Fig. 14.1
Acute Charcot arthropathy. Note severe swelling and erythema which is difficult to differentiate from acute infection
1.
Isolated Charcot arthropathy
2.
Charcot arthropathy with noninfected ulceration
3.
Charcot arthropathy with soft tissue infection
4.
Charcot arthropathy with osteomyelitis
The differential diagnosis in the presence of unilateral edema, erythema, and increased temperature includes cellulitis or other soft tissue infection, thrombophlebitis, or acute arthropathy such as gouty arthritis. Additionally, stress fractures or insufficiency fractures may also present with the same clinical symptoms. This is usually secondary to diabetes-associated bone disease with continued ambulation on the fracture due to the inability of the patient to perceive the fracture especially in the presence of sensory neuropathy. It has been suggested that the unperceived bony injury may represent an initial inciting factor for the development of Charcot arthropathy [1].
Charcot arthropathy often leads to boney prominence associated with destruction and collapse along the medial or lateral borders of the foot or through the ankle. This prominence can lead to local ulceration which compromises the skin envelope and creates an environment for soft tissue infection (Fig. 14.2). The adjacent bone eventually becomes exposed to organisms and osteomyelitis is a common sequella. The Charcot deformity and resultant boney prominence that created the ulceration will have to be dealt with along with the infection. This can be done as a staged procedure or as a single-stage reconstruction. Osteomyelitis through a hematogenous route can also occur in patients with both the acute and chronic Charcot arthropathy [2]. Osteomyelitis can also be the cause of the Charcot arthropathy due to weakening of the bone structure [2, 3].


Fig. 14.2
Ulceration of medial aspect of the foot secondary to deformity associated with midfoot Charcot arthropathy
Clinical Evaluation
As with most clinical disorders, evaluation of a patient with Charcot arthropathy and potential infection involves a careful history, clinical examination, the judicial utilization of laboratory studies, and bone and joint imaging studies.
In a patient with Eichenholtz stage 0 or stage I Charcot joint deformity, the patient may recall unilateral swelling preceding the development of an open wound. Under such circumstances, the edema may be complicated by other causes of swelling, such as venous insufficiency, lymphedema, or neuropathic edema commonly encountered in the patient with diabetic autonomic neuropathy. Lower extremity edema may result in pressure against shoes or the supporting surface, following which the ulceration noted was subsequent to the edema.
The patient with chronic Charcot arthropathy manifesting as Eichenholtz stage II or stage III deformity may recall initial swelling and deformity of the foot, following which an ulceration of the skin envelope occurred. Charcot arthropathy is not associated with a history of fever, chills, or systemic inflammatory response to sepsis. In those circumstances in which the patient recalls the ulceration preceding swelling, redness, and warmth, a consideration that the manifestations noted represent an infectious process is raised. It should be noted that local infection including osteomyelitis in a patient with diabetes can occur absent systemic signs or symptoms of sepsis. Although pain may be present in a patient with Charcot arthropathy, the deformity is typically painless. Significant pain is usually present with local sepsis.
There is an association of ulceration and infection including osteomyelitis in the Charcot foot, but the relationship is not well defined in the literature. Ulceration in the Charcot foot typically occurs adjacent to prominent and palpable osseous structures such as the cuboid, fifth metatarsal base, or below the first metatarsal-cuneiform joint. There is no specific data available evaluating the incidence of osteomyelitis in a patient with diabetic ulceration associated with Charcot arthropathy. Generally, references are sited which examine the incidence of osteomyelitis association with diabetic ulceration. Studies have demonstrated that greater than 50 % of chronic diabetic ulcerations are infected, and of those ulcerations, 20–60 % of infected ulcerations can be demonstrated as having an underlying osteitis or osteomyelitis. Ulcerations of longer duration are more likely to be associated with underlying osteitis or osteomyelitis. It has also been generally reported that ulcerations greater than 2.0–4.5 cm2, and deeper than 3 mm, are more likely to be associated with underlying osteitis or osteomyelitis [4–7].
