Fig. 21.1
Flow diagram for treatment options based on route of calcaneal osteomyelitis and wound status. Calcaneal osteomyelitis is generally caused by one of three routes of infection including hematogenous, direct inoculation from penetrating trauma, or contiguous spread of infection from adjacent ulceration. Treatment options are dependent on multiple variables including the source of the infection, extent of bone involvement, surrounding soft tissue quality and wound deficit, vascular status, and ambulatory status. The flowchart diagrams our five treatment options which are largely based on route of infection and wound status. Despite surgical intervention, medical management with antibiotics is required in the treatment pathways unless the leg is amputated. This protocol assumes that treatment may be escalated if poor clinical response is encountered
Table 21.1
Treatment protocols for calcaneal osteomyelitis
 |
Clinical and Radiographic Workup
A standardized workup for osteomyelitis including probe to bone, vascular status, inflammatory marker labs, and imaging is important for the diagnosis and management of calcaneal osteomyelitis (Fig. 21.2). Radiographic changes generally lag behind the initial development of osteomyelitis by a few weeks. Baseline X-rays early in the course of heel ulceration are helpful for later comparison as anatomy can vary. The opposite heel can also be imaged for comparison as the calcaneus is largely symmetrical in most individuals. A positive probe-to-bone exam or unexplained elevation of inflammatory marker labs raises concern for bone infection at which point advanced imaging or biopsy is helpful to confirm the diagnosis. Advanced imaging such as MRI may have clinical utility even with X-ray changes in an effort to determine the extent of bone infection or involvement of adjacent soft tissues. If the infection extends into the adjacent bones of the rearfoot, limb salvage techniques are likely to fail (Fig. 21.3a). Bone scan and CT are reasonable alternatives for patients unable to undergo MRI. Bone scan is a cost-effective screening method to rule out osteomyelitis, especially in patients with bilateral decubitus heel ulceration (Fig. 21.3b).
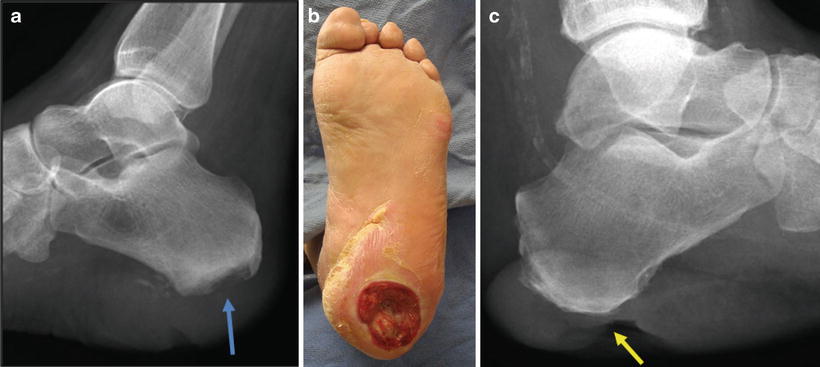
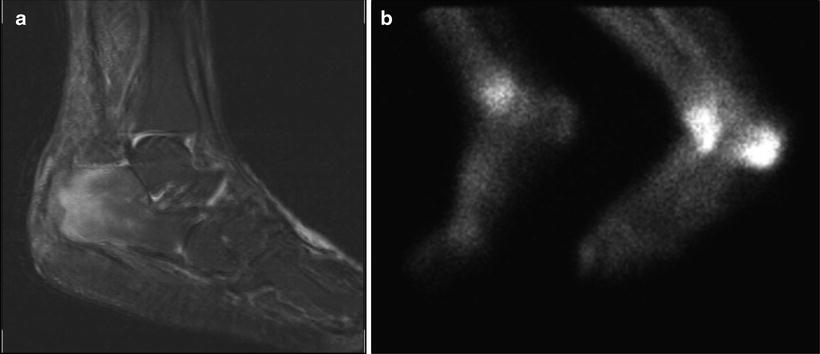
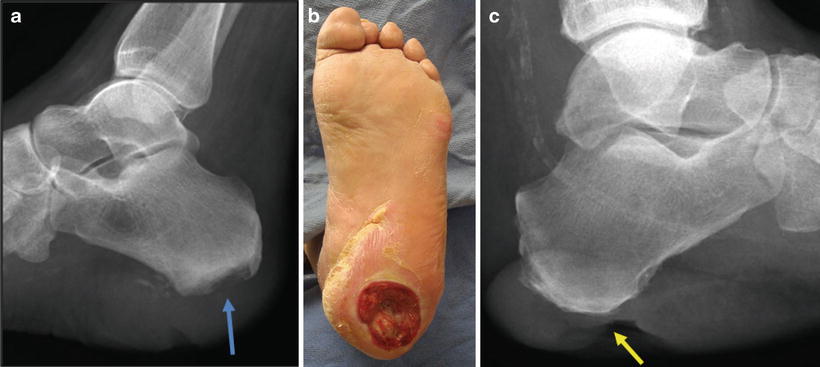
Fig. 21.2
