19
Orthopedic Management of the Hip and Pelvis
1. Identify common hip fractures.
2. Outline and discuss common methods of management and rehabilitation of ordinary hip fractures.
3. Identify and describe common methods of management and rehabilitation after hip arthroplasty.
4. Identify and describe common soft-tissue injuries of the hip.
5. Outline and describe common methods of management and rehabilitation of soft-tissue injuries of the hip.
6. Identify common fractures of the pelvis and hip.
7. Discuss methods of management and rehabilitation for fractures of the pelvis and acetabulum.
HIP FRACTURES
The clinical significance of hip fractures is reflected in the annual rate of fractures and the financial burden to the economy that hip fractures produce.10,16 Goldstein10 states that more than 300,000 fractures occur annually with an associated cost of $10 billion. Other authorities4,16 report that 267,000 fractures occur annually, with a price tag of $33.8 billion.4 Although fractures in general occur to all age groups, hip fractures are most common among elderly women.4,16,17 Hip fractures in women can be attributed in part to the higher incidence of osteoporosis in this group17; with regard to age, hip fractures represent the most common acute orthopedic injury in the geriatric population.16
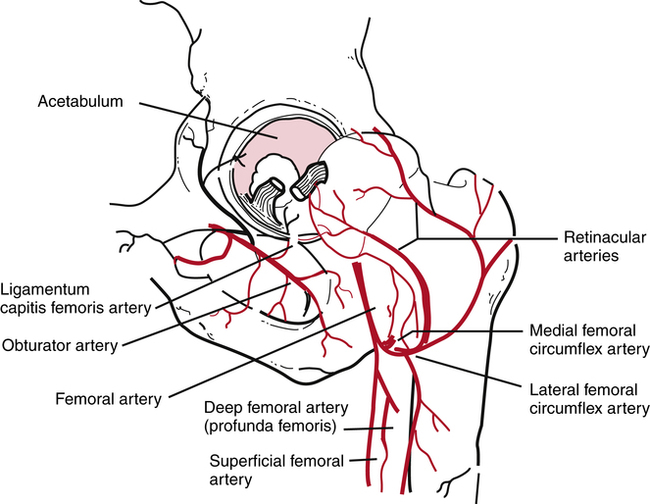
The classification of hip fractures is clinically significant for the PTA because the severity and location of the fracture profoundly affect surgical management and physical therapy interventions. The vascular supply to the femoral head and neck may be significantly compromised with certain fracture patterns and levels of severity (Fig. 19-1).17 LeVeau17 states, “The extent of the supply of blood to the head of the femur determines remodeling and healing after femoral neck fracture or hip dislocation.”
Generally, hip fractures can be classified by location and described by severity (simple or comminuted).9 Fractures of the hip can be located in the following areas:
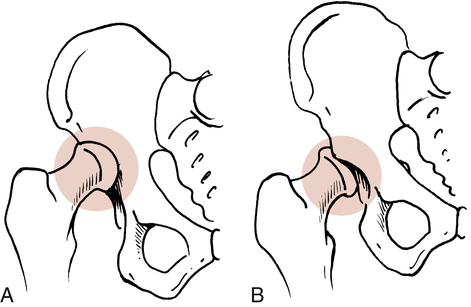
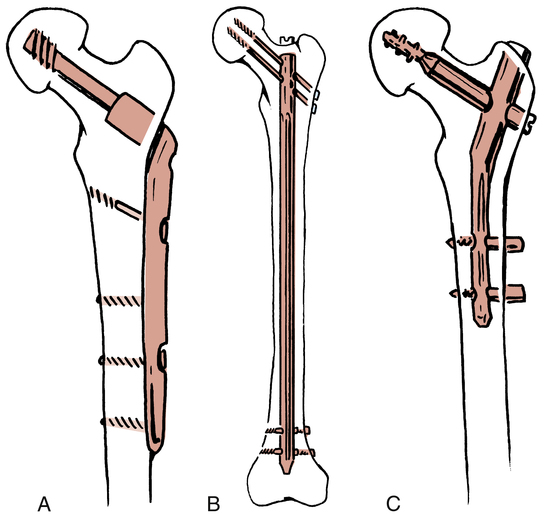
 Extracapsular or intertrochanteric9,10,21 (Fig. 19-2, A)
Extracapsular or intertrochanteric9,10,21 (Fig. 19-2, A)

 Femoral neck or subcapital areas11 (intracapsular) (Fig. 19-2, B)
Femoral neck or subcapital areas11 (intracapsular) (Fig. 19-2, B)
 Proximal femoral shaft or subtrochanteric areas (Fig. 19-2, C)11
Proximal femoral shaft or subtrochanteric areas (Fig. 19-2, C)11
Secondary to the location and severity of hip fracture, the most significant complication is related to osteonecrosis and the loss of blood supply to the femoral head leading to avascular necrosis (AVN). Gross and associates11 affirm, “any fracture of the neck (femoral) can disrupt this tenuous blood supply. As a result, there is an exceedingly high incidence of avascular necrosis of the femoral head after hip fractures.” LeVeau17 states, “avascular necrosis may occur after hip fracture in about 65% to 85% of the patients.”
