Chapter 41 Osteoporosis
Clinicians can add quality to the years of life of patients with osteoporosis through the use of an interdisciplinary approach. This condition is the most prevalent metabolic bone disease in the United States and is a major public health problem. The direct and indirect cost of osteoporosis in the United States alone is estimated to be more than $14 billion annually.53 Much of this expense relates to hip fractures. In 15% to 20% of hip fracture cases, the outcome is fatal.57,62
The World Health Organization has defined osteoporosis as bone mineral density (BMD) of 2.5 standard deviations below the peak mean bone mass of young healthy adults.107 The T score shows the amount of one’s bone density compared with a young adult (at the age of 35) of the same gender with peak bone mass. The Z score is calculated in the same way, but the comparison is made with someone of the same age, sex, race, height, and weight. The Z score is adjusted for an individual’s age, and the T score is not. For example, a 75-year-old woman with a Z score of −1.0 is one standard deviation below the BMD of an average 75-year-old woman, but her T score may be −3.0 because she is three standard deviations below the BMD of an average 35-year-old woman. Normal BMD is a T score −1 or greater; osteopenia, a T score between −1 and −2.5; osteoporosis, a T score −2.5 or less; and severe osteoporosis, a T score −2.5 or less with fracture. In the asymptomatic stage, osteoporosis is characterized simply by decreased bone mass without fracture. Osteoporosis becomes clinically problematic only when the bone fractures.
Bone Function and Structure
Bone serves as a mechanical support for musculoskeletal structures, as protection for vital organs, and as a metabolic source of ions, especially calcium and phosphate. Despite its appearance, bone is an active tissue. To maintain its biomechanical competence, bone tissue undergoes continuous change and renewal so that older bone tissue is replaced by newly formed bone tissue. Approximately 20% of bone tissue is replaced annually by this cyclic process. There are two types of bone cells: osteoclasts, which resorb the calcified matrix, and osteoblasts, which synthesize new bone matrix.65
Bone Remodeling
The number of active remodeling units in trabecular bone is about 3 times greater than in cortical bone. The physical endurance of any bone is affected by the percentage of cortical bone involved in its structure. Trabecular bone is more active metabolically than cortical bone because of the considerable surface exposure areas. Consequently, more bone loss occurs at the trabecular areas when resorption is greater than formation. The vertebrae consist of 50% trabecular bone and 50% cortical bone, whereas the femoral neck consists of 30% trabecular bone and 70% cortical bone. When bone turnover increases, bone loss and osteoporosis occur in the vertebrae before they occur in the femoral neck.
Pathogenesis
Trabecular (or cancellous) bone represents about 20% of skeletal bone mass and makes up 80% of the turnover media. The cortex makes up only 20% of the turnover media and is made of compact bone. It represents 80% of skeletal bone mass. In both cortical and trabecular bone, bone remodeling is initiated with the activation of osteoclasts. The resulting resorption sites are then refilled by osteoblastic activities, a process called bone formation. If the amount of bone resorbed equals the amount formed, the bone loss is zero. The remodeling process does not result in zero balance after age 30 to 35 years, however, and after this age the normal process of remodeling results in bone loss.63
Certain conditions, such as hyperparathyroidism or thyrotoxicosis, can increase the rate of bone remodeling. These conditions increase the rate of bone loss, which results in high-turnover osteoporosis. The secondary causes of osteoporosis are associated with an increased rate of activation of the remodeling cycle. Although factors such as calcium intake, smoking, alcohol consumption, physical exercise, and menopause are important factors in determining BMD, genetic factors are the major determinant and contribute to 80% of the variance in peak BMD.16 Fracture incidence related to osteoporosis is lower in men than in women because the diameter of vertebral bodies and long bones is greater in men at maturity and bone loss is less (about half that of women) throughout life.67
Classification of Osteoporosis
Osteoporosis can be primary or secondary to other disorders that result in bone loss. The most common causes of osteoporosis are listed in Box 41-1. The most common type of osteoporosis is either postmenopausal or age related.56
BOX 41-1 Common Causes of Osteoporosis
Modified from Sinaki M: Metabolic bone disease. In Sinaki M, editor: Basic clinical rehabilitation medicine, ed 2, St Louis, 1993, Mosby. Used with permission of Mayo Foundation for Medical Education and Research.
Acquired (Primary and Secondary)
Generalized
Primary osteoporosis is the rare disorder of idiopathic juvenile osteoporosis. This type of osteoporosis typically occurs before puberty (between ages 8 and 14 years), and patients present with osteoporosis that is progressive over 2 to 4 years in association with multiple axial or axioappendicular fractures. Remission usually occurs by the end of the 2- to 4-year course.36 In this type of osteoporosis, the process of bone formation is normal but osteoclastic activity increases, resulting in increased bone resorption. This type of osteoporosis is most evident in the thoracic and lumbar spine and needs to be distinguished from juvenile epiphysitis or Scheuermann disease. It is usually self-limiting, but the radiographic appearance might not return to normal. The laboratory values are typically normal, and the diagnosis is made by exclusion.
