Orthoses in the Management of Hand Dysfunction
Noelle M. Austin and MaryLynn Jacobs
He who works with his hands is a laborer, He who works with his hands and his mind is a craftsman, He who works with his mind and his heart is an artist.
Unknown
Learning objectives
On completion of this chapter, the reader will be able to:
3. Identify the three arches of the hand along with creases and discuss their significance.
4. Identify a 90-degree angle of pull and explain its importance in the application of force.
6. Explain the importance of patient education related to proper orthosis wear, care, and precautions.
The hand is the body’s tool to interact with the surrounding environment. A hand afflicted with disease or injury greatly impairs the ability to function, even if normal functioning proximal joints and muscles are present. The therapist’s ability to provide clinical intervention can positively affect the use of the hand and therefore overall function. One tool at a therapist’s disposal is orthotic intervention. The appropriate use of orthoses during specific phases of tissue healing, depending on the diagnosis, can be an effective adjunct to traditional therapy techniques for restoring use of the limb. Treatment decisions must be based on an integration of knowledge and clinical experience along with information specific to the individual patient, including diagnosis, general medical status, and the physician’s prescription. Clinicians need to understand the principles associated with orthotic design and fabrication.
This chapter focuses on orthotic fabrication for the hand and upper extremity and includes discussion of nomenclature, materials, mechanical and anatomical principles, and case studies to provide examples of orthotic intervention with an emphasis on critical thinking.
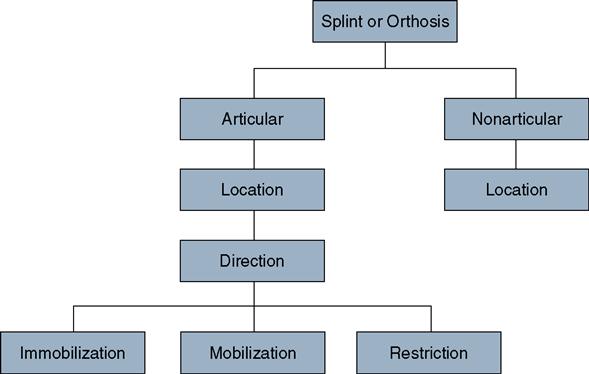
Nomenclature
In the medical literature, the terms splint, brace, support, and orthosis have similar definitions.1,2 This is often confusing to physicians, therapists, students, insurance companies, and even those who fabricate these devices. Are splints made by a therapist? Is an orthosis made by an orthotist? In 1989, the American Society of Hand Therapists (ASHT) put together a task force to address issues such as proper nomenclature and redefinition of orthoses in an attempt to enhance and clarify communication among all disciplines.1 The task force developed a Splint Classification System (SCS) and addressed the similarity in definitions of the words splint, brace, support, and orthosis (Figure 14-1). The task force’s review confirmed that these words were so similar in nature that they were used interchangeably in the hand therapy literature. Another key issue that challenged the task force was how to define orthoses to provide universal comprehension and approval. Currently, there is a shift in nomenclature from the word ‘splint’ to ‘orthosis’ in order to follow Center for Medicare and Medicaid Services (CMS) guidelines for billing and reimbursement purposes. Therefore, the word orthosis will be utilized throughout this chapter and should be adopted in clinical and billing documentation as well.3
Traditionally, orthoses have generally been described according to their form (e.g., thumb spica splint, wrist cock-up splint, ulnar gutter splint).4 This form-based nomenclature, however, can often lead to confusion and misunderstanding regarding the actual orthosis requested. The SCS painstakingly describes most universally used orthoses according to their specific function (e.g., thumb immobilization splint, wrist/hand extension mobilization splint). This functional-based description of orthoses gives clinicians a clear concept of what the orthosis must look like and what its function should be. The specific categories described by the SCS are outlined in Figure 14-1.
Articular and Nonarticular Orthoses
Orthoses are classified into two broad categories: articular and nonarticular. Articular orthoses, the most common type of fabricated orthosis, are those that cross a joint or series of joints. Examples of articular orthoses include a wrist immobilization orthosis, proximal interphalangeal (PIP) joint extension mobilization orthosis, and elbow flexion restriction orthosis. The word articular is implied in the orthosis description and is not necessary in the title of the orthosis.