Three main clinical complications are noted with subtrochanteric fractures: malunion, delayed union, and nonunion avascular necrosis.18 Two factors associated with malunion and nonunion of subtrochanteric hip fractures are:
 The subtrochanteric area of the proximal femur is cortical bone, which has a decreased blood supply.
The subtrochanteric area of the proximal femur is cortical bone, which has a decreased blood supply.
 The subtrochanteric area is prone to large biomechanical stresses that can lead to loosening of various fixation devices.18 This complication must be considered by the PTA when treating patients with this type of fracture.
The subtrochanteric area is prone to large biomechanical stresses that can lead to loosening of various fixation devices.18 This complication must be considered by the PTA when treating patients with this type of fracture.
Many options are available in treating hip fractures: The choice depends on the patient’s age, location of the fracture, quality of bone, severity of the fracture (simple, displaced, or comminuted), activity level of the patient, associated soft-tissue injuries, and specific goals for the patient’s return to activity. Generally, hip fractures are managed surgically with an open reduction with internal fixation (ORIF) procedure that secures the fracture fragments with various rods, nails, pins, screws, and plates.9,10,16 Some hip fractures can be managed conservatively with bed rest, traction, and protected weight bearing.18 For example, in a fractured greater trochanter where the displaced fracture fragment is less than 1 cm (as evaluated by the physician radiographically), the treatment could be bed rest for several days, range of motion (ROM) exercises, and limited weight bearing for 4 weeks.18
With an isolated lesser trochanteric fracture (most common in adolescents), the physician bases treatment on the amount of fragment displacement. If the fracture is displaced more than 2 cm, the physician could perform an ORIF procedure; if the fragments are in closer apposition, the physician may elect rest, protected weight bearing, and limited exercise for 3 to 4 weeks.18 Figure 19-3 depicts common fixation devices used to secure fracture fragments using an ORIF procedure.
While treating patients with hip fractures, the PTA must be aware that venous thrombosis is a potentially critical complication after hip surgery. Without prophylactic medications to minimize thrombosis, statistics show that 40% to 90% of patients develop this condition after hip surgery.18 Venous thrombosis is the most common complication after hip fracture in the elderly population of patients.18
Hip fractures and dislocations can occur in combination, as well as isolated events. Usually hip dislocations are either anterior or posterior (Fig. 19-4). Isolated hip dislocations generally are treated conservatively with bed rest, traction, and protected limited weight bearing for up to 12 weeks.18 For example, with an anterior hip dislocation, bed rest with traction is prescribed, with specific precautions to strictly avoid extreme hip abduction and external rotation to prevent redislocation. Usually protected weight bearing is allowed when the patient can achieve painless hip ROM around 3 to 4 weeks after the incident.18 Conversely an isolated posterior hip dislocation is treated with bed rest and traction in abduction with precautions to prevent hip abduction, flexion, and internal rotation to protect the joint from dislocation.18
Rehabilitation after Hip Fractures
The patient’s overall preoperative physical and mental condition is a predictor of postoperative success. Patients with major cardiovascular or pulmonary disease processes, obesity, osteoporosis, dementia or poor upper body strength are at increased risk for postoperative complications. Overall mortality rates of 20% after 1 year, 50% at 3 years, 60% at 6 years, and 77% after 10 years have been reported.7
Although the overall goal of rehabilitation is to restore patients to preinjury level, this may not be realistic. Only 20% to 35% of patients regain their preinjury level of independence. As many as 15% to 40% require institutionalized care for more than 1 year after surgery. Many (50% to 83%) require devices to assist with ambulation.14
The progression from maximum to minimum protection closely follows the rate of bone healing. However, other factors are considered in safely and effectively providing an environment for the return to functional activities. In the maximum-protection phase of recovery (phase 1 to 21 days postoperatively, as described by Goldstein9), the fracture site is protected; pain and swelling are reduced; and isometric exercises, gentle protected ROM, and limited weight bearing begin.9,17
The general goals of recovery are to increase muscular strength specific to the surgery, improve overall conditioning, increase ROM of the affected hip, enhance aerobic fitness, increase local muscular endurance, reduce pain and swelling, reestablish normalized gait mechanics, and protect the healing structures from internal and external forces that can impede healing.9,17
Goldstein9 identified a few major complications that occur, particularly during the maximum-protection phase of recovery. Generally, no combined diagonal or rotary forces are used in exercises during this phase. Hardware loosening and delayed healing may occur if increased torque is placed through the healing fracture site by excessive unwanted forces.9 No active straight-leg raises or supine hip bridges should be performed during the first 6 to 8 weeks after surgery. Goldstein states, “The power generated by the massive hip muscles is so great during those exercises that there is a danger of displacing the fractured segments.”9
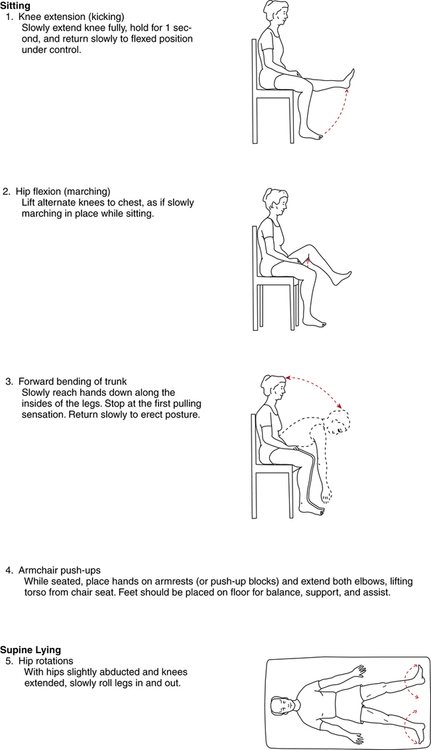
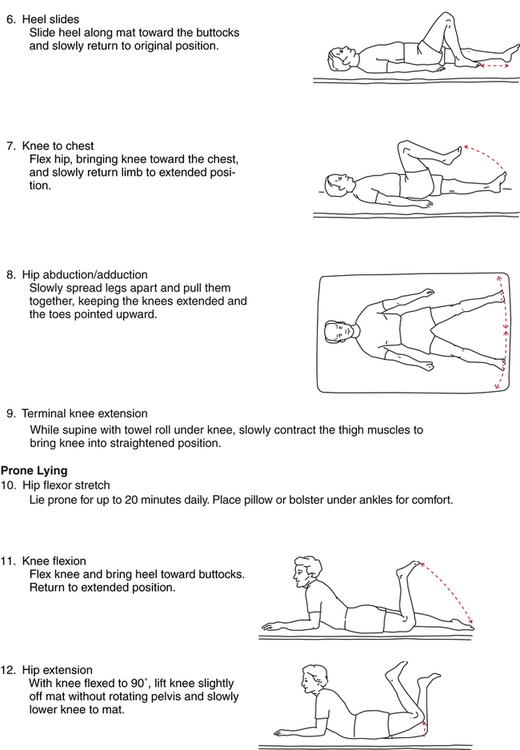
In addition to rudimentary isometric quadriceps sets, gluteal sets, ankle pumps, and gentle hip-motion exercises, authorities advocate adding the exercises described in Figure 19-5 progressively during the first 3 weeks after surgery,9 although exercises number 3 (forward bending of trunk) and 12 (hip extension in prone) are not advocated by the author of this chapter.
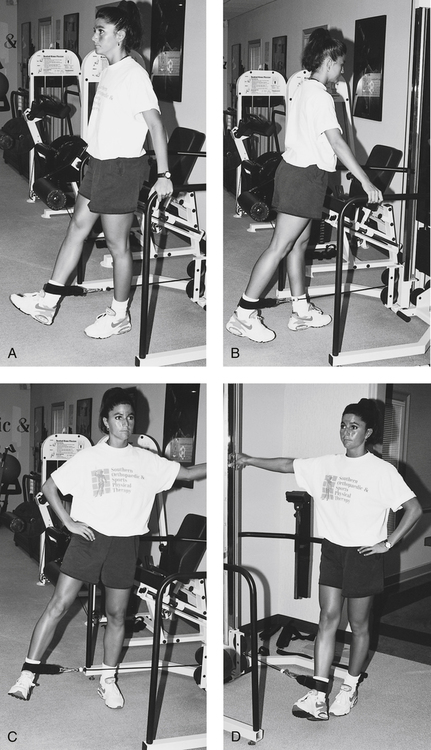
The moderate-protection phase, defined as 3 to 6 weeks after surgery,9 provides for more challenging exercises directed at regaining hip and knee motion, improving quadriceps and hamstring strength, and increasing strength to the hip extensors, abductors, and adductors. Standing four-position hip strengthening can be achieved initially without any resistance until a proper pattern of movement is achieved. Advancing this exercise can be accomplished using a cable system (Fig. 19-6), lower levels of Thera-Band, or ankle weights. The initiation of limited ROM leg presses can commence during this phase as well.
PROXIMAL FEMORAL OSTEOTOMY
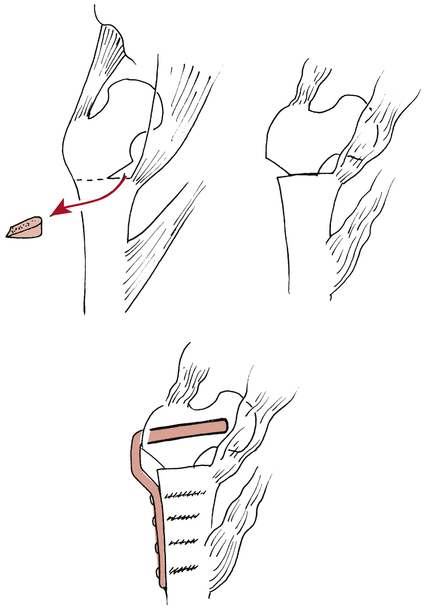
Intertrochanteric osteotomy may be performed when degenerative joint disease (DJD) is extensive and results in hip pain associated with subchondral bone erosion, articular cartilage fibrillation and fissuring, and hip joint incongruity.15 The goal of this surgical procedure is to reduce pain and improve function related to advanced osteoarthritis by surgically changing the femoral neck-shaft angle so that healthy cartilage is exposed, thus “improving joint surface congruity.”15 Figure 19-7 illustrates this procedure and shows the changed neck-shaft angle relationship, reduced ligamentous and muscular tension, and improved joint articulation occurring after surgery.15
Rehabilitation after Proximal Femoral Intertrochanteric Osteotomy
Weight-bearing status is highly individualized but generally is progressed according to the rate and quality of bone healing. Typically, a walker or crutches reduces compressive loads through the hip during TDWB, PWB, and non–weight bearing (NWB) gait techniques. In most cases, protected weight bearing is strictly enforced for 8 to 12 weeks after this procedure.15
HEMIARTHROPLASTY OF THE HIP
For femoral head osteonecrosis or severe femoral head fractures, hemiarthroplasty is used to eliminate pain and improve function. This procedure replaces the damaged femoral head with a bipolar prosthesis. Because hemiarthroplasty requires a normal acetabular surface,15,22 it is rarely used for arthritis.22 This is considered a conservative procedure15 when compared with a total hip replacement. Hemiarthroplasty can be converted at a later date to total hip replacement if symptoms persist and the joint degenerates.22 The term bipolar refers to two separate snap-fit components of one femoral prosthetic unit. A bipolar prosthesis is usually a large-diameter femoral head component that snap-fits snugly onto a smaller diameter femoral head, which is part of the total prosthetic unit.9,15 A unipolar femoral prosthesis is a self-contained femoral head and shaft without additional components. The bipolar prosthesis usually produces less wear caused by friction and reduced impact loading of the acetabulum.20
FIXATION OF PROSTHETIC HIP COMPONENTS
As discussed in Chapter 9, the method of fixation of various prosthetic components directly affects the short- and long-term course of rehabilitation after hip arthroplasty. Both femoral and acetabular components usually can be secured to the bone with a cement, polymethylmethacrylate (PMMA), which is not actually an adhesive, but rather provides a strong interference fit between the prosthesis and the bone.20 Or the components can be secured with a noncemented biologic tissue ingrowth prosthesis. Miller22 recommends that cemented femoral stems be used only for patients older than 65 years of age, and that noncemented prostheses be used for younger patients. Weight-bearing precautions are related to the specific type of fixation procedure used to secure the prosthesis. Weight bearing generally is deferred for longer periods of time with a noncemented biologic tissue fit prosthesis so that the bone can grow into the porous coated femoral stem. Weight bearing with cemented devices can progress at a slightly faster rate. However, in either case, rotational forces (torque) must be strictly avoided to minimize the loosening of components.