The presence of exposed bone at the base of an ulceration in a patient with Charcot arthropathy increases the likelihood of associated osteitis or osteomyelitis. When not directly visible within the ulceration itself, probing of the ulcer with a metallic probe is frequently employed in order to determine the likelihood of osteomyelitis (Fig. 14.3). This maneuver is commonly referred to as the “probe to bone test.” There are no specific studies on the utilization of the probe to bone test for the diagnosis of osteomyelitis in ulcers associated with Charcot arthropathy. Reported rates of sensitivity of the probe to bone test ranged from 38 to 94 % and specificity 85 %–98 % [8–13]. A positive probe to bone test is most valuable when placed in proper clinical context; in many patients contamination of the outer portion of the bone, osteitis rather than osteomyelitis is present. Given the presence of either a positive probe to bone test or radiographs suggestive of osteomyelitis, one study demonstrated that 72.4 % of patients demonstrated histologically proven osteomyelitis, of which 82.5 % demonstrated a positive bone culture [11]. In general, osteomyelitis may be diagnosed with confidence when the probe to bone test is positive in a patient whose clinical presentation is consistent with osteomyelitis or when the radiographs are consistent with osteomyelitis.
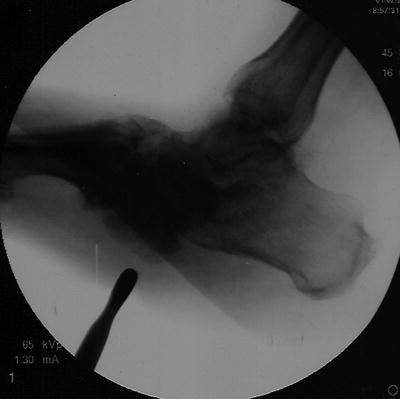
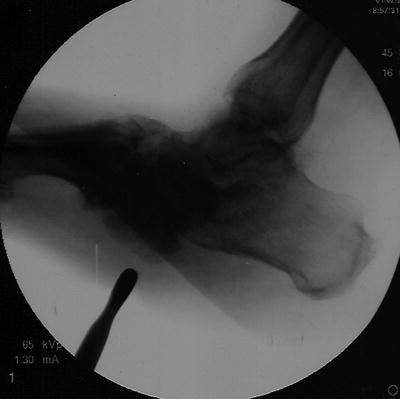
Fig. 14.3
Probe to bone test. Note that the wound is located directly over the prominent midfoot bone associated with Charcot arthropathy
Laboratory Evaluation
Although characterized by clinical evidence of inflammatory changes such as redness, swelling, and warmth, laboratory studies with Charcot arthropathy are generally not reflective of a systemic response to infection or other inflammatory process. Markers for inflammation such as elevated procalcitonin, elevated erythrocyte sedimentation rate (ESR), elevated C. reactive protein (CRP), and presence of a leukocytosis are not present and, when present, should raise the concern for underlying infection. The utilization of procalcitonin to determine the presence of osteomyelitis in patients with infected diabetic foot ulcers has been examined. Elevation in procalcitonin levels was noted in patients both with osteomyelitis (66.7 pg/mg) and without osteomyelitis (58.6 pg/mL) [14]. In general, erythrocyte sedimentation rates and elevation in WBC are significantly higher in the presence of osteomyelitis. C. reactive protein has not been demonstrated to be of significant assistance in the differentiation of soft tissue versus bone infection in a patient with diabetic foot ulceration. However, posttreatment persistent elevation of CRP is associated with increased risk of amputation [15].
Bone Biopsy
Bone biopsy and histology have long been considered the “gold standard” for the diagnosis of osteomyelitis associated with diabetic ulceration. Bone histology along with bone culture is also used for the discrimination of Charcot arthropathy from osteomyelitis. The areas that should be biopsied are based on radiologic examination: MRI, CT scan, and X-ray, as well as intraoperative clinical findings. Multiple areas of the bone in question should be biopsied and labeled by their anatomic orientation. Possible contamination of the specimens obtained and difficulty in histologic discrimination of osteomyelitis from Charcot arthropathy with the associated bony changes require careful interpretation of bone histology and bone culture reports. In one study, pathologists blinded to the source of specimens obtained from diabetic patients and asked to diagnose either osteomyelitis or no osteomyelitis were in complete agreement in only 33.33 % of cases and were in disagreement as to the presence or absence of osteomyelitis in 41.03 % of cases [16]. Another study found that the results of specimens divided and sent for culture and histology demonstrated that a positive culture and a negative histology are just as likely to occur as are a positive histology and a negative culture. The study further concluded that microbiologic testing is equivalent to histologic testing for the diagnosis of osteomyelitis associated with diabetic ulceration [17]. The usefulness of obtaining both a bone culture and histology is reflected by a study demonstrating that culture demonstrates a 42 % sensitivity for the diagnosis of osteomyelitis, whereas the combination of culture and histology is associated with 84 % sensitivity with a diagnosis of osteomyelitis [18]. Biopsy of the bone directly under an ulceration by approaching the bone directly through the wound itself has been reported [19]. Although the potential for contamination exists with this approach, successful resolution of underlying osteomyelitis, present in 96 % of bone cultures obtained through the wound, was reported utilizing treatment based upon the wound culture. Cultures obtained directly from exposed bone for the treatment of osteomyelitis has been examined, although not specifically for ulceration in diabetic ulceration associated with Charcot arthropathy. Bone contact swabs were compared with bone biopsy in one study, demonstrating 82.35 % agreement with swabbing of the exposed bone and true bone biopsy. Swabbing of the exposed bone was 96 % sensitive for the causative pathogen, with a 79 % specificity and a positive predictive value of 92 % [20]. Evaluation of osteomyelitis by culturing through a sinus tract has also been examined. In one study, two different cultures were obtained from a sinus tract taken at different times. The concordance of the sinus tract cultures with true bone cultures was reported as 96 %, with a sensitivity of 91 % and a specificity of 86 %. Accuracy of sinus tract cultures was reported as 90 %, particularly when the infection was monomicrobial in etiology [21]. The techniques of needle biopsy versus transcutaneous biopsy for the diagnosis of osteomyelitis have also been examined. Needle biopsy has been demonstrated to be associated with a 16.1 % false-positive and 38.1 % false-negative rates. Overall, bone biopsies have been reported as associated with a 67.7 % recovery rate, bone needle biopsy 58 % recovery rate, and bone swabs 96.7 % recovery rate [22].
Circumstances have been proposed in which biopsy should be considered [23]. These circumstances include concern for the presence of a drug-resistant organism, the presence of continuing bone destruction or elevated markers of inflammation in the presence of ongoing antibiotic therapy, in circumstances where a definitive diagnosis is required, and finally in those circumstances wherein there is a plan for the utilization of internal or external fixation secured within a bone which is potentially infected.
Bone cultures and histological specimens are frequently obtained from patients who have received prior antibiotic therapy for presumed soft tissue or bone infection. Ideally, bone cultures are obtained when the patient is either antibiotic naïve or has not received antibiotics for at least 2 weeks. Discontinuation of antibiotics for 48 h has been associated with acceptable bone cultures [24].
All techniques of bone culture and histology are associated with both false-positive and false-negative results. The practitioner faced with the possibility of Charcot arthropathy with associated soft tissue or bone infection should consider the results of testing in a clinical scenario as “likely associated with osteomyelitis” versus “not likely to be associated with osteomyelitis.”
In summary, bone cultures and histology are associated with a significant incidence of false-positive and false-negative results. Studies available for the evaluation of bone cultures and histology associated with diabetic ulceration are not studies specifically entered for the treatment of possible osteomyelitis in the patient with Charcot arthropathy. All such studies must be interpreted carefully in the patient with Charcot arthropathy. This is of particular concern given the fact that many diabetic ulcerations, unlike the patient with Charcot arthropathy, do not present with significant signs of inflammation such as erythema, warmth, and acute edema.
Bone and Joint Imaging
Charcot arthropathy, particularly during its acute phase, is characterized by variable presentation of osteopenia, joint effusion, the presence of bone debris, as well as erosive and destructive bone changes on X-ray. At times, the distribution of such changes particularly when limited to Lisfranc joint, or the midtarsal joint, strongly suggests the presence of Charcot arthropathy to the experienced clinician. However, the radiographic changes, which characterize Charcot arthropathy, may also be demonstrated in a patient with osteomyelitis. Given the presence of an open wound, particularly with exposed bone, in a warm and swollen foot in the patient with diabetes, the presence of disruptive or resorptive bone changes is concerning. The differential diagnosis of such changes includes Charcot arthropathy, osteomyelitis, inflammatory arthritis, or reactive bone changes secondary to adjacent soft tissue inflammation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