Radiographic evaluation in the workup of calcaneal osteomyelitis. Standard X-rays are the first-line imaging study and should not be skipped for advanced imaging. Our heel X-ray protocol includes four views of the heel which includes the lateral, both obliques, and an axial view. Baseline X-rays for slow-healing wounds are useful for comparison months later if infection develops. Alternatively, bilateral comparison views serve a similar purpose. (a) Cortical erosion is typically the first sign of infection as seen here deep to a decubitus ulcer at the apex of the heel (blue arrow). (b) X-ray findings should be correlated with the clinical picture including location and depth of the wound and clinical signs of infection. (c) Note how this large soft tissue defect extends to bone (yellow arrow) yet the calcaneus appears relatively normal
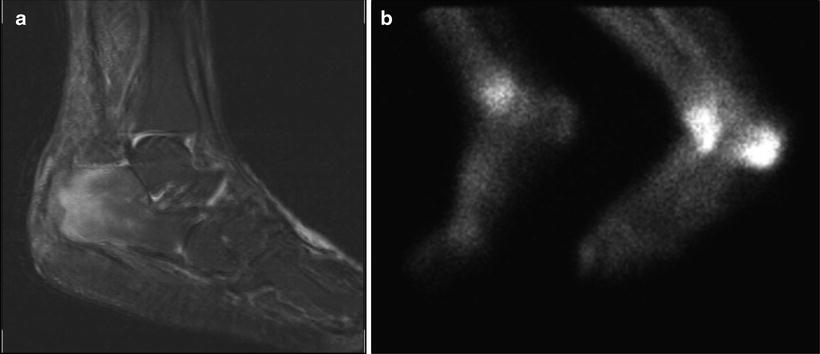
Fig. 21.3
Advanced imaging for diagnosis of calcaneal osteomyelitis and surgical planning. MRI is our go-to advanced imaging modality for calcaneal osteomyelitis. CT and bone scan have clinical utility depending on individual patient circumstances. Advanced imaging can be very sensitive to detect early onset of osteomyelitis but is not entirely diagnostic as false-positive studies are common. Advanced imaging is useful to determine the extent of osteomyelitis; however, bone inflammation as seen on MRI and bone scan can be misleading regarding viability of the involved bone. MRI is useful to evaluate for involvement of the surrounding soft tissues including the plantar arch or proximal leg as well as the subtalar joint, ankle joint, and talus. Infection spreading into these adjacent structures is more likely to be treated with leg amputation as local measures are less effective. (a) Once infected, a large portion of the calcaneus will appear inflamed on MRI. Intraoperative assessment of bone viability is important under these circumstances to determine if bone is dead and abscessed or inflamed yet viable. Bone scan has practical implications for screening, especially in patients with bilateral decubitus wound infection. (b) Bone scan images suggest unilateral osteomyelitis and decrease the need for bilateral MRI. Bone scan is not as useful for anatomic delineation of infection but is very sensitive for early-onset screening
Adequate blood flow for healing of the surgical procedure is necessary especially when considering a local flap for closure purposes. The blood supply to the heel is from two source arteries, the lateral calcaneal branch from the peroneal artery and the medial calcaneal branch from the posterior tibial artery [16]. The success of surgical intervention is related to the patency of these two arteries. Patients with non-reconstructible vascular compromise may not be able to successfully heal after foot surgery, and leg amputation may be more prudent for this patient population.
