral soft-tissue imbalance (Fig. 11.1b). A reduction osteotomy involves excision of this medial bony flare to decompress the medial soft-tissue structures [1, 2]. Rarely, despite extensive soft-tissue release and a reduction osteotomy, a knee deformity may be too rigid and/or the medio-lateral soft-tissue imbalance too severe to correct. In such cases a sliding medial condylar osteotomy (SMCO) in a varus knee [3] or a lateral epicondylar osteotomy (LEO) in a valgus knee [4] may be required to achieve optimum limb alignment and soft-tissue balance.
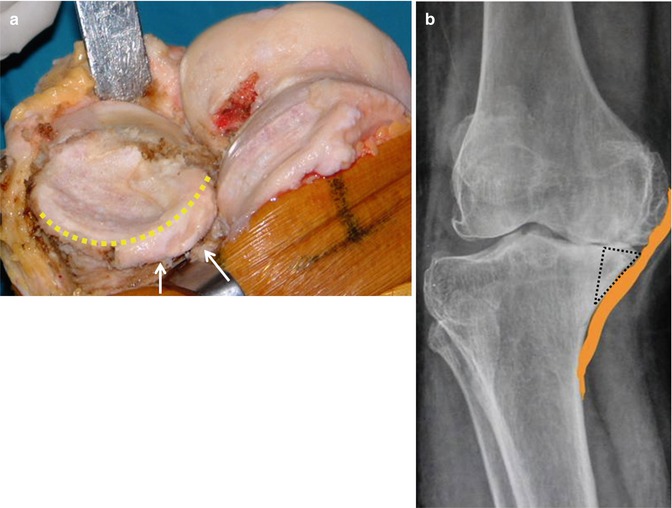
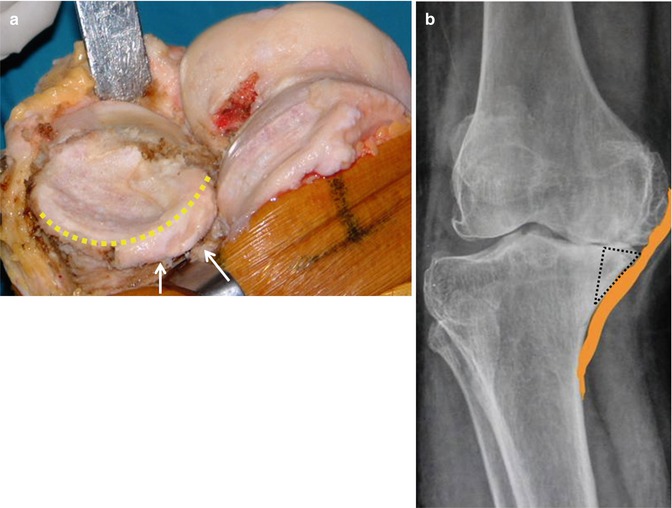
Fig. 11.1
Medial and posteromedial bony changes of the tibial plateau in varus arthritic knees. (a) Intraoperative photograph showing posteromedial bony flare (dotted line) of the tibial plateau (arrows). (b) Preoperative knee standing radiograph showing the bony flare (triangle) which causes tenting of the medial soft-tissue structures in varus arthritic knee
In cases with severe extra-articular deformities, a corrective osteotomy may be required simultaneously with the TKA in order to facilitate restoration of limb alignment [5–7]. However, in severe tibial extra-articular deformities where a medial closing wedge corrective osteotomy is required, the intact fibula at the apex may not allow complete closure at the osteotomy site, and therefore a segmental fibular osteotomy will have to be performed [6]. Sometimes in a stiff knee, excessive soft-tissue contractures and severe arthritis of the patellofemoral joint may result in poor exposure through the routine arthrotomy approach. A tibial tubercular osteotomy in such cases will facilitate adequate exposure of the joint for TKA. Hence, the main indications of an osteotomy in primary TKA are (a) correction of limb malalignment in knee arthritis due to an associated extra-articular deformity, (b) soft-tissue balance in severe and/or rigid knee deformities and (c) surgical exposure in a stiff or ankylosed knee joint. Each osteotomy as discussed above has a specific role to play during TKA (Fig. 11.2). This chapter aims to outline the indications and technique of various osteotomies used in primary TKA.