Hormones and Physiology of Bone
The rate of bone remodeling can be increased by parathyroid hormone (PTH), thyroxine, growth hormone, and vitamin D (1,25-dihydroxyvitamin D3 [1,25(OH)2D3]). It can be decreased by calcitonin, estrogen, and glucocorticoids.46
Role of Sex Steroids
The main endocrine function that occurs at menopause is loss of secretion of estrogen and progesterone from the ovaries.34,46,67 The premenopausal ovary produces primarily estradiol. Progesterone secretion, which occurs cyclically after ovulation in the premenopausal stage, also decreases to very low levels in the postmenopausal stage. These changes in circulating sex steroids are gradual in a woman’s sexual reproductive life. The premenopausal ovary also produces androgens, especially testosterone. The circulating testosterone levels decrease after menopause. The major source of estrogen in postmenopausal women is conversion from dihydroepiandrostenedione. The latter is then converted into androstenedione, which changes into estrone in fat cells. Estrone is the major source of estrogen in postmenopausal women.
Men do not have the equivalent of menopause, but in some elderly men bone mass decreases along with a decline in gonadal function. The testosterone level in men decreases with age as a result of a decreased number of Leydig cells in the testes. Male hypogonadism is typically associated with bone loss.41
Other Factors Affecting Bone Mass
Several other factors can contribute to the reduction of sex-related steroid levels. In hyperprolactinemia, which is due to a prolactin-secreting pituitary tumor, failure of the gonadal axis results in a substantial loss of bone. Amenorrheic athletes who exercise excessively, such as high-mileage runners or ballet dancers who have lower-than-normal body weight, have lower circulating estradiol, progesterone, and prolactin levels. Their amenorrhea is associated with hypothalamic hypogonadism, which leads to excessive bone loss. This bone loss can be mostly reversed when training distances are decreased.14,44 With weight gain and improvement in nutrition, these young women can facilitate resumption of menses and reversal of bone loss.7,21,106 Reduction of sex steroid concentrations is not the only cause of bone loss. Other factors such as race, genetics, nutrition, physical exercise, and lifestyle can also contribute to the rate of bone loss after an ovariectomy or natural menopause.72 It is well known that bone must be physically stressed to be maintained. A considerable body of data shows that the rate of change in strain also influences bone growth and remodeling.52
Effect of Aging on Bone Mass
It appears that special forms of vitamin K therapy in elderly persons can be associated with a reduction in the rate of bone resorption, demonstrated by decreased excretion of urinary hydroxyproline. Further studies are needed in this area. Studies have shown that calcium absorption is less efficient in elderly people.32 Bone loss also has been related to deficiencies in trace metal elements, such as copper, zinc, and magnesium, but this issue is not fully resolved.
Plasma calcitonin levels are higher in men than in women. Calcitonin levels do not change with age. Studies have shown that estrogens stimulate calcitonin secretion.99,100 Thyroid hormone levels typically show no change or are slightly decreased with age. The PTH level increases with age, perhaps because of mild hypocalcemia and decreased 1,25(OH)2D3 concentration. This reduction in the active form of vitamin D can be due to decreased consumption of dietary vitamin D, decreased exposure to sunlight, decreased skin capacity for vitamin D conversion, reduced intestinal absorption, and reduced 1-α-hydroxylase activity.
Several studies have shown that the level of physical activity decreases with aging.73 This is important because physical strain and mechanical load also positively affect bone mass.23 Exercise is known to stimulate the release of growth hormone or other trophic factors that can stimulate osteoblastic activity.20 Optimal nutrition and physical activity are necessary to achieve the genetic potential for bone mass. The peak bone mass attained by young adulthood is a major determinant of bone mass in later life. Female gymnasts, both children and college-aged athletes, reportedly have higher BMD than swimmers.6,19 Nutrition also can affect both bone matrix formation and bone mineralization. In general, in estrogen-deficient women, calcium intake of 1500 mg/day and 800 international units/day of vitamin D are recommended.
