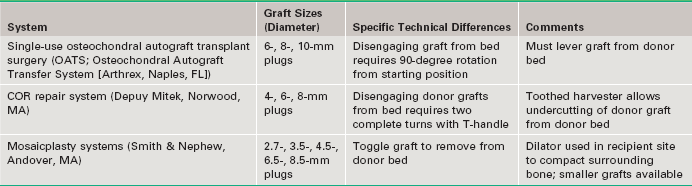
Chapter 67 Defects of articular cartilage are a relatively common problem encountered by the sports medicine physician. Isolated cartilage defects can occur secondary to acute trauma or can be atraumatic in nature. The latter often occur in the form of osteochondritis dissecans, the cause of which is not fully understood, and can be found in juveniles and in adults. The distinction is important, because patients with open physes have a much better prognosis with nonoperative treatment.1 Patients with symptomatic focal cartilage defects are candidates for operative treatment to relieve symptoms and also to potentially prevent subsequent arthritic changes.2 Surgical treatment options include arthroscopic debridement, microfracture, autologous chondrocyte implantation (ACI), matrix-induced chondrocyte transplantation, osteochondral autograft transplant surgery (OATS), and osteochondral allograft transplantation. OATS may be the best option in appropriately selected patients. There are several different transplant systems available, but the concept remains the same: the transplantation of full-thickness osteochondral bone plugs from an area of the knee that is non–weight-bearing or has low contact pressures to the osteochondral defect of the ipsilateral knee. Typical Physical Examination Findings • Standard anteroposterior (AP) and lateral knee views. • Sunrise patellofemoral view to visualize patellar and trochlear lesions. • Notch view may be best to visualize lateral aspect of medial femoral condyle (typical location of osteochondral defects [OCDs]).3 • A mechanical axis view is obtained if malaligment is suspected. • MRI is necessary to best evaluate location and size of articular cartilage lesions. MRI is also important for evaluation of menisci, ligaments, and remainder of articular cartilage. • Bone scans, computed tomography, and tomograms are not as useful as MRI for evaluation of OCDs and the remainder of the knee. • Contrast arthrography (intra-articular or intravenous) may prove to be more sensitive than MRI alone, which can have a high false-negative rate.4 • Arthroscopy remains the gold standard for evaluation of articular cartilage lesions. We prefer to perform single-plug autograft transplants on defects 1 cm2 in diameter or smaller, with allograft transplants used for larger defects. However, some authors perform autograft transplants on defects as large as 4 cm2, with good results5 with use of multiple plugs of varying size (aka “mosaicplasty”). Three different systems are commercially available in the United States. All three are very similar and differ in the available graft sizes and minor variations of technique. A comparison is shown in Table 67-1. An example of the necessary equipment is shown in Figure 67-1.
Osteochondral Autograft for Cartilage Lesions of the Knee
Preoperative Considerations
Physical Examination
Imaging
Additional Imaging
Indications
Expanded Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Osteochondral Autograft for Cartilage Lesions of the Knee