13
Orthopedic Pharmacology
1. Discuss pharmacokinetic concepts, including absorption, distribution, metabolism, excretion half-life, and duration of action, and their relationship and significance to rehabilitation therapies.
2. Discuss pharmacodynamic concepts including the dose–response relationship, therapeutic window, adverse drug reactions, toxicity, tolerance, withdrawal, and addiction.
3. List the general principles of safe medication use and the physical therapist assistant’s role in optimizing patient safety.
4. Discuss general principles of treatment and prevention of orthopedic infection including why such infections are difficult to treat and importance of antibiotic compliance.
5. Discuss the analgesics best suited for different types of pain.
6. Discuss how opioids work differently from antiinflammatory analgesics in the treatment of pain.
7. Discuss common side effects and precautions associated with opioids, acetaminophen, nonsteroidal antiinflammatory drugs, cyclooxygenase-2 inhibitors, and corticosteroids.
8. Discuss the risk of acetaminophen overdoses during pain management.
BASIC PRINCIPLES OF PHARMACOLOGY AND SAFE MEDICATION USE
Pharmacokinetics
Simply put, pharmacokinetics is a term used to describe what the body does to a medication. The four pharmacokinetic phases are (1) absorption, (2) distribution, (3) metabolism, and (4) excretion.7
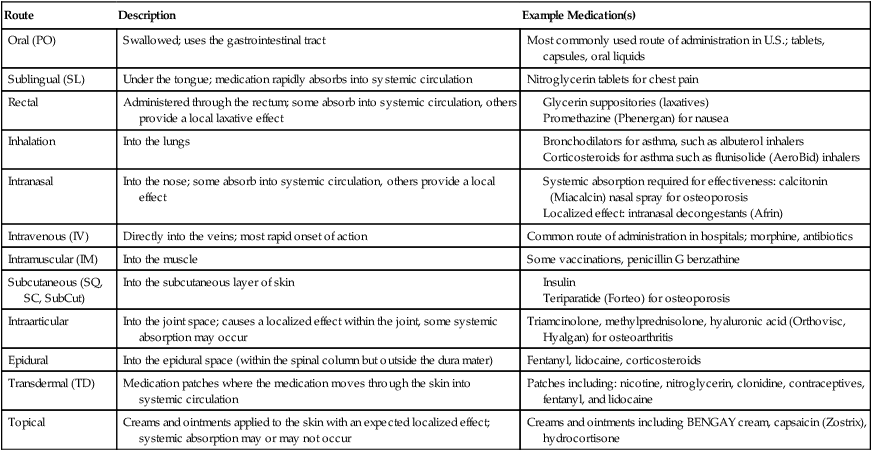
Absorption describes how the medication moves from its site of administration into the systemic circulation (into the bloodstream). Some common routes of administration are shown in Table 13-1. Most medications must move from the site of administration into systemic circulation to be effective. Others, such as topical creams or inhalers, may provide therapeutic benefits through a localized effect. Although systemic absorption may not be necessary for effectiveness of topically applied medications, it can occur and result in side effects. For example, high dose, long-term use of inhaled corticosteroids to treat asthma has been shown to result in enough systemic absorption to increase the risk of developing osteoporosis.12,15
Table 13-1
List of Common Routes of Administration
| Route | Description | Example Medication(s) |
| Oral (PO) | Swallowed; uses the gastrointestinal tract | Most commonly used route of administration in U.S.; tablets, capsules, oral liquids |
| Sublingual (SL) | Under the tongue; medication rapidly absorbs into systemic circulation | Nitroglycerin tablets for chest pain |
| Rectal | Administered through the rectum; some absorb into systemic circulation, others provide a local laxative effect | |
| Inhalation | Into the lungs | |
| Intranasal | Into the nose; some absorb into systemic circulation, others provide a local effect | |
| Intravenous (IV) | Directly into the veins; most rapid onset of action | Common route of administration in hospitals; morphine, antibiotics |
| Intramuscular (IM) | Into the muscle | Some vaccinations, penicillin G benzathine |
| Subcutaneous (SQ, SC, SubCut) | Into the subcutaneous layer of skin | |
| Intraarticular | Into the joint space; causes a localized effect within the joint, some systemic absorption may occur | Triamcinolone, methylprednisolone, hyaluronic acid (Orthovisc, Hyalgan) for osteoarthritis |
| Epidural | Into the epidural space (within the spinal column but outside the dura mater) | Fentanyl, lidocaine, corticosteroids |
| Transdermal (TD) | Medication patches where the medication moves through the skin into systemic circulation | Patches including: nicotine, nitroglycerin, clonidine, contraceptives, fentanyl, and lidocaine |
| Topical | Creams and ointments applied to the skin with an expected localized effect; systemic absorption may or may not occur | Creams and ointments including BENGAY cream, capsaicin (Zostrix), hydrocortisone |
The rate and extent of drug absorption through the skin can be dramatically increased by application of heat; therefore heat generating modalities (e.g., heating pads, ultrasound, infrared lamps, and warm hydrotherapy) should not be applied near transdermal medication patches. Electromagnetic (e.g., ultraviolet radiation, lasers, and diathermy) and electrical current modalities (e.g., transcutaneous electrical nerve stimulation [TENS]) should also not be used near medication patches because many patches have metallic backings that conduct electric currents, leading to significant heat generation and burns.3
Medications are cleared from the body through metabolism, excretion, or both. Metabolism is the biotransformation or chemical alteration of the medication. The byproduct of drug metabolism is called a metabolite. Through metabolism, some medications are inactivated, whereas others remain active (active metabolite) but are more water soluble for easier elimination by the kidneys. Generally, metabolism takes place in the liver but it can occur through enzymatic processes in the kidneys, lungs, and bloodstream. Differences in drug response, side effects, and safe dose can be greatly affected by genetic differences in drug metabolism.21
Pharmacodynamics
Simply put, pharmacodynamics is a term used to describe what the medication does to the body. It is a study of the relationship between the amount of drug in the body and the response observed.7 Pharmacodynamics include a wide variety of principles, such as the dose–response relationship, therapeutic window, adverse reactions, and toxicity.
Tolerance occurs when the reaction to a drug diminishes over time. Tolerance can occur to both the benefits of a medication (making it less effective over time) and the ADRs (making it better tolerated over time).4 Withdrawal symptoms indicate physical dependency and are expected to occur with certain medications when used over a prolonged period. Withdrawal symptoms are generally the opposite of the pharmacologic effects of the medication. For example, one withdrawal symptom of a medication used to lower blood pressure would be hypertension.
Psychological dependency, also called addiction, occurs with certain medications such as opioid analgesics, amphetamines, and benzodiazepine sleep aids, as well as other substances with abuse potential, including cocaine, heroin, alcohol, caffeine, and nicotine. Withdrawal symptoms do contribute to the development of addiction in that the patient continues to use the substance to avoid the unpleasantness of the withdrawal symptoms; but having withdrawal symptoms alone does not meet the definition of addiction. It is important to understand the difference between physical and psychological dependency.4 Psychological dependency and addiction involve strong cravings and desires for the drug that overwhelm daily life. There is a loss of control over its usage and use continues despite its negative impact on quality of life.4,6 Drug addiction is most strongly associated with medications that rapidly distribute into the CNS causing high levels of euphoria and dysregulation of the neurotransmitters involved in the body’s natural reward and pleasure centers.