TOTAL HIP REPLACEMENT
 Osteoarthritis (both femoral head and acetabulum)
Osteoarthritis (both femoral head and acetabulum)
 Juvenile rheumatoid arthritis (the most common indication for THR in adolescents)20
Juvenile rheumatoid arthritis (the most common indication for THR in adolescents)20
 Significant alterations in activities of daily living (ADLs)22
Significant alterations in activities of daily living (ADLs)22
Surgeons must select a proper femoral head size for each patient. In theory, a large-diameter femoral head may provide for greater ROM and inherent stability.20,22 This makes sense because greater forces are necessary to dislocate a large-diameter head from the acetabulum. In practice, large-diameter femoral head components do not reduce the incidence of dislocation after surgery. Therefore the most commonly used head size is moderate (26 to 28 mm) rather than overly large (32 mm).20,22
One of the most common complications related to THR, using a noncemented femoral stem component, is persistent thigh pain with an antalgic gait (painful limp-gait) pattern. This thigh pain may last for 1 or 2 years after surgery and is reported in approximately 20% of all patients with this fixation type.20,22
The most significant complication after THR, with the highest mortality, is thromboembolic disease.20 The entire rehabilitation team (PT, PTA, physician, etc.) must be concerned with this complication and monitor for this continually. While many of the signs of thromboembolitic disease after THR are the same as with any other lower extremity injury or surgery, some specific signs post THR would be localized tenderness and swelling along the distribution of the deep venous system of the hip, specifically the femoral vein along the anterior thigh.
Because the method of fixation is directly related to the initiation and progression of weight bearing after surgery with uncemented components, some authorities recommend TDWB on the second day postoperatively, gradually progressing to FWB by 8 weeks postoperatively.9 With a cemented (PMMA) prosthesis, Goldstein9 suggests TDWB 2 days after surgery, progressing to FWB by the third week postoperatively. These timetables for weight bearing are directed by the biologic rate of bone healing and the wishes of the physician and are applied under the direction of the PT. A cemented component generally allows earlier motion and weight bearing than an uncemented prosthesis.
Loosening of the components has been estimated at 10% to 40% by 10 years postoperatively.22 Loosening is more common among younger, more active patients, obese patients, patients with rheumatoid arthritis, and patients with previous hip surgery.22 The PTA must be acutely aware of these factors when treating THR patients and recognize the increased potential for component loosening.
Postoperative dislocation of the hip after THR is another clinically significant complication occurring at rates between 1% and 4%.22 These dislocations are multifactorial, requiring an awareness of the basic concepts of hardware design, fixation procedures, and surgical approaches and patient compliance with specific total hip precautions to avoid dislocation. The most immediate concern during the recovery from THR is teaching and reinforcing precautions to the patient, nursing staff, family, and other caregivers.
 Avoid hip adduction. This is usually accomplished by using an abduction wedge or pillow.
Avoid hip adduction. This is usually accomplished by using an abduction wedge or pillow.
 Avoid hip internal rotation. The affected limb can be supported medially with pillows or a wedge to maintain the limb in neutral or slight external rotation.
Avoid hip internal rotation. The affected limb can be supported medially with pillows or a wedge to maintain the limb in neutral or slight external rotation.
 Avoid hip flexion greater than 90°.
Avoid hip flexion greater than 90°.
 Avoid the combination (simultaneous performance) of hip flexion, internal rotation, and adduction for up to 4 months after surgery.9
Avoid the combination (simultaneous performance) of hip flexion, internal rotation, and adduction for up to 4 months after surgery.9
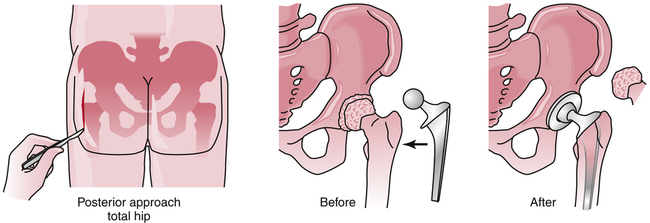
The preceding precautions apply when a posterior (Fig. 19-8), posterolateral, or lateral approach is used. If an anterior surgical approach is used, combined hip extension and external rotation should be avoided.9 Again, this variation is needed because the surgeon had to extend and externally rotate the limb to dislocate the hip and gain exposure for replacement.