Nonarticular orthoses do not cross a joint; instead, they stabilize the body segment to which they are applied. The ASHT recommends that clinicians include the term nonarticular before an orthosis description; an orthosis used to stabilize the humerus would be called a nonarticular humerus orthosis, and an orthosis designed to soley stabilize a metacarpal would be called a nonarticular metacarpal orthosis. Without this designation, the orthosis fabricator may not know whether to include or exclude proximal or distal joints in the orthotic design.
Location
Location refers to the specific body part or joint levels acted on by the orthosis. The primary joint is the target joint. The secondary joints are included for protection, stabilization, or comfort. When several primary joints are involved (e.g., crush injury to the hand), the description of the orthosis can be simplified by grouping all the joints together, such as hand orthosis or digit orthosis.
Direction
Direction refers to the primary direction of the force applied when the orthosis is worn. This includes flexion, extension, radial or ulnar deviation, supination, pronation, abduction, and adduction. Information regarding direction is essential because it tells the clinician the desired joint positioning. Direction notation is also critical when fabricating a mobilization orthosis; accurate application of the direction of force is essential to achieve the goal of joint or soft tissue mobility.
Purpose of Orthosis
The purpose or intent of the orthosis is the single most important aspect documented in the description. The purpose of the orthosis can be to (1) immobilize a structure, (2) mobilize a tissue, or (3) restrict an aspect of joint motion.
Immobilization
The purpose of an immobilization orthosis is simply to place a structure in its anatomical or most comfortable resting position. Immobilization orthoses are perhaps the most common and simple form, although it can be used for complex injuries. Immobilization orthoses immobilize the joints they cross.
Mobilization
Mobilization refers to moving or stretching specific soft tissues or joints to create change. The benefits of using mobilization orthoses as a treatment modality have been well documented in the literature.5–8 The effectiveness of mobilization does not rely on stretching tissue but rather on the facilitation of cell growth. The target tissue lengthens when the living cells of the contracted tissues are stimulated (by the application of force) to grow. This stimulation occurs when steady tension is applied through the orthosis over a specific period of time. The living cells recognize the tension applied and permit the older collagen cells to be actively absorbed and replaced with new collagen cells oriented in the direction of tension.9–16 Tissue growth has been clearly demonstrated in certain cultures in which elongating certain body parts, such as earlobes and lips, is popular. In these cultures, dowels are used to serially increase the diameter of the intended structure, slowly allowing expansion and accommodation of the new tension and diameter. Another common example includes the use of braces and retainers in the dental field. There are three choices of orthotic design to mobilize tissue, including serial static, static progressive, and dynamic orthoses.
Restriction
Restriction orthoses restrict or block an aspect of joint motion. These are generally simple orthoses applied in such a way that they limit motion. Therapists can construct static orthoses, dynamic orthoses, and forms of taping to become types of restrictive orthoses because they can be made to restrict some portion of joint motion while allowing full motion in the opposite direction.
Examples
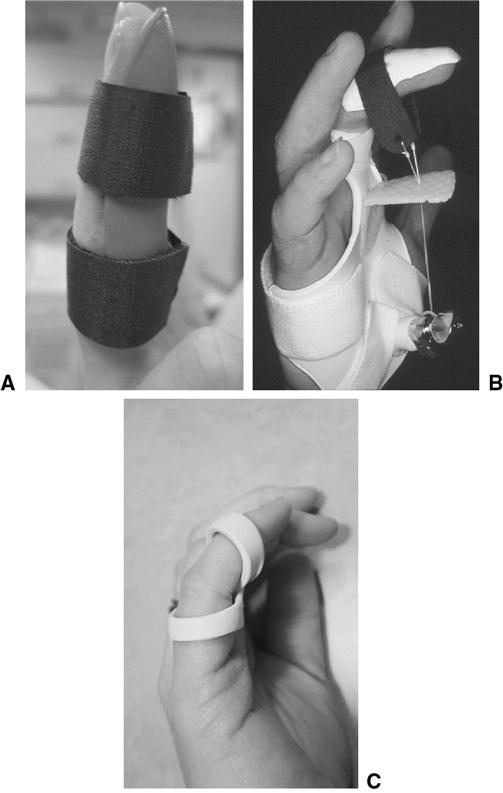
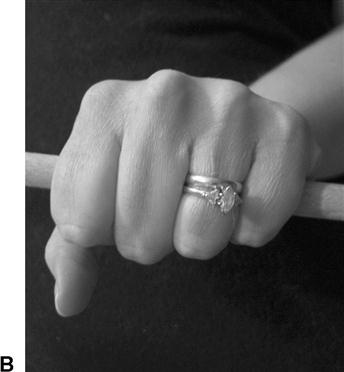
Figure 14-2 demonstrates the critical impact that the words immobilization, mobilization, and restriction can have when describing an orthosis. Within the PIP immobilization orthosis (see Figure 14-2A), the PIP joint is immobilized in a comfortable resting position to allow the involved structures to heal, commonly used for a PIP ligament sprain. The PIP flexion mobilization orthosis stretches the PIP joint into flexion to address a PIP extension contracture (using a static progressive approach) (see Figure 14-2B). The PIP joint is restricted from full extension but allowed to flex fully within the boundaries of the PIP extension restriction orthosis, which is commonly used for swan neck deformities when the PIP joint pulls into hyperextension (see Figure 14-2C).
Design Descriptors
Design descriptors are used to increase clarity of the specific orthosis request and provide detail in notes or for correspondence to physicians or reimbursement sources. The design descriptors are non-SCS nomenclature but are commonly used by the hand therapy and surgery community.17 The most commonly used descriptors are summarized in Box 14-1.
Choices of Orthotic Designs
The choices of orthotic design include familiar terminology: static, serial static, dynamic, and static progressive orthoses. An orthotic design should be chosen to achieve the goals of immobilization, mobilization, or restriction of a specific tissue.
Static Orthoses
Static orthoses have a rigid base, immobilizing the joints they traverse (Figure 14-3). A static orthosis provides stabilization, protection, and support to a body segment such as the elbow, wrist, or finger. Static orthoses are perhaps the most common orthoses made. They can be used as an adjunct to treatment, an exercise device, by blocking a distal or proximal joint to increase glide of another joint or improve tendon excursion.
Serial Static Orthoses
Serial static orthoses or casts are applied with the joints, soft tissue, or musculotendinous units they cross in a lengthened position (near maximum) and are worn for extended periods of time (Figure 14-4). Tissue held in this end-range position should react and accommodate by stretching into the desired direction of correction. Serial static orthoses are often removed during therapy and exercise sessions so that the clinician and patient can work on the involved structures with modalities such as heat, ultrasound, joint mobilization, and range of motion (ROM). The orthosis or cast is then remolded to maintain the gains made during the exercise session. This design may provide greater patient compliance and ensures that the tissue is being continually stressed without the risk of the tissue rebounding (reverting back to original shortened state) upon removal of the orthosis. Some therapists use an approach with serial static orthoses when the orthosis is worn continuously for a few days and then removed in therapy. In other cases, using these orthoses at night only can help maintain the gains made throughout the day with exercise and stretching. Nonremovable serial static orthoses may also be a better choice for patients who are young, who have cognitive or behavioral issues, or who have fluctuating tone and spasticity.
Dynamic Orthoses
Dynamic orthoses use an elastic-type force to mobilize specific tissues to achieve increases in ROM (Figure 14-5). Most dynamic orthoses have a base that permits the attachment of various outriggers and components. The mobilizing forces applied through a dynamic orthosis are elastic (stretchy) in nature, such as rubber bands, springs, or wrapped elastic cord. The dynamic force applied continues as long as the elastic component can contract, even when the tissue reaches the end of its elastic boundary.18
Static Progressive Orthoses
Static progressive orthoses achieve tissue mobilization by applying low-load force to the tissue’s end range in one direction over a long period of time (Figure 14-6).5 The goal is that the tissue will eventually accommodate to this position. The fabrication of a static progressive orthosis is similar to a dynamic orthosis, but the force applied is static or nonelastic. The mobilization force can be generated through static line, nonelastic strapping materials, hinges, turnbuckles, and various types of inelastic tape. When the joint position is achieved and the tension on the static progressive component is set, the orthosis will not continue to stress the tissue beyond its elastic limit.18 Force can be altered by the patient or therapist through progressive adjustments. Some patients may tolerate static progressive orthoses better than dynamic. One reason may be that the joint position is constant while the tissue accommodates gently and gradually to the tension, without the influences of gravity and motion.18,19
Objectives for Orthotic Intervention
The key objective for orthotic fabrication may not always be straightforward. The objectives for orthotic intervention may be multiple, as in a wrist and hand immobilization orthosis (resting hand orthosis) used on a patient with rheumatoid arthritis. The orthosis may be constructed to immobilize inflamed arthritic joints, yet place the metacarpophalangeal (MP) joints serially in a gently extended and radially deviated position to minimize ulnar drift and periarticular deformity. Critical thinking is a necessary process when fabricating orthoses; multiple injuries, wound status, age, and lifestyle are a few of the key factors that must be taken into consideration. More skilled clinicians can appreciate that there can be several purposes for one orthosis; therefore creative problem solving must be used when fabricating orthotic devices for the more involved, complex injury.
Immobilization Orthoses
Orthoses designed to hold or immobilize a joint or limb segment can be used to do the following17:
• Protect and position edematous structures
• Aid in maximizing functional use
• Protect healing structures and surgical procedures
• Provide support and protection for soft tissue healing
• Maintain and protect reduction of fracture
• Improve and preserve joint alignment
• Block and transfer muscle and tendon forces
Mobilization Orthoses
Orthoses designed to change or mobilize tissues or structures are used to do the following17:
Restriction Orthoses
Orthoses designed to restrict or limit motion may be used to do the following17:
Anatomy-related principles
Therapists treating the upper extremity need to have a thorough understanding of the complex anatomical features of the hand and arm to manage patients with dysfunction effectively. Disturbance of the delicate relationship between the bones, muscles, nerves, and other soft tissue structures, either by disease or trauma, can result in disruption of normal function. Knowledge of normal anatomical features and how pathological conditions affect them is important for therapists to make appropriate clinical decisions regarding treatment interventions.11,20–22
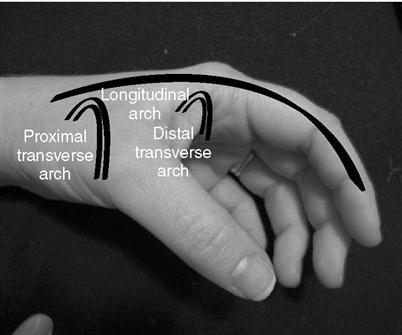
Arches of the Hand
The configuration of the bones in the hand, along with the tension of the muscles and ligaments in this region, contribute to the creation of an arch system composed of the proximal transverse, distal transverse, and longitudinal arches (Figure 14-7).23,24 This arch system is vital for positioning the hand to allow for normal function related to grasp and prehension.24,25 Incorporating these arches within an orthosis is essential to allow maximal function and comfort. Including the arches also prevents orthosis migration on the extremity.
The fixed proximal transverse arch is created by the configuration of the distal row of the carpal bones and the taut volar carpal ligament. This region is also referred to as the carpal tunnel, through which the long flexors and median nerve pass en route to the hand.26 This fixed structure provides mechanical advantage to the flexors, maximizing grasp function.
The mobile distal transverse arch is located at the level of the metacarpal heads. This arch is adaptive by the mobile ulnar fourth and fifth carpometacarpal (CMC) joints and highly mobile thumb trapeziometacarpal joint.27 This increased mobility of the peripheral digits allows for optimal grasping abilities.
The longitudinal arch spans the length from the metacarpal to the distal phalanx. A disruption of this arch occurs in patients who have sustained an ulnar nerve injury with resulting loss of intrinsic muscle function. In this situation, the hand takes on an intrinsic minus position with the MP joints hyperextended and the PIP and distal interphalangeal joints flexed (clawlike deformity).23
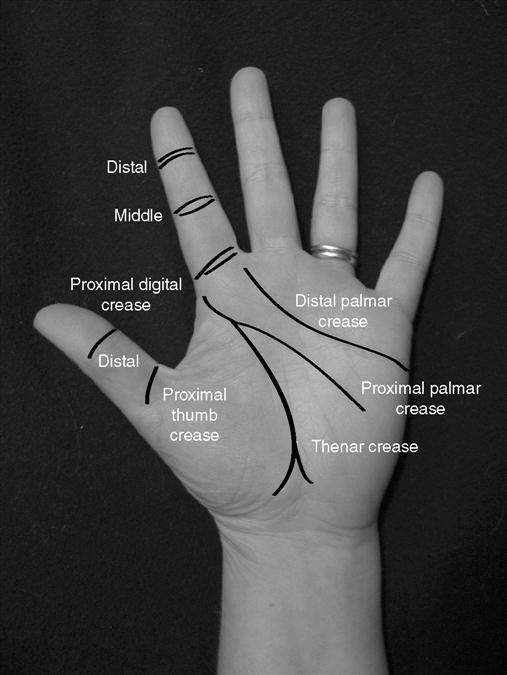
Palmar Creases
The regular arrangement of creases is easily visible on the volar surface of the hand (Figure 14-8). The thick palmar skin is fixed to the underlying structures by fibrous connections that aid in formation of these creases.27 Therapists need to appreciate the location of these creases and how they correlate with the underlying anatomy. Commonly, these creases are used by therapists as an anatomical guide when creating orthosis patterns. For example, the distal palmar crease and proximal palmar crease must be fully cleared when fabricating a wrist immobilization orthosis to allow for unrestricted ROM at the MP joints. However, care must be taken not to clear too much because the mechanical advantage of the orthosis can be adversely altered.17
Metacarpal Length and Mobility
Dual obliquity is a concept relating to the anatomy of the metacarpals.23,25 Because of the differing lengths of the metacarpals (radial side of hand longer than ulnar), when an object is held in the hand, an oblique angle is formed compared with the distal ends of the radius and ulna (Figure 14-9A). In addition, the object is angled in accordance with the distal transverse arch and increasing mobility of the ulnar metacarpals (see Figure 14-9B). This dual obliquity should be incorporated into the orthosis to provide a comfortable and functional orthosis that resists migration because of the incorporation of the arches.