Isolated Medical Management
Medical management of calcaneal osteomyelitis without surgical intervention is feasible under certain circumstances, particularly in hematogenous osteomyelitis which is covered in Chap. 7. Bone biopsy is ideal but not always necessary for patients undergoing medical management which allows culture-specific antibiotic treatment. The trephine or needle bone biopsy technique can be performed as a sterile bedside procedure under local anesthesia, especially in patients with neuropathy. Bone biopsy techniques are covered in Chap. 4. Calcaneal osteomyelitis associated with infected decubitus ulcers, open trauma, and postoperative infections is frequently not amenable to isolated medical management due to wound infection, soft tissue defect, exposed bone, necrotic bone, and soft tissue abscess.
Cortical Window with Internal Medullary Bone Debridement
Cortical window and medullary bone debridement allows internal medullary debridement of infection with preservation of the structure and function of the calcaneus by preserving the cortical shell which is largely uninvolved in osteomyelitis caused by direct inoculation or hematogenous source. MRI is useful to determine the extent of bone abscess or necrosis; however, it is important to note that inflammation of the medullary bone on MRI does not necessarily indicate dead bone. Infected bone can be preserved as long as it remains viable which is best determined on direct operative inspection. This conservative surgical approach allows decompression of sequestered infection and procurement of tissue for bone biopsy through a small incision.
Patient Selection
Calcaneal osteomyelitis associated with penetrating injuries or hematogenous spread frequently involves medullary bone infection without significant infection of the surrounding soft tissues or cortical bone. Puncture wounds to the heel may violate the cortical bone with implantation of bacteria directly into the medulla of the calcaneus due to the high-impact nature of stepping on a nail [17]. The puncture wound may heal uneventfully while the infection festers deep within the calcaneus with late presentation similar to hematogenous osteomyelitis. Although rare, there is also a potential to develop calcaneal osteomyelitis after injection for plantar fasciitis, and case studies have been described in the literature [18, 19].
Surgical Technique
Typically there is minimal or no wound defect present which allows for ellipse of the small wound or linear incision for exposure to the infected bone as demonstrated in case 1 (Figs. 21.4, 21.5, and 21.6). A medium-sized trephine is used to core out the involved bone or open the cortex (Fig. 21.7). A curette can then be inserted into the canal with the goal to curette to healthy, bleeding bone and procure specimen for biopsy. This technique can be performed in a staged-type manor with the initial surgery involving incision and drainage, bone debridement, placement of antibiotic beads, and wound closure. The stage 2 procedure allows bead removal, repeat debridement, clean margin bone biopsy, and final wound closure (Fig. 21.8a).




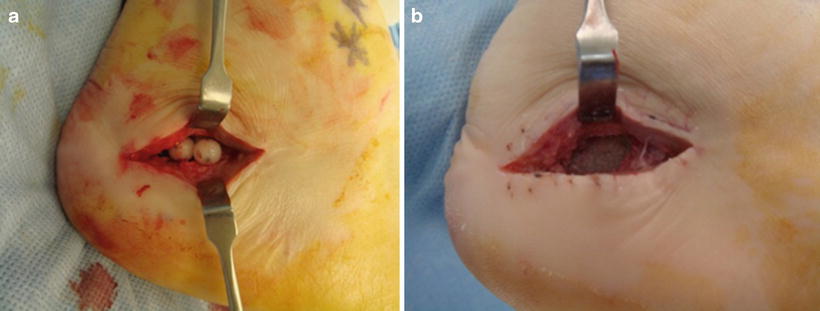

Fig. 21.4
Patient selection for cortical window with internal medullary debridement technique is shown in case 1. This minimally invasive approach is considered in patients with small wounds and localized bone infection associated with penetrating injuries or hematogenous spread of infection. Note the small but penetrating heel wound which probed to bone raising concern for osteomyelitis

Fig. 21.5