Clinical Manifestations of Osteoporosis
Osteoporosis is typically a “silent disease” until fractures occur. Osteoporotic vertebral fractures can go unnoticed until they are incidentally seen on a chest radiograph. Appendicular fractures, however, typically require immediate attention. The fact that a fracture resulted from osteoporosis should not affect the orthopedic method of management. The most common areas for osteoporotic fractures are the midthoracic and upper-lumbar spine (Figure 41-1),81 hip (proximal femur), and distal forearm (Colles fracture). The highest incidence of fractures is in white women. The female/male ratio is about 7:1 for vertebral fractures, 2:1 for hip fractures, and 5:1 for Colles fractures. It has been estimated that after menopause a woman’s lifetime risk of sustaining an osteoporotic fracture is 1 in 2 or 3.51
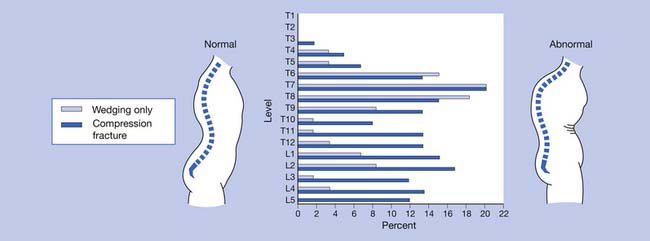
FIGURE 41-1 Incidence of wedging and compression fractures at various levels of the spine.
(Modified from Sinaki M, Mikkelsen BA: Postmenopausal spinal osteoporosis: flexion versus extension exercises, Arch Phys Med Rehabil 65:593-596, 1984, with permission.)
Fractures and Management
The relationship between bone mass and spinal fractures has been extensively studied, and it is known that fracture risk increases as bone mass decreases. For every standard deviation of decrease in BMD, the risk of osteoporotic fracture of the spine increases 1.5- to 2-fold, and the risk of hip fracture increases 2.6-fold.30 Another predictor of fracture risk is age itself. The risk of fracture as a result of osteoporosis doubles every 5 to 7 years.30 It is not clear whether age-related changes in bone density or bone quality are factors that increase the risk of fractures caused by falls.
Vertebral Fracture
Acute pain that occurs in the absence of a previous fracture is usually due to compression fractures of the vertebrae. Sometimes a minor fall or even an affectionate hug can cause a compression fracture. The compressed vertebrae might not be apparent on radiographs for up to 4 weeks after the injury.56 Compression fractures usually result in acute pain that later resolves (Box 41-2).71 The spinal deformity that can result from these fractures can produce chronic pain.71
BOX 41-2 Management of Acute Pain in Patients With Osteoporosis
Modified from Sinaki M: Metabolic bone disease. In Sinaki M, editor: Basic clinical rehabilitation medicine, ed 2, St Louis, 1993, Mosby. Used with permission of Mayo Foundation for Medical Education and Research.
Kyphotic postural change is the most physically disfiguring and psychologically damaging effect of osteoporosis.85 The incidence of osteoporosis can be substantially decreased only by early detection and subsequent intervention in high-risk patients.
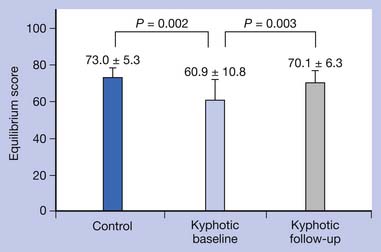
Disproportionate weakness in back extensor musculature relative to body weight or spinal flexor strength considerably increases the possibility of compressing the vertebrae in the fragile osteoporotic spine. Recognition and improvement of decreased back extensor strength can enhance the ability to maintain proper vertical alignment.69 The geriatric population has an increased risk of debilitating postural changes because of several factors, the two most apparent being a greater prevalence of osteoporosis and an involutional loss of functional muscle motor units.27,50 Development of kyphotic posture not only can predispose to postural back pain but also can increase the risk of falls.48 Several other factors also can contribute to the risk for falls (Box 41-3).
BOX 41-3 Factors Contributing to Risk for Falls
Modified from Sinaki M: Falls, fractures, and hip pads, Curr Osteoporos Rep 2:131-137, 2004, with permission.
Extrinsic
Intrinsic
Chronic spinal pain can be due to the deformity caused by vertebral wedging and compression, as well as by secondary ligamentous strain. These deformities are often difficult to distinguish from the usually associated disk deterioration. The intervertebral disks undergo the most dramatic age-related changes of all connective tissues.1 With aging, there is an increase in the number and diameter of the collagen fibrils in the disk. This change is accompanied by a progressive decrease in disk resilience. Loss of distinction between the nucleus pulposus and the annulus fibrosus eventually occurs.
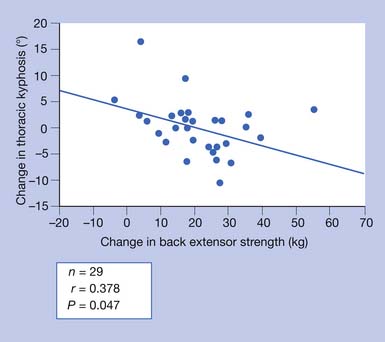
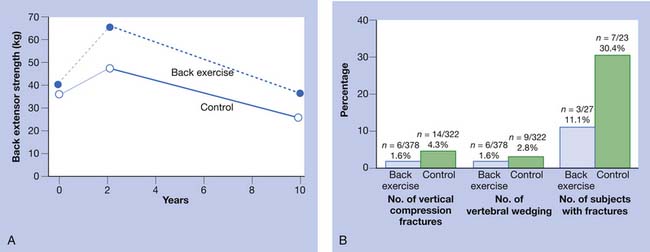
Chronic back pain secondary to osteoporosis is related to postural changes resulting from vertebral fractures.85 Strong back muscles contribute to good posture and skeletal support (Figure 41-2).33,84,89 One controlled study showed the long-term effects of back extensor resistance training 8 years after cessation of the exercise.86,91 The women in the study were not receiving hormone replacement therapy. Compared with the exercise group, the control group had a 2.7 times greater number of vertebral fractures at 10-year follow-up evaluation.91 The pain and skeletal deformity associated with osteoporosis might secondarily reduce muscle strength. The reduction in muscle strength can further exacerbate the postural abnormalities associated with this condition (Figure 41-3).
Chronic pain can also be due to microfractures that are visible only on bone scanning and which can occur continuously. Management of chronic osteoporosis-related pain is outlined in Box 41-4. Prescription of opiate analgesics, such as codeine sulfate or its derivatives, should be undertaken judiciously because their use can cause constipation.68
BOX 41-4 Management of Chronic Pain in Patients With Osteoporosis
Modified from Sinaki M: Metabolic bone disease. In Sinaki M, editor: Basic clinical rehabilitation medicine, ed 2, St Louis, 1993, Mosby. Used with permission of Mayo Foundation for Medical Education and Research.
New Hypothesis on the Most Effective Exercise to Reduce the Risk for Vertebral Fracture
After a 10-year follow-up study,91 the author developed the following hypothesis: “Back strengthening exercises performed in a prone position rather than in vertical position (nonloading) can decrease risk of vertebral fractures through improvement of horizontal trabecular connections.”79 The exercise needs to be progressive, resistive, and nonloading to avoid vertebral compression fracture.
Vertebroplasty and Kyphoplasty
Vertebroplasty and kyphoplasty procedures are used for the management of vertebral fractures. These procedures involve the injection of acrylic cement (such as polymethylmethacrylate) into a partially collapsed vertebral body. Jensen et al.35 found that 63% of osteoporotic patients who underwent vertebroplasty decreased their use of opiates and analgesics for pain control, 7% increased their use, and 30% continued on the same use. More recently, two multicenter randomized controlled trials evaluating vertebroplasty demonstrated no significant difference in pain relief when compared with a sham procedure.5,37 Vertebroplasty does not substitute for rehabilitative measures that are needed after fracture.31,59 One study showed significantly fewer vertebral refractures after vertebroplasty in patients who received instruction for back extension exercises.31 The author recommends a rehabilitation program, especially back extension exercises, for osteoporosis management.
Hip Fracture
Falls and hip fractures can be life threatening.55,101 In addition to weakness of the lower limbs, one of the contributing factors to falls is disequilibrium of individuals with spinal kyphotic posture.78 The kyphotic posture places the center of gravity closer to the limit of stability.93 Measures that reduce instability, such as proper exercise program and use of a weighted kypho-orthosis (WKO), can reduce both the fear of falls and the risk of falls (Figure 41‑4).93
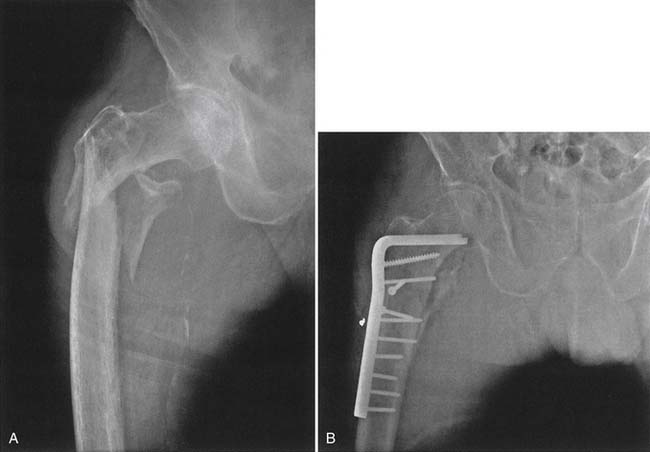
The trochanteric hip fracture creates fewer problems, despite the fact that the fracture engages more bone than the femoral neck fracture. The operative treatment of choice is internal fixation (Figure 41-5). The postoperative course for all hip fractures, regardless of whether internal fixation or joint arthroplasty is done, is less eventful if physical therapeutic measures are used postoperatively, including the use of gait aids with partial weight-bearing on the operative side. Only for patients with severely comminuted fractures or fractures in which the operative result has been unsatisfactory is the restriction of weight-bearing to no weight-bearing needed.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree