Fig. 22.1
Wheelchair-related lateral ankle decubitus pressure sores. Nonambulatory patients likely spend more hours of the day in a wheelchair or motorized powerchair than in bed which increases the risk of wheelchair-related foot and ankle pressure sores. Contracture of the lower extremity associated with neuromuscular conditions creates lateral prominence which further predisposes to lateral pressure from the foot rest

Fig. 22.2
Lateral ankle pressure sores associated with ankle-foot orthotic (AFO) bracing. AFO bracing is commonly employed for foot and ankle weakness or contracture deformity. (a) Neuromuscular disorders like stroke, cerebral palsy, and traumatic brain injury commonly result in plantar flexion and inversion deformity at the ankle which creates lateral malleolar prominence and is a source of pressure associated with AFO bracing. (b) The brace is intended to maintain positioning at the foot and ankle which naturally applies pressure in the region of the lateral malleolus. Early intervention with brace modifications is helpful, but medical or surgical treatment to reduce spastic contracture may be necessary
Treatment protocols for osteomyelitis of the distal fibula are not well described in the literature. Osteomyelitis is largely a late-stage presentation which commonly results in failure to heal a decubitus ulcer despite months of expensive wound care. The late-stage development of bone exposure and resultant osteomyelitis of the fibula is difficult to predict in the early stages of wound management. Full-depth compromise of the overlying soft tissue is likely the main determining factor since the bone becomes immediately exposed when a truly full-thickness eschar finally sloughs after months of monitoring. Factors that lead to poor wound healing, including poor nutrition, circulatory compromise, and edema, further predispose to soft tissue infection and resultant osteomyelitis. Early intervention for lateral malleolar decubitus ulceration primarily involves off-loading, local wound care, edema control, and vascular intervention if needed. Surgery is primarily considered once the underlying bone becomes exposed or when early signs of infection develop. Consideration of surgical treatment for equinovarus contracture deformity can also be considered early in the course of treating pressure sores.
Conservative surgical intervention is not likely to cure osteomyelitis of the distal fibula since infection can be extensive throughout the lateral malleolus and wound defects are difficult to close primarily. Wide resection of the distal fibula may be the most prudent approach for patients confined to a wheelchair as extensive resection of bone allows mobility of the surrounding tissue which aids in primary closure. Complete distal fibulectomy is less practical for ambulatory patients as this is likely to destabilize the ankle and results in exposure of the ankle joint, talus, and tibia which may lead to contiguous spread of infection [8]. Successful wound healing is a critical aspect of successful surgical management for osteomyelitis of the distal fibula since prolonged bone exposure following bone resection often leads to persistent infection. Our preferred surgical approach involving wound excision, lateral cortical debridement of the distal fibula, bone biopsy, and advanced wound closure techniques including negative-pressure wound therapy (NWPT) or local flap closure of the wound is the focus of this chapter. Extensive soft tissue loss can also be treated with various musculocutaneous pedicle flaps or free muscle flaps followed by skin grafting [9–17]. Wide resection of the infected wound and distal fibula with delayed fusion of the ankle is discussed in Chap. 10.
Natural Progression of Lateral Ankle Decubitus Ulceration with Late-Stage Development of Osteomyelitis
Lateral ankle pressure sores typically follow a natural healing progression from initial decubitus insult to eventual healing that may be protracted for perhaps 1 year in duration depending on the size and stage of ulceration and effectiveness of off-loading. The superficial skin may initially form a blister while the compromised deeper soft tissues eventually become a black, leathery eschar that remains firmly attached to the underlying tissue and bone. Minimal topical care or debridement is necessary during the early phase of eschar formation or maturation since the eschar serves as a natural barrier to infection. It is important to minimize edema in the extremity and protect the peripheral tissues against ongoing decubitus pressure. Antibiotics are not necessary or helpful during this stage, and expensive wound care treatments are of little value while the eschar remains intact. Assessment of extremity circulation may identify the need for vascular intervention which is more useful at this early stage rather than later when the wound becomes compromised with infection. The patient may remain ambulatory for lateral malleolar decubitus ulcers since mobility minimizes the risk of ongoing decubitus pressure. Non-bed-related sources of decubitus pressure should be rectified including pressure while sitting in a wheelchair and ill-fitting AFO braces.
Debridement of the eschar eventually becomes necessary during the course of eschar maturation. Blistering of the superficial skin may occur early, and loosely adhered tissue can be removed once the blister becomes dessicated. Deep debridement is otherwise delayed until the edges of the eschar become softened, macerated, and delaminated months into the healing process. Granulation tissue around the margin of the eschar is frequently noted at this time. The central aspect of the eschar typically remains firmly attached to the deep periosteum and should be left in place as a natural barrier to infection. The ideal healing process would involve progressive formation of granulation tissue as the eschar delaminates from the peripheral margin toward the center of the wound [18]. Epithelialization at the intact skin margin and simultaneous circumferential contraction toward the center of the wound allows progressive healing. Normal healing takes months and frequently more than 1 year for large wounds. The central aspect of the eschar eventually softens or “ripens” to the point where it is no longer advantageous and should be removed. A soft, necrotic, and foul-smelling eschar eventually becomes a harbinger for bacteria and may predispose to the onset of infection. This slow approach to eschar removal can oftentimes be performed in the office and without anesthesia provided that only necrotic and loose tissue is removed. Final eschar excision may require an operating room procedure for patients with intact sensation. Our routine is to begin hydrating or enzymatic debriding agents once granulation tissue is exposed around the peripheral margin of the eschar or when the eschar is completely removed.
Complete eschar removal finally allows assessment of the depth of necrosis and potential exposure of the fibula. The distal fibula is oftentimes covered with nonviable slough which represents unhealthy periosteum and devitalized fibrotic tissue. The fibula may become exposed but is frequently not yet infected at the time of complete eschar removal. Lateral malleolar decubitus wounds differ from heel decubitus wounds in that the heel has a thick pad of compartmentalized fat separating the superficial skin from the deep bone allowing greater healing potential once the eschar is removed.
Early workup for osteomyelitis is typically not necessary since osteomyelitis is more likely to develop over time once the eschar sloughs. Assessment of probe-to-bone status, baseline inflammatory marker labs, and X-rays are oftentimes obtained at this point. The patient may still be months away from the onset of fibular osteomyelitis, but consideration could be given to early decortication and rotational flap coverage of the wound. This decision is oftentimes based on the size of the wound, the extent of bone exposure, the quality of the surrounding tissue, and the relative health of the patient. The typical patient with a lateral malleolar decubitus ulcer is not a great surgical candidate, yet waiting for infection to develop may compromise the healing potential of this potentially life-altering situation. One year of wound treatment can be very disheartening and frustrating for an ambulatory patient who is unwilling to accept the risk of potential limb loss. Wheelchair-bound patients may be more amenable to a wait-and-see approach. Ultimately, the decision for early surgical intervention is difficult since flap surgery puts adjacent tissue at risk and surgery may expose uninfected bone to potential contamination.
Diagnosis of Distal Fibular Osteomyelitis
Standard X-rays are not very effective at identifying early onset of osteomyelitis in the distal fibula. Erosion of the lateral cortex is typically the first finding yet the cortex on the distal fibula is relatively thick, and it may take months to see radiographic signs of cortical erosion (Fig. 22.3). Abnormality of the overlying soft tissue due to the leathery eschar or sloughing tissue also changes the appearance of bone density on X-ray. Serial MRIs during a 12-month course of wound monitoring is not practical or cost-effective. MRI is typically reserved for patients with high suspicion for osteomyelitis with desire to evaluate the extent of infection and to rule out soft tissue abscess, ankle joint sepsis, and involvement of the tibia or talus. The diagnosis of osteomyelitis is best made by evaluating the entire clinical picture including local wound appearance, probe-to-bone status, infection marker labs, and X-rays. An abrupt jump in erythrocyte sedimentation rate (ESR) from a baseline normal value to a high double-digit value raises suspicion for new onset of osteomyelitis; however, this approach can be misleading since an elevated ESR is not specific to the ankle condition, which makes baseline lab values clinically useful.


Fig. 22.3
Radiographic evaluation for osteomyelitis. X-rays are not very sensitive at detecting early onset of osteomyelitis in the distal fibula, but periosteal reaction or cortical erosion may eventually become apparent. Early X-rays are primarily useful for late-stage comparison once osteomyelitis develops. The lateral cortex is the most likely location for osteomyelitis associated with decubitus ulceration. Note the obvious soft tissue deficit over the distal fibula which interferes with assessment of bone density
Osteomyelitis typically occurs from contiguous spread of infection from the overlying decubitus wound. Lack of clinical signs of wound infection therefore would suggest the absence of osteomyelitis. Chronic wounds that are covered in slough are always contaminated with bacteria, and wound culture is not an accurate way to identify infection or causative organisms. Bone biopsy is ultimately the ideal diagnostic test to identify osteomyelitis which is discussed in Chap. 4. The primary risk of bone biopsy when wounds are present is that violation of the cortex exposes the cancellous bone to potentially contaminating organisms. Festering and untreated osteomyelitis, on the other hand, will likely preclude progressive wound healing despite costly and burdensome wound care, thus making bone biopsy a valued test despite inherent risks.
Bone scan should be considered for patients unable to undergo MRI and is more cost-effective than bilateral MRI for patients with bilateral involvement. A negative bone scan largely rules out osteomyelitis with the exception that severe arterial insufficiency could lead to a false negative bone scan. MRI is useful from a surgical planning standpoint regarding extent of incision and drainage procedures, ideal location of bone biopsy, involvement of adjacent bone structures, and involvement of the peroneal tendons. The lateral ankle tendons are commonly exposed within a chronic lateral malleolar ulcer and oftentimes become diseased or infected. The peroneal tendon sheath can also become a pathway for spread of infection into the leg or foot. The peroneal tendons can be inspected at the time of surgery but avoiding interruption of the tendon sheath is desirable if the tendons appear uninvolved on MRI. Findings on MRI consistent with inflammation within the distal fibula should not be automatically interpreted as necrotic or dead bone. Direct visualization of bone viability at the time of surgery allows for surgeon judgment regarding the potential to preserve the distal fibula with conservative lateral cortical debridement and postoperative antibiotic therapy. It is desirable to preserve a functional lateral malleolus unless the bone is truly dead and necrotic [8]. CT is a third option for advanced imaging although MRI and bone scan may have greater clinical utility.
Tendon Lengthening Options for Neuromuscular Contracture of the Foot and Ankle
Surgical treatment of equinovarus contracture deformity may be necessary for AFO-related lateral malleolar ulcers in patients with contracture associated with neuromuscular disorders. Tendon lengthening procedures allow proper positioning in the brace which ultimately reduces lateral ankle decubitus pressure [7]. The posterior tibial tendon is lengthened to reduce varus contracture of the foot and ankle. For ambulatory patients, a sliding Z-lengthening procedure allows side-to-side repair after lengthening. Nonambulatory patients with chronic edema and expected permanent use of AFO bracing can be treated with a smaller, almost percutaneous incision and complete posterior tibial tenotomy (Fig. 22.4). Equinus ankle contracture is addressed with Achilles tendon lengthening (TAL) which can be performed using multiple small incisions or as an open procedure (Fig. 22.5). The minimally invasive triple hemisection TAL does not allow suturing of the tendon; however, this may be desired in conditions involving spasticity to ensure that the tendon is adequately lengthened. Over lengthening is less of a concern since postoperative use of a rigid AFO is likely under these circumstances. Open Achilles Z-lengthening allows direct suturing at the desired tendon length but is less desirable when the local soft tissue is compromised by uncontrolled edema or when adjacent ulceration predispose to cross contamination. Figure 22.6 highlights the effectiveness of soft tissue release in patients with neuromuscular contracture.
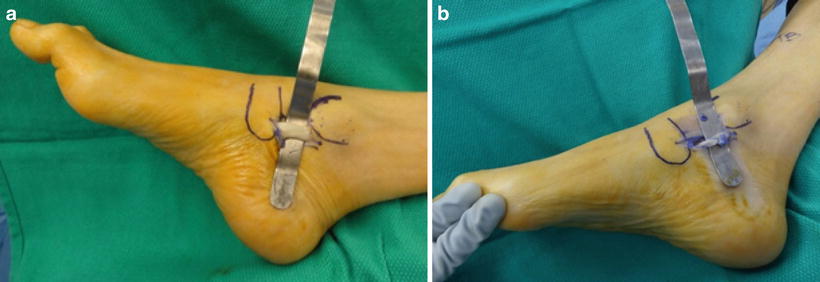
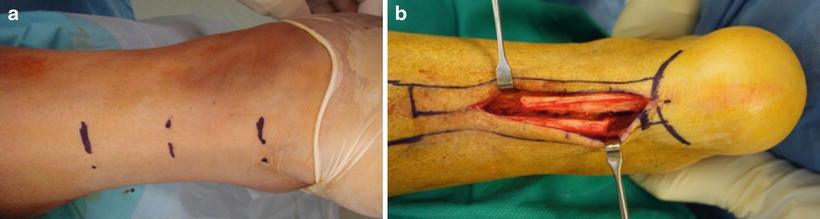

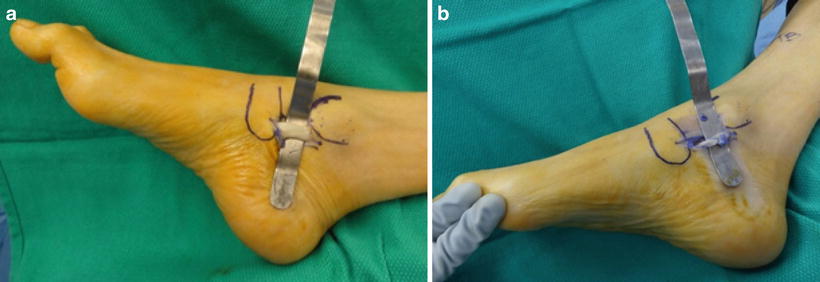
Fig. 22.4
Open Z-lengthening of the posterior tibial tendon to treat inversion contracture deformity. (a) Posterior tibial tendon Z-lengthening or tenotomy was performed through a small open incision extending from the tip of the medial malleolus to the navicular tuberosity. The posterior tibial tendon is fairly subcutaneous at this location, and the incision is safely away from the posterior tibial nerve and artery. Tendon contracture makes for easy palpation of the tendon for incision placement. (b) A sliding Z-lengthening tendon release was performed followed by side-to-side repair
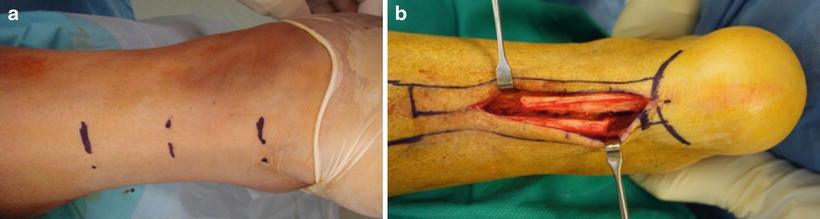
Fig. 22.5
Achilles tendon lengthening to treat ankle equinus. (a) Incisions are shown for minimally invasive triple hemisection Achilles lengthening. (b) Open Achilles Z-lengthening allows more controlled lengthening with direct suturing at the desired tendon length

Fig. 22.6




Soft tissue release of ankle and digital contracture associated with stroke. (a) This foot was partially supple when relaxed but severely plantarflexed and inverted when weight bearing forces stimulated spasticity. This created a dilemma when attempting to brace the limb in the neutral position. (b) Six-week post-op clinical result is shown with the right foot now resting flat on the ground. She regained active ankle dorsiflexion at the ankle and no longer suffered with toe contracture. Intentional weakening of the spastic posterior tibial, Achilles, and flexor tendons allowed fairly normal function of the anterior tibial and extensor tendons which were previously overpowered by posterior contracture. Surgical intervention oftentimes allows ambulation without an AFO which further alleviates pressure on the lateral malleolus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