Positioning the Hand
When deciding how to position the hand within an orthosis, many factors must be considered, including the patient’s diagnosis, healing time frame, and intervention goals. Being mindful of proper positioning within an orthosis initially can help prevent future joint and soft tissue contractures. The two most common positions described in the literature include the position of function and the position of rest.17,28 See Figure 14-10 for the general joint angles described for each position.
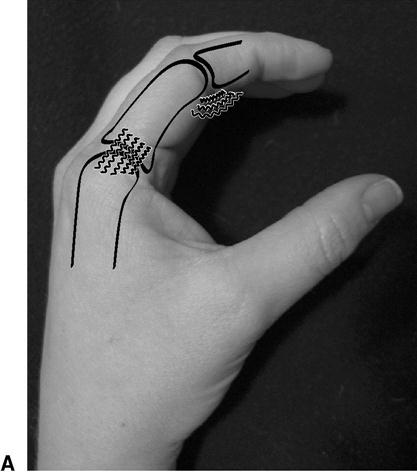
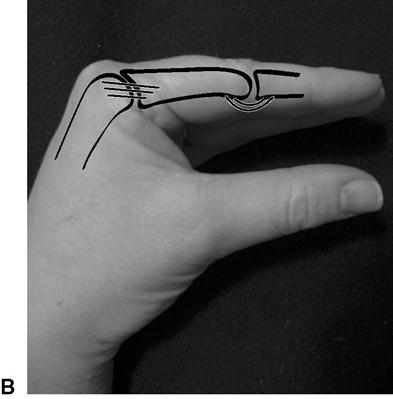
The antideformity position considers the unique anatomical characteristics of the MP and PIP. The length of the collateral ligaments at the MP joint varies according to the position of the MP joint (Figure 14-11).29 The collateral ligaments are slack with MP joint extension, whereas tension in the collateral ligaments increases with greater amounts of MP joint flexion. Placing the joints in flexion within an orthosis helps prevent MP joint extension contractures (limited flexion). If the joints were placed in extension with resulting MP contractures, the disruption of the longitudinal arch would greatly impair grasping abilities.
Similarly at the PIP joint level, the volar plate is placed on tension with PIP joint extension, whereas flexion at the PIP joint places the volar plate at risk for shortening (see Figure 14-11A and B).29 Shortening of the volar plate could result in debilitating PIP joint flexion contractures, which can significantly affect the ability to grasp and especially release objects. Therefore careful positioning of the PIP joint in extension (as long as not contraindicated per the diagnosis) is crucial to maintain the length of the volar plate.
Tissue Precautions
In the upper extremity, a number of areas exist where bony protuberances or superficial nerves are highly susceptible to compression from orthoses (Box 14-2).30 If these areas are not accounted for in the fabrication process, the orthosis will likely be uncomfortable for the patient and therefore possibly not worn. Special consideration must be given to the patient with impaired sensation (those with peripheral nerve injury, neuropathy, nerve root compression, or central nervous system disorders). Those with limited or absent sensation do not have the normal ability to feel or detect areas of excess pressure; instead, they must rely on visual inspection to determine integrity of skin and soft tissue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree