Chapter 30 Orthotic management of the neuropathic and/or dysvascular patient
Peripheral neuropathy
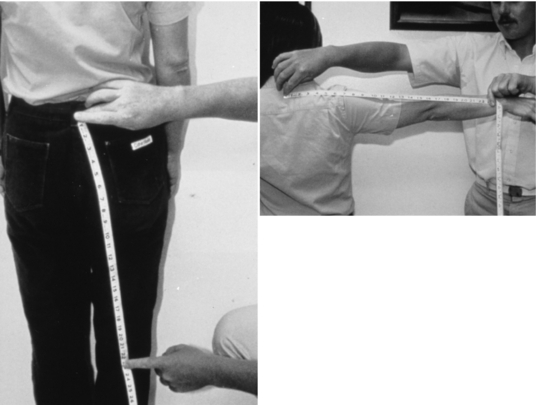
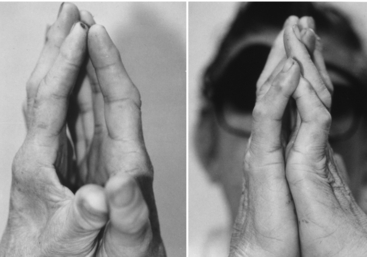
The loss of sensation in peripheral neuropathy is symmetrical and equidistant from the spine in both arms and legs (Fig. 30-1). Therefore, the hands should be evaluated for neuropathy as well as the feet. Little attention has been paid to the “diabetic hand syndrome” in which the joints of the fingers and wrists exhibit limited joint mobility. This condition occurs in 30% to 50% of people who have had type 1 diabetes for more than 15 years. One sign of severe limited joint mobility is the inability to place pronated hands flat on a table or to touch the palms together in the prayer position (Fig. 30-2). The skin is thick and cannot be “tented” on the back of the fingers.24 Thenar atrophy and clawing of the fingers may be present. Hand deficits affect functions such as the ability to don and doff an orthosis and footwear.4
Bilateral testing for sensation is especially important for both the unilateral and bilateral amputee in order to map areas of insensitivity and to follow their progression. Neuropathy may affect a single nerve (mononeuropathy) due to nerve trauma or entrapment, but in most chronic diseases it presents as a polyneuropathy with uncomfortable paresthesias such as prickling, tingling, burning, and jabbing sensations.44,47
The most common disease processes resulting in peripheral neuropathy are as follows:
The following substances and conditions can also cause peripheral neuropathy 8,9,27:
A high index of suspicion for neuropathy is useful when examining the feet of individuals with these conditions. Diabetes mellitus is the leading cause of peripheral neuropathy in the United States, with 54,000 amputations of the lower limb occurring yearly in a population of 14 million diabetics at an annual cost of $14 billion.3,21,32,35,37,48
Complaints of numbness, tingling, or burning night pain are common with neuropathy. The degree of sensory loss is difficult to quantify, but it is important to use an objective method of evaluation for initial detection as well as follow-up. Patients who are unable to detect a Semmes-Weinstein monofilament of 5.07 diameter (10g of force) pressed against their skin have loss of protective sensation and are at risk for foot injury without protective shoes and inserts. It is important to closely inspect the insensate foot, looking and feeling for areas of callused or atrophic skin vulnerable to breakdown, especially on weight-bearing surfaces. In addition, one should check for bony prominences related to claw toes, bunions, or Charcot fracture malalignment. Signs of concomitant dysvascularity, such as pulselessness, decreased hair growth, decreased skin temperature, or gangrene, indicate a high risk of eventual amputation if remedial steps are not taken.
Pressure on the skin can lead to ulceration and destruction of tissue in the neuropathic limb:
Infection abets the spread of tissue destruction. Once the skin is broken, bacterial invasion may cause the surrounding skin to become more vulnerable to even slight pressure, rendering it unsuitable for weight bearing.11
Recurrent ulceration is common over bony prominences, especially in weight-bearing skin. A newly healed ulcer is covered by thin, scarred skin that is likely to tear with stress. Skin adherent to bone has poor shock- and shear-absorbing qualities, making it vulnerable to breakdown. Protection of such skin areas is possible with careful shoe and insert construction.10,12
Charcot neuroarthropathy (Charcot joint)
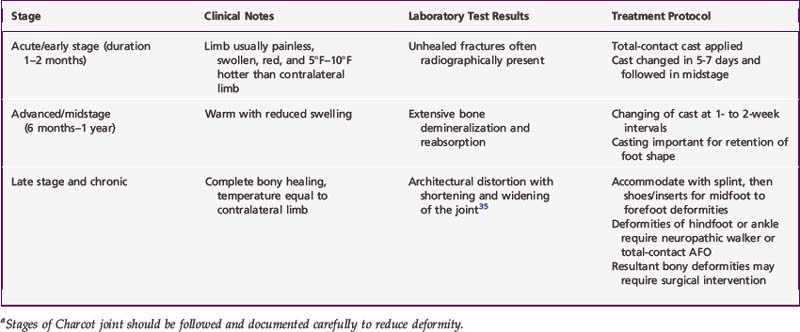
Whatever the cause(s), Charcot neuroarthropathy can lead to radical changes in the shape and stability of affected joints. Its clinical stages, outlined in Table 30-1, should be followed and documented carefully, with management at each stage designed to minimize deformity. Treatment consists of casting in the neutral position for several months, followed by an orthosis such as a neuropathic walker, also known as a Charcot restraint orthotic walker. When the process becomes quiescent, the foot should be protected with appropriate shoes and inserts. If it does not become quiescent or recurs, a permanent ankle–foot orthosis (AFO) may be required.
Examination
The neuropathic limb with intact skin requires careful physical examination to identify deformities that may lead to ulceration in the future. Shoes and socks are removed from both feet at every visit to allow full visualization of calluses, bony prominences, and areas of skin inflammation or breakdown. Thickening of the skin (callus) is a response to increased local pressure or friction (shear).14,45 Skin dryness is the result of autonomic neuropathy, in which sweat and oil production are decreased. Loss of hair growth may be indicative of vascular impairment. Motor neuropathy and Charcot neuroarthropathy often leave the foot deformed.
Joint stiffness increases the risk of ulceration by decreasing normal motion of foot joints during gait, thereby increasing foot–shoe contact pressures. It is important that the ankle have a dorsiflexion range of at least 10 degrees to allow ambulation without harm to midfoot joints or the great toe.38 When the heel rises, the forces on the plantar surface of the metatarsal heads and toes can peak to 80% of body weight when walking and 275% when running. With limited motion in the metatarsophalangeal (MTP) joints, these forces can result in ulceration.4,41,44
Toe deformities
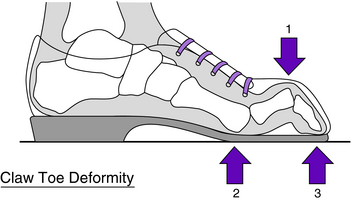
Toe deformities can lead to ulceration by contact with shoe surfaces or adjacent toes. Clawed toes are dorsiflexed at the MTP joints and plantarflexed at the interphalangeal (IP) joints. Excessive pressure occurs where the shoe makes contact with the metatarsal heads and toes (Fig. 30-3). Soft corns are hyperkeratotic lesions caused by pressure on the skin of tightly apposed toes in a moist environment.14 These can be relieved with tube foam placed over the adjacent toes or lamb’s wool between the toes (Fig. 30-4). Hypertrophy of nails caused by fungus (onychomycosis) is common in the diabetic population. These nails tear shoe linings, creating rough surfaces that may abrade the toes.