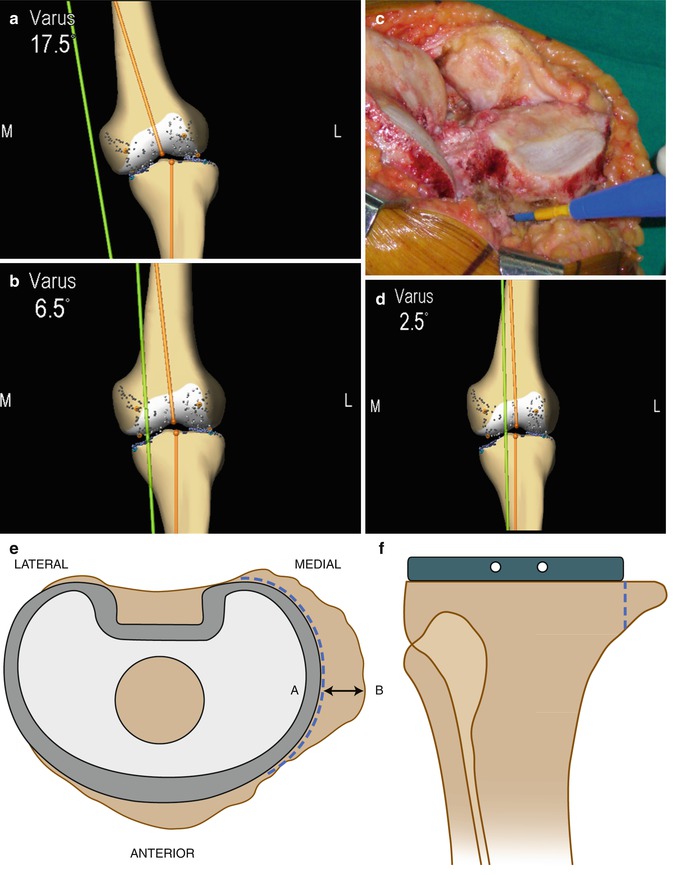
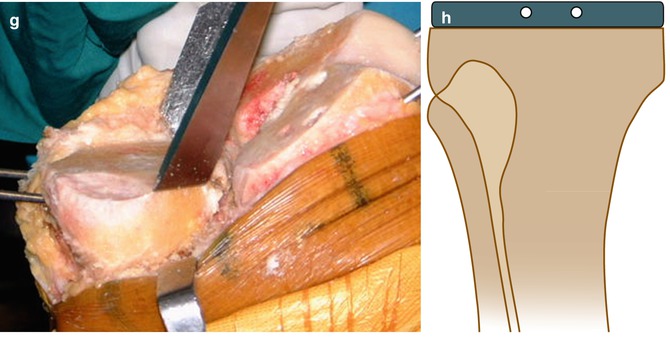
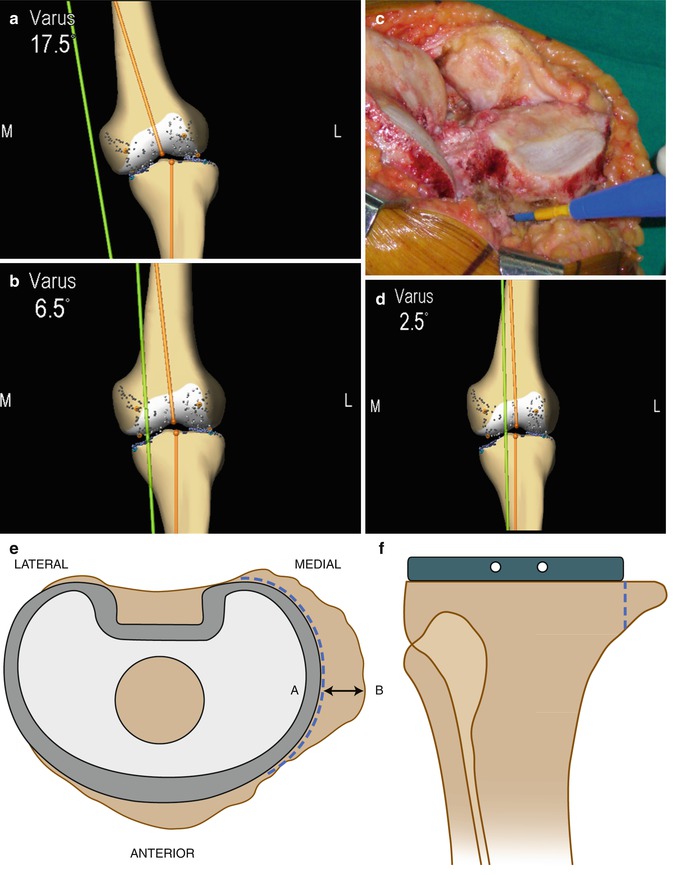
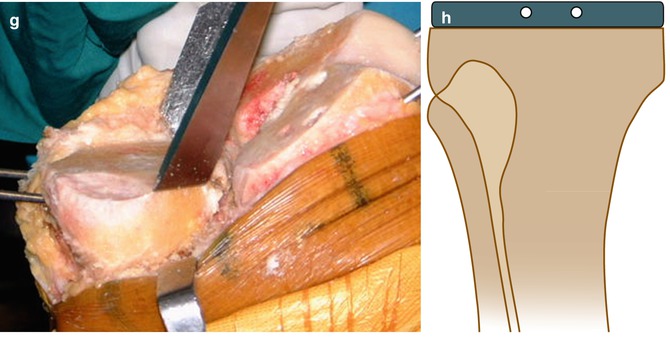
Fig. 11.2
Step-by-step technique of reduction osteotomy performed to achieve deformity correction and/or medio-lateral soft-tissue balance in varus arthritic knees undergoing TKA. (a, b) Step 1 – Intraoperative recording of varus deformity of 17.5° (a) and maximum correctibility up to 6.5° varus (b) on applying a valgus stress at the knee. (c) Step 2 – Posteromedial soft-tissue release (deep medial collateral ligament, posteromedial capsule and semimembranosus) to achieve deformity correction and medio-lateral soft-tissue balance. (d) Step 3 – Intraoperative recording of final correction achieved after posteromedial release shows a residual varus deformity of 2.5° on applying a valgus stress at the knee. Based on the “2-mm excision for 1° degree correction” principle, a reduction osteotomy of 5 mm is required in this case to achieve full correction (or neutral alignment). (e, f) Step 4 – Using the tibial tray of appropriate size as reference, the required amount of osteotomy is marked on the tibial cut surface (distance AB) along the margin of the tibial tray as seen in the axial (e) and frontal (f) views. (g, h) Step 5 – Reduction osteotomy performed along the marked line using an osteotome as seen intraoperatively (g) and on a schematic diagram (h)
Types of Osteotomies and Technique
Reduction Osteotomy of the Tibia
Principle: A reduction osteotomy involves excision of the posteromedial bony flare on the tibial plateau to decompress medial soft-tissue structures in a varus arthritic knee undergoing TKA (Fig. 11.1). This osteotomy works similar to the excision of osteophytes where they cause tenting and a bowstring effect on the adjoining medial soft-tissue structure (Fig. 11.1). Reduction osteotomy allows correction of deformity and medio-lateral soft-tissue balance without having to resort to excessive soft-tissue release and acts as a soft-tissue sparing step.
Indications: These include residual varus deformity of >2° (when measured using computer navigation) or medio-lateral soft-tissue imbalance (excessive medial tightness or excessive lateral laxity) despite sufficient medial soft-tissue release (deep MCL, posteromedial capsule and semimembranosus) in a varus arthritic knee undergoing TKA.
Technique: Reduction osteotomy can achieve deformity correction in a predictable manner using the “2-mm excision for 1° degree correction” formula especially in knees with <15° preoperative varus deformity [1]. However, this formula may not be as predictable in knees with >15° preoperative varus deformity due to associated severe medial soft-tissue contracture or lateral soft-tissue laxity and/or an associated extra-articular deformity [1]. A step-by-step technique for this osteotomy is illustrated in Fig. 11.2.
Precautions: Since reduction osteotomy can achieve deformity correction in a predictable manner (1° correction for every 2 mm of excision) especially in arthritic knees with <15° preoperative varus deformity, the surgeon should be careful not to perform it in limbs where the varus deformity is <5° or where the deformity is fully correctible as it may lead to excessive slackening of soft tissue medially and overcorrection [1]. Furthermore, the surgeon needs to take care that only the medial bony flare is excised (as previously measured in relation to the residual varus deformity and keeping the tibial tray as the reference) and the osteotomy should not be too medial and excessive as this may detach the superficial MCL which is attached 6–7 cm distal to the joint line (Fig. 11.3). In case the patient has a significant medial bone loss which has been built up with cement or bone graft, the fixation should be supplemented with a long tibial stem (Fig. 11.4).
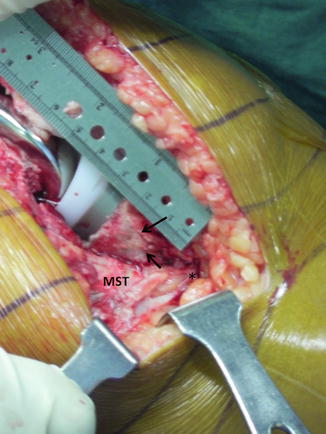

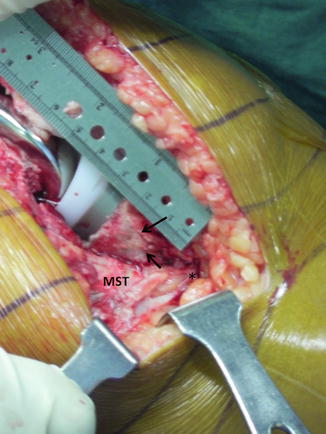
Fig. 11.3
Intraoperative photograph showing relation of the reduction osteotomy (arrows) to the medial soft-tissue sleeve (MST). Note that the attachment of the superficial MCL (asterisk) is distal to the distal border of the reduction osteotomy (arrows)

Fig. 11.4
Pre- and postoperative standing knee radiograph of a case with varus arthritis in which reduction osteotomy has been performed as part of TKA. (a) Preoperative radiograph showing prominent medial tibial bony flare with medial tibial bone loss. (b) Postoperative radiograph of the same patient showing final alignment after TKA with a reduction osteotomy. The medial bone loss has been built up using bone autograft fixed with Kirschner wires and supplemented with a long tibial stem
Postoperative Care: Postoperative physiotherapy is similar to that of a routinely performed TKA and no postoperative bracing is required.
Sliding Medial Condylar Osteotomy (SMCO)
Principle: A sliding medial condylar osteotomy involves detachment of a bony segment medially from the medial femoral condyle with the medial collateral ligament (MCL) attached to it. This allows distal displacement and fixation of the femoral attachment of the MCL (while preserving its attachment to bone) to increase the medial gap vis-à-vis the lateral gap in varus arthritic knees during TKA. Subperiosteal stripping of tibial attachment of MCL or its detachment from the femoral side with a wafer of bone is an imprecise technique and carries the risk of overrelease and medio-lateral instability [8], whereas SMCO is precise and quantitative and allows repositioning the MCL more accurately.
Indications: These include rigid, recalcitrant varus deformities not amenable to full correction of limb alignment and/or medio-lateral imbalance despite extensive medial soft-tissue release (except superficial MCL and pes anserinus) and a reduction osteotomy during TKA.
Technique: A step-by-step technique for this osteotomy is illustrated in Fig. 11.5.
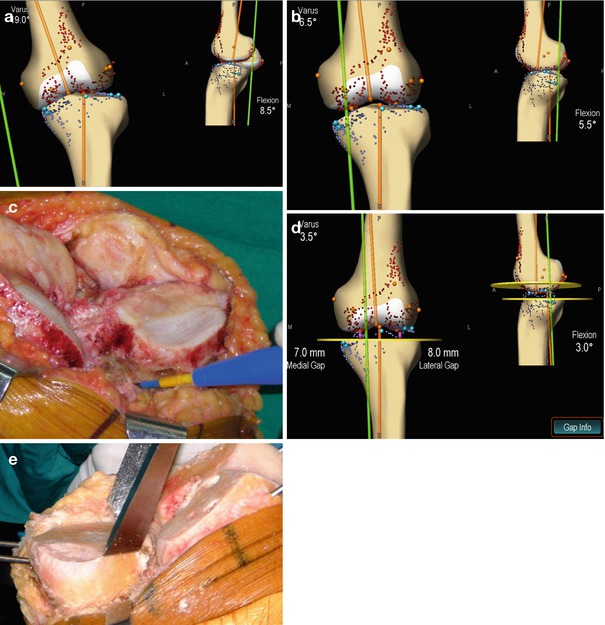
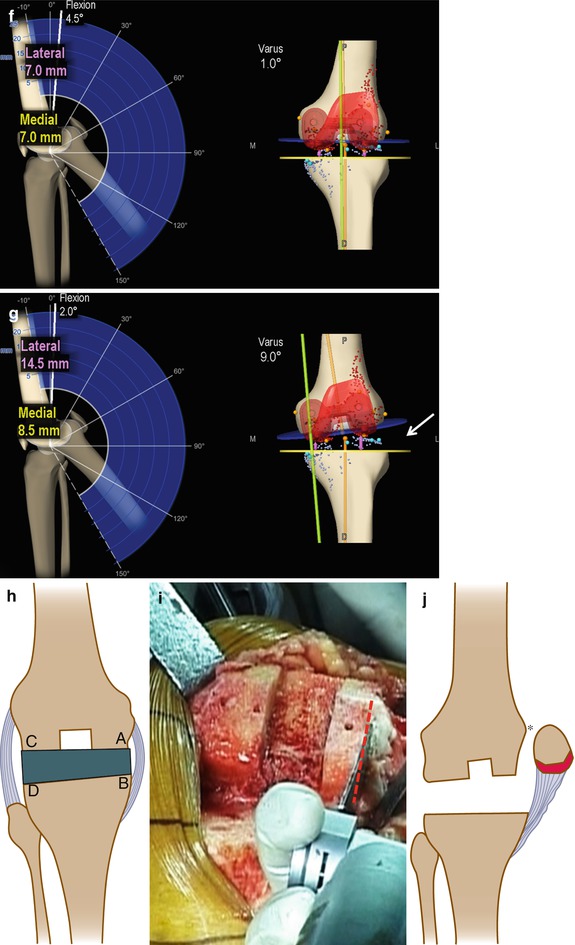
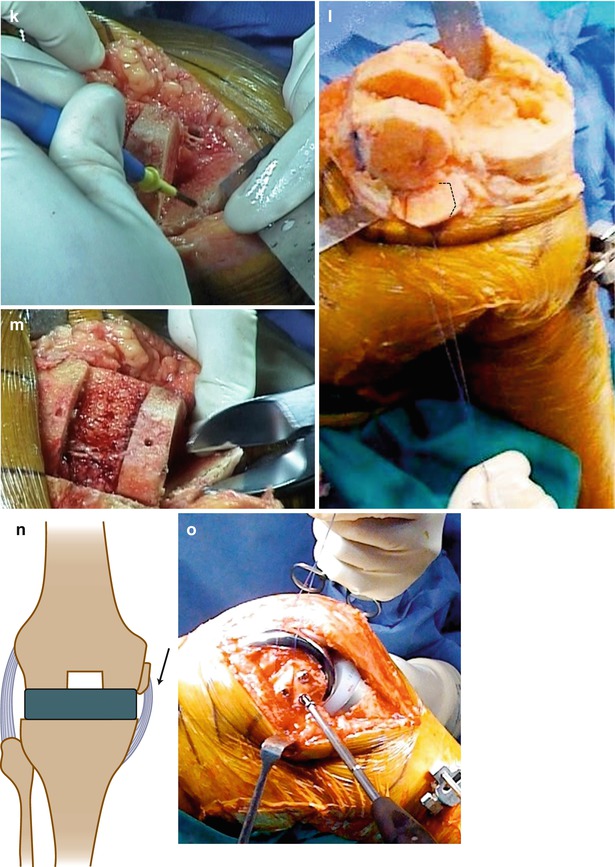
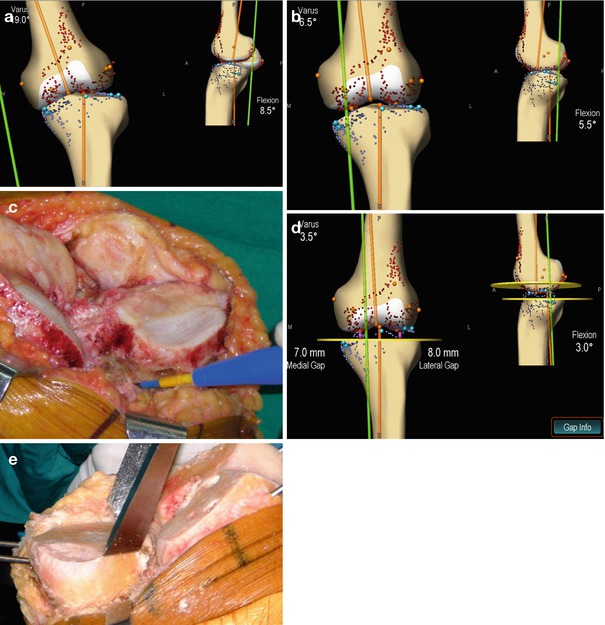
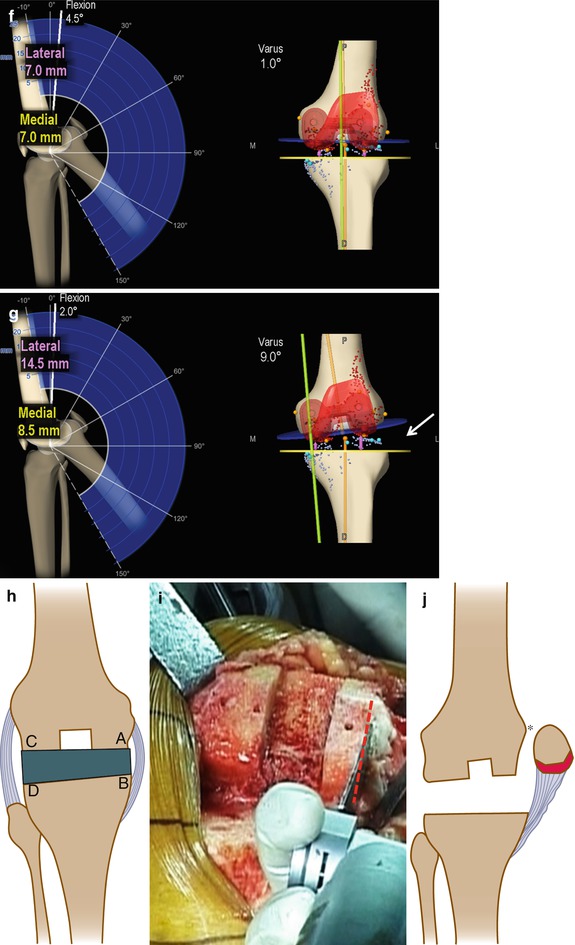
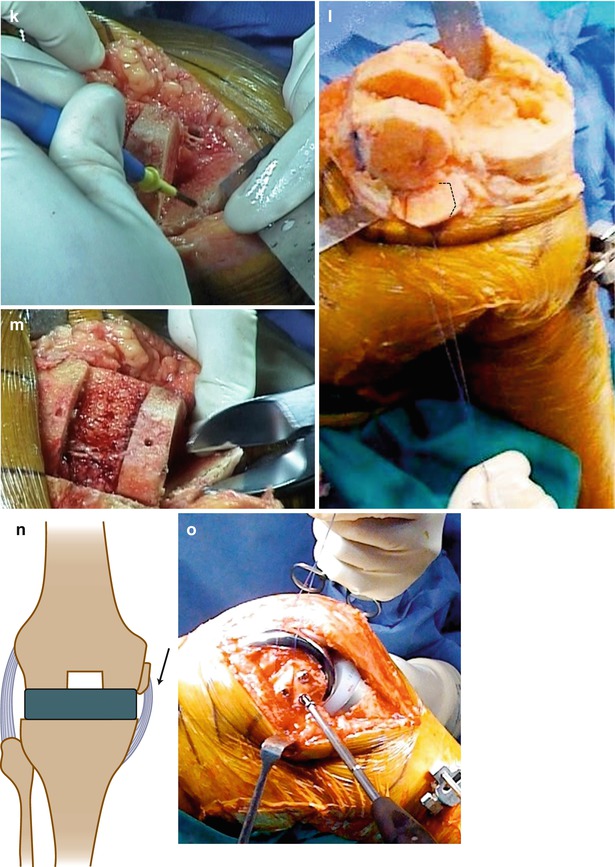
Fig. 11.5




Step-by-step technique of sliding medial condylar osteotomy (SMCO) performed to achieve deformity correction and/or medio-lateral soft-tissue balance in varus arthritic knees undergoing TKA. (a, b) Step 1 – Intraoperative recording of varus deformity of 17.5° (a) and maximum correctibility up to 6.5° varus (b) on applying a valgus stress at the knee. (c) Step 2 – Posteromedial soft-tissue release (deep medial collateral ligament, posteromedial capsule and semimembranosus) to achieve deformity correction and medio-lateral soft-tissue balance. (d) Step 3 – Intraoperative recording shows a residual varus deformity of 3.5° on applying valgus stress at the knee despite posteromedial soft-tissue release. A reduction osteotomy will have to be performed to correct this residual deformity. (e) Step 4 – Reduction osteotomy done to correct the residual varus deformity based on the “2-mm excision for 1° degree correction” principle. (f, g) Step 5 – Intraoperative recording shows complete correction of deformity after reduction osteotomy (f): however, on maximum varus stress to the knee the same knee shows excessive lateral soft-tissue laxity (arrow) vis-à-vis the medial side (g). A SMCO is now required to achieve medio-lateral soft-tissue balance. (h) Step 6 – The difference between the medial and lateral gap in knee extension (distance CD–AB) is measured to determine the amount by which the medial condylar block needs to be shifted distally. This distance can be determined using either navigation or a measuring scale. (i, j) Step 7 – Plane of the osteotomy cut is marked on the medial femoral condyle. The cut starts 5 mm lateral to the medial edge of the bony medial condyle (red line) and continues obliquely in the superomedial direction to exit distal to the adductor tubercle (asterisk). The osteotomy is performed using a reciprocating saw. (j, k) Step 8 – The amount by which the medial condylar block needs to be shifted distally is marked on the block using a measuring scale and electrocautery. (l) Step 9 – The condylar block is now controlled using sutures (Vicryl no. 1) passed through its soft-tissue attachment. Dotted line signifies amount of bone marked on the condylar block which will be excised. (m) Step 10 – The amount of bone previously marked on the condylar block is now excised using a bone cutter. (n) Step 11 – The condylar block is now gently shifted distally and repositioned in place using the attached sutures. The medio-lateral balance and alignment are then checked with trial implants in full extension and the knee in 90° flexion with the condylar block in its new position. (o) Step 12 – After cementing of the final implant, the condylar block is fixed in position using two to three cancellous screws with the knee in 45° flexion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