X-ray changes correlate with the location of the small heel wound in case 1. Preoperative radiographs demonstrated lucency and mottling of the posterior aspect of the calcaneal tuberosity which is highly suspicious for osteomyelitis. Elevated ESR and CRP were also consistent with osteomyelitis. MRI followed by bone biopsy and medullary debridement through a cortical window was the next logical step

Fig. 21.6
Incision approach in case 1 for biopsy technique through the wound. A 3:1 ellipse of the small wound allowed access for bone debridement and excision of the sinus tract. A linear or oblique incision may be used if there is no soft tissue defect. The incision is kept off of the weight bearing surface and away from the Achilles tendon, sural nerve, and vascular structures where possible. Layered dissection is not necessary or desired since the incision is small and there are no vital structures on the medial, lateral, or plantar aspects of the posterior tuberosity of the heel

Fig. 21.7
Case 1: Bone debridement and biopsy preferred technique. (a) Bone biopsy was obtained with the use of a medium-sized trephine to open the cortex and core out the involved bone and sinus tract. (b) This provides bone specimen for biopsy. (c) A narrow curette is then passed into the medullary canal allowing debridement to viable, healthy bone as shown in a different patient who developed hardware-related osteomyelitis. Intra-op imaging is used to confirm the location and monitor extent of bone debridement
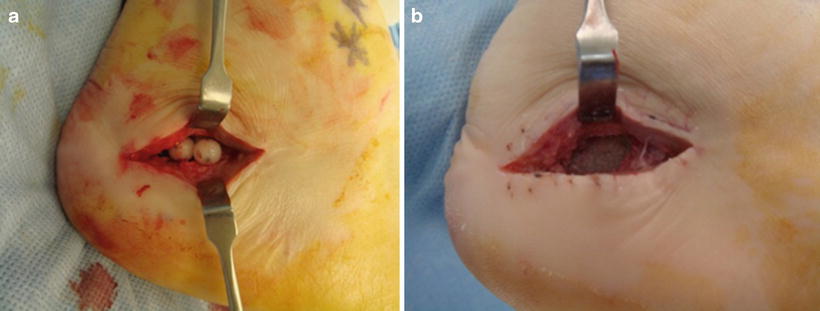
Fig. 21.8
What to do with the bone deficit? (a) Staged surgery in case 1 allows insertion of an antibiotic-impregnated cement bead chain and temporary closure of the wound which provides high local levels of antibiotics and serves as a void filler if future bone grafting is planned. Bead removal is performed approximately 2 weeks later which allows repeat biopsy. The same incision can be used for multiple debridement procedures. A dilemma remains regarding the best option for filling of the void at the time of the definitive procedure. (b) Stage 2 surgery involves removal of antibiotic beads, and clean margin bone biopsy. The defect could be left as is or the defect could be packed antibiotic-impregnated calcium sulfate pellets which are absorbed slowly but can be associated with persistent wound drainage
Bone Grafting of the Defect
Small bone defects can heel secondarily, while large defects may require bone grafting in an effort to minimize the risk of pathologic fracture. Serial negative bone cultures performed during repeat antibiotic bead exchange procedures allow successful bone grafting once culture is negative. Absorbable antibiotic-impregnated calcium sulfate pellets are another option although these are commonly associated with persistent drainage from the surgical wound as the resorbing material is extruded [20–23] (Fig. 21.8).
Postoperative Care
A major benefit of this calcaneus sparing approach is that the Achilles tendon attachment and plantar weight bearing aspect of the heel are not affected. Wound closure is immediate or delayed depending on the clinical situation. The same incision can be used for multiple debridement procedures if a staged approach is needed. Postoperative weight bearing status is determined by the location of the incision and extent of bone debridement. There is risk of pathologic calcaneus fracture from infection or surgical manipulation. It is common to leave stitches in place for up to 6 weeks in the diabetic population if wound healing is delayed (Fig. 21.9). Inflammatory marker labs are monitored to direct the course of antibiotics. Antibiotics are used to treat residual infection as this surgical approach is not intended to be curative in isolation.


Fig. 21.9
Case 1: Postoperative protocol. Postoperative weight bearing status is determined by the location of the incision and extent of bone debridement. Six weeks of non-weight bearing is the norm given the location of the incision and desire to protect the calcaneus against pathologic fracture. (a) Initial postoperative lateral radiograph demonstrating the bone void filler (blue arrow). (b) Initial intraoperative-closed incision. (c) Six weeks postoperative with delayed suture removal and debridement of any dried eschar along the incision
Wound Excision with Cortical Debridement
Excision of a decubitus, traumatic, or surgical wound followed by conservative debridement of the underlying cortical bone allows removal of necrotic tissue, debridement of nonviable cortical bone, procurement of bone tissue for biopsy, and exposure of vascular cancellous bone which promotes granulation tissue to allow progressive wound healing. The overall structure of the calcaneus is preserved to maintain heel function. The insertion of the Achilles tendon is preserved when possible although posterior wounds are frequently compromised by exposure and necrosis of the distal Achilles.
This conservative surgical approach takes into account that the remaining calcaneus is infected but still healthy enough to recover with combined medical and conservative surgical management. Local antibiotic delivery is not very practical with this approach due to lack of dead space to accommodate insertion of antibiotic-impregnated beads.
Patient Selection
Calcaneal osteomyelitis associated with contiguous spread of infection from an adjacent decubitus, surgical, neuropathic, or traumatic wound commonly involves a full-thickness soft tissue defect and necrosis of the exposed periosteum and cortical bone. The internal medullary bone may also be infected but still viable due to the robust internal vascularity of the calcaneus. MRI is useful to determine the extent of infection although the surgeon should be mindful that inflamed bone is not necessarily dead bone. Extensive wounds on the plantar weight bearing surface or necrosis of a broad section of the calcaneus may be more amenable to partial calcanectomy which is discussed later in this chapter.
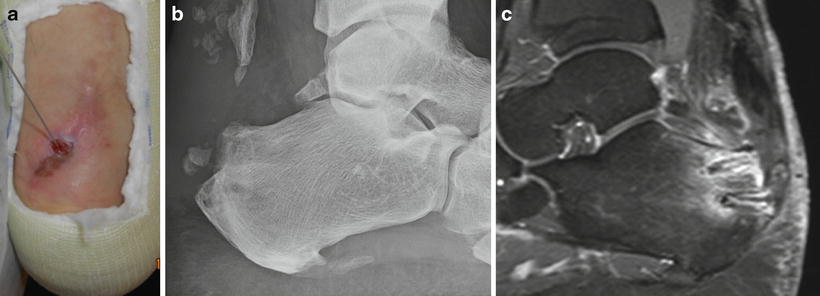
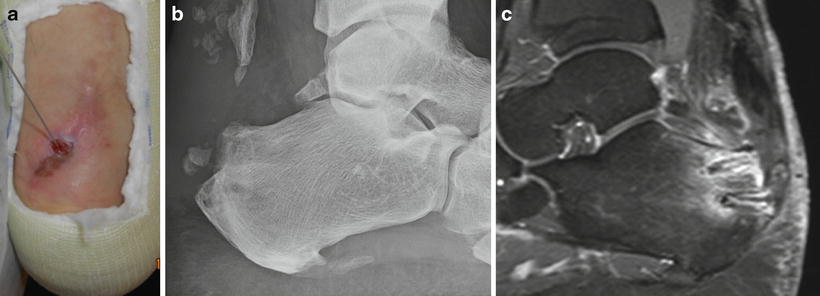
Fig. 21.10
Case 2: nonhealing surgical wound with concern for osteomyelitis. Second-opinion consultation for a nonhealing wound following retrocalcaneal surgery 7 months prior. History of early wound dehiscence with repeat wash out and closure. (a) The wound probed to bone raising suspicion for bone infection. (b) Radiographs were difficult to interpret given recent surgery and extensive calcifications. (c) MRI suggested disease within the Achilles and spread of infection within the calcaneus although false positive is possible with recent tendon and bone surgery. Note anchors present at the site of infection concern. Treatment involved open cortical debridement for removal of infected and prominent bone, removal of residual hardware, bone biopsy, inspection and debridement of the Achilles, and exposure of viable cancellous bone which promotes soft tissue healing
Surgical Technique
Incision placement will vary based on the wound location and extent of soft tissue involvement. Wound closure may or may not be possible, but 3:1 ellipse of the wound is common, and linear extension may be necessary for adequate exposure. The bed of the wound is often nonviable in patients with osteomyelitis, and wound excision down to bone is the norm. Hardware from previous surgery is removed, assuming the fracture or previous surgical intervention is stable and conversion to external fixation may be necessary. A wide section of cortical bone is encountered with this approach, allowing direct inspection for signs of bone necrosis, abscess, erosion, etc. A rongeur or other bone cutting instrument is used to remove the outer shell of cortical bone, exposing the underlying cancellous bone and procuring bone for biopsy. The intent of bone debridement is to remove the nidus of infection yet preserve a functional calcaneus if possible. The bone is reshaped to minimize the risk of recurrent tissue breakdown. A necrotic Achilles insertion is common with posterior wounds, and salvage of the tendon may not be possible. Normal-appearing, bleeding, viable bone is preserved regardless of what looks abnormal on MRI. Serial debridement every few days or weeks may be necessary to achieve a healthy margin without excessive resection.
Wound Closure Options
Primary wound closure is typically not possible for large ulcers yet prolonged exposure of cancellous bone beyond the course of antibiotic therapy is not likely to be successful. Negative-pressure wound therapy is a common approach to promote formation of granulation tissue over the freshly debrided bone surface which can be covered with a skin graft once the wound granulates to the surface. Local rotational flaps provide better tissue durability on the heel but have limited utility without wide bone resection as in partial calcanectomy. Advanced plastic surgical techniques are possible including a reverse sural artery flap or transpositional muscle flap followed by skin grafting [24–29]. These are fairly invasive options but may be considered depending on the size and location of the wound defect as the sural artery flap or skin graft to the plantar heel may not withstand the stress of walking.
Postoperative Care
Prolonged wound care with an extended period of non-weight bearing may be needed with this approach as complete resolution of the wound may take months. A rigid ankle-foot orthosis (AFO) will be needed in cases where the Achilles tendon cannot be preserved. Delayed flexor hallucis longus tendon (FHL) transfer is an option for selected patients including postoperative calcaneal osteomyelitis secondary to insertional Achilles tendon surgery. Resolution of infection is warranted prior to performing FHL tendon transfer. The surgeon may consider performing repeat bone biopsy prior to undergoing reconstructive tendon surgery.
Case Examples of Wound Excision with Cortical Debridement
Three case examples are shown to demonstrate patient selection criteria, surgical technique, and aftercare. Case 2 involved calcaneal osteomyelitis after repair of an insertional Achilles tendon rupture that developed wound dehiscence postoperatively. The patient underwent wound excision, removal of soft tissue anchors, near-total resection of the Achilles tendon insertion, bone resection and biopsy, and primary wound closure (Figs. 21.10, 21.11, and 21.12). Case 3 involved calcaneal osteomyelitis associated with open reduction and internal fixation of a calcaneal fracture. Treatment consisted of raising the lateral flap, removal of hardware, debridement of cortical bone, bone biopsy, and primary wound closure (Figs. 21.13, 21.14, 21.15, and 21.16). Case 4 involved a decubitus Achilles tendon wound that developed calcaneal osteomyelitis. Treatment involved wide resection of the necrotic Achilles followed by cortical debridement and partial wound closure (Figs. 21.17, 21.18, 21.19, 21.20, 21.21, and 21.22). Bone biopsy-directed postoperative antibiotics were used in each case.

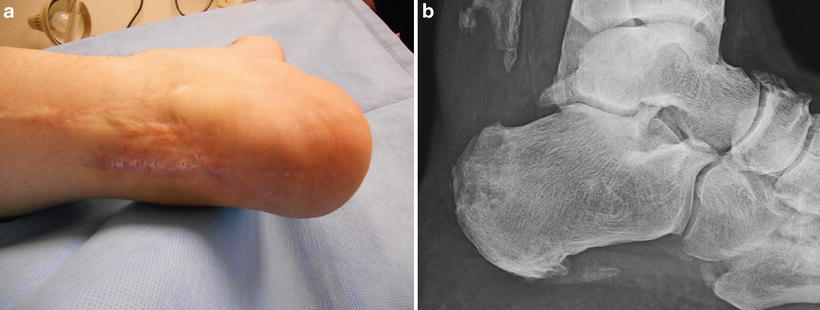
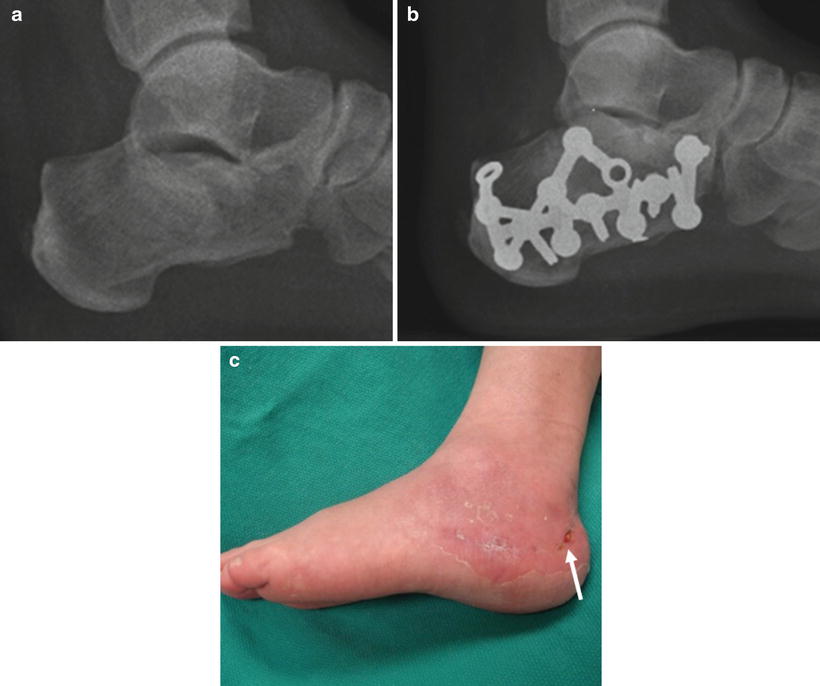

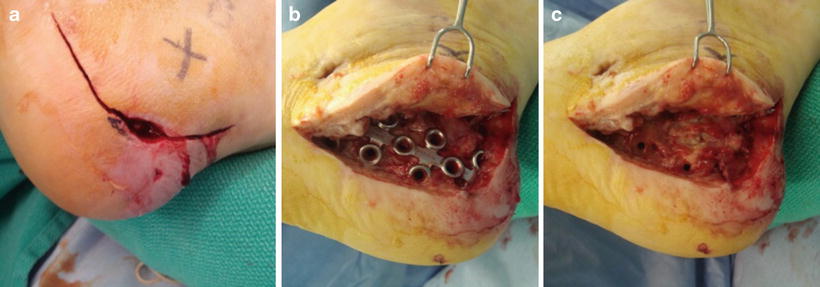

Fig. 21.11
Case 2: initial postoperative lateral radiograph. Intraoperative findings included infection coursing along the bone anchors, and the central portion of Achilles tendon was necrotic. The anchors were removed followed by curettage to debride the anchor holes and procure bone biopsy. The posterior heel was remodeled as shown with the intent to preserve the tuberosity knowing that medical treatment would follow. Only the medial and lateralmost slips of the Achilles tendon remained attached. Bone biopsy revealed chronic osteomyelitis
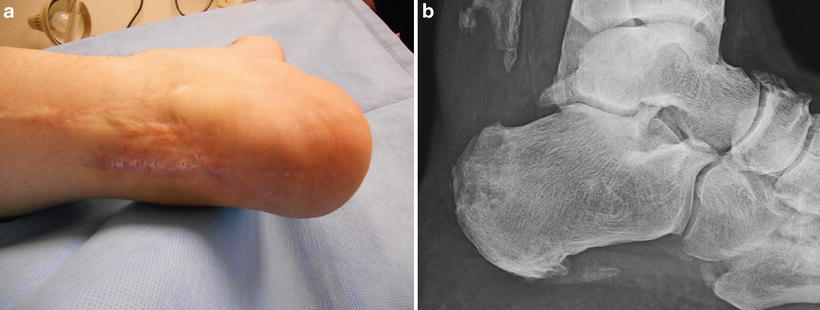
Fig. 21.12
Case 2: postoperative course. Clinical photos at 4 months post-op (a) demonstrate complete healing of the incision. Lateral radiograph (b) demonstrates no progressive destruction 4 months later. No residual weakness, gait changes, or concern for infection was noted at 11-month follow-up
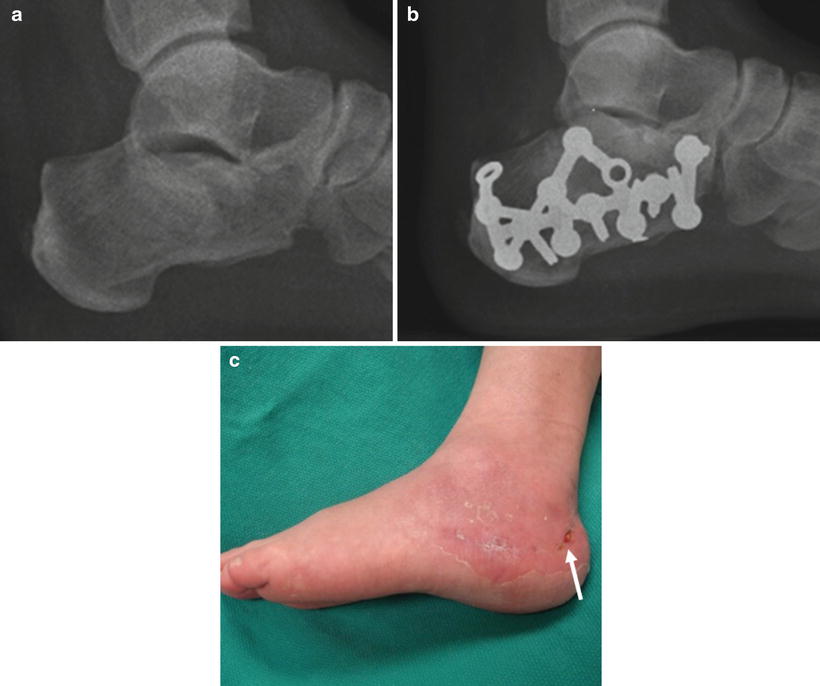
Fig. 21.13
Case 3: infected sinus tract, exposed hardware, and concern for osteomyelitis following calcaneal fracture open repair. (a) Preoperative lateral radiograph demonstrates a joint depression intra-articular calcaneal fracture. (b) ORIF involved extensile lateral exposure with plate fixation which was delayed for 3 weeks secondary to swelling. (c) The tip of the flap failed to heal leading to postoperative infection several months after surgery (arrow). Exposed hardware and concern for osteomyelitis was treated with removal of hardware, bone biopsy, cortical bone debridement, and primary closure of the wound

Fig. 21.14
Case 3: bone biopsy considerations. Bone biopsy was initially obtained through a separate incision away from the open wound to minimize the risk of cross contamination. See Chap. 4 for further details on bone biopsy techniques
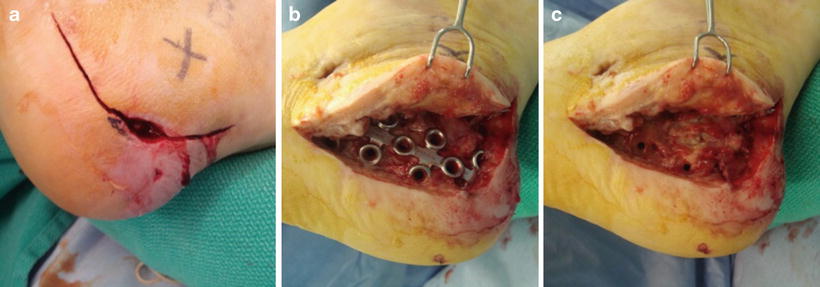
Fig. 21.15




Case 3: hardware removal and cortical debridement. The original flap was raised to allow access for hardware removal and closure of the chronic wound. (a) The incision was made full thickness to bone with care to stay perpendicular to the skin edges. (b) The flap was raised full thickness with a limited-touch technique. (c) Hardware from previous surgery was removed, as the fracture was healed. The lateral cortex was widely exposed for debridement and biopsy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