Complications of the neuropathic foot
Dermatological conditions can affect the insensate limb. Necrobiosis lipoidica diabeticorum can be confused with venous stasis disease but does not require or respond to the extensive treatment required of the latter condition. The round, firm plaques of necrobiosis, which later ulcerate, are reddish brown to yellow and are seen three times more often in women than men.34,49 They are common along the tibia and require only protective dressings until the ulcers heal. Plantar keratoderma is an excessive buildup of keratin following the loss of sweat and oil production in the skin associated with autonomic neuropathy. As a result, the entire margin of the heel pad undergoes diffuse thickening, followed by fissures that allow entrance of bacteria and subsequent infection (Fig. 30-5). Prevention includes reduction of keratin buildup by debridement and retention of skin moisture with the use of various creams.14 Pseudomonas is a bacterium that produces a green pigment within a moist environment. Colonization of the skin by this bacterium is treated by exposing the limb to air. It is important to remember that more dermatological conditions in neuropathic diabetics are discovered by inspection than by patients’ complaints of discomfort.49
Sensation
To assess the risk of ulceration in a neuropathic limb, the level of sensation must be determined. Because sensory loss can have a gradual, almost unnoticed onset, patient history can be misleading. Repeated quantitative measurements of sensation over time help assess progression of sensory impairment. Calibrated Semmes-Weinstein monofilaments, mounted on Lucite rods, provide a simple, quantitative method to determine sensory loss.36 This is a single-point perception test in which the examiner presses the end of the monofilament against the skin until it bends, then removes it from the skin surface and notes the patient’s response (Fig. 30-6). The monofilaments have reliability at the 95% confidence level.6 They are used to categorize feet into those with normal sensation (4.17 diameter: 1g pressure); loss of protective sensation requiring protective footwear (5.07 diameter: 10g pressure); and no sensation (6.10 diameter: 75g pressure). Ulcer risk is proportional to the severity of sensory loss. Although Semmes-Weinstein monofilaments can be obtained in larger sets, researchers at the Hansen’s Disease Center (Carville, LA) concluded that testing with the three sizes noted is sufficient for grading the insensitive limb. Use of the monofilament is not to be confused with testing for sharp/dull sensation.
Temperature
Areas of increased skin temperatures (hot spots) offer another physical sign that is helpful in detecting areas prone to ulceration.5 Therefore, palpating the surface of the foot should be a part of every foot examination, including twice-daily self-examination for all patients with feet at risk for ulceration.15 Temperature scanning/mapping of areas that commonly break down can be precisely done with surface-sensing devices (thermocouple or infrared) (Fig. 30-7). The infrared units allow recording of multiple readings, providing a rapid scan of the limbs. When one area definitely has a temperature 3°F (2°C) or more higher than adjacent areas, it can be assumed that there is an area of inflammation due to high pressure, Charcot neuroarthropathy (fracture/dislocation), or infection. This area must be immediately relieved of pressure until a definitive diagnosis has been made, allowing appropriate treatment to be instituted. On follow-up of the patient, the temperature differential should decrease as healing progresses. Vascular impairment should be suspected when one limb is significantly colder or distal portions of the foot show a drop in temperature.12 It should be remembered, however, that the lower limbs normally become somewhat cooler from proximal to distal.5
Documentation
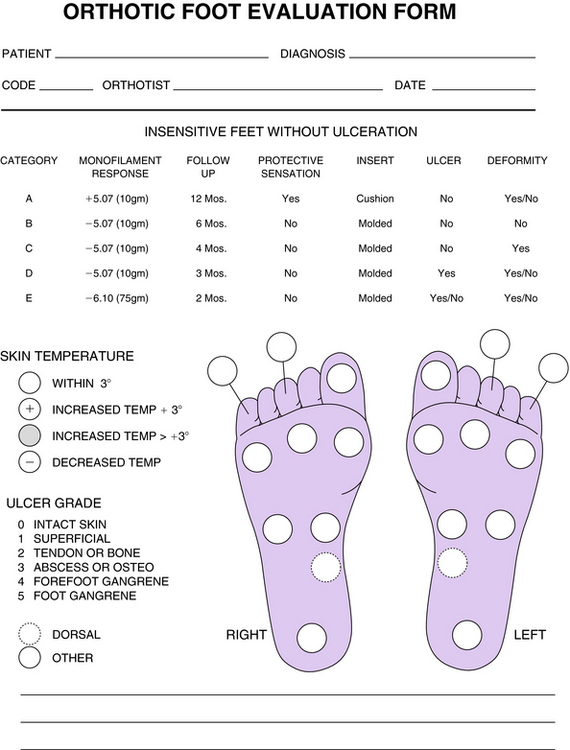
Continuity of documentation is essential to ensure high-quality care. This requires a standard form for initial assessment and future follow-up (Fig. 30-8). Tracing the outline of an ulcer on transparent radiological or other rigid film allows for a detailed record of healing progression. Providing the patient with a duplicate tracing to follow the progress of the ulcer may improve compliance. Photographs of an ulcer are important for visualizing reduction in its area and volume.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree