23
Orthopedic Management of the Wrist and Hand
1. Identify and describe a common compression neuropathy of the wrist.
2. Discuss methods of management and rehabilitation of compression neuropathy of the wrist.
3. Identify and describe common ligament injuries of the wrist.
4. Describe and discuss methods of management and rehabilitation of ligament injuries of the wrist.
5. Describe methods of management and rehabilitation for distal radial and ulnar fractures.
6. Identify methods of management and rehabilitation for scaphoid fractures.
7. Identify and describe common metacarpal and phalanx fractures and methods of management and rehabilitation.
8. Describe methods of management and rehabilitation following surgery for Dupuytren’s disease.
9. Identify and describe common extensor and flexor tendon injuries.
10. Discuss methods of management and rehabilitation of extensor tendon and flexor tendon injuries.
11. Identify methods of management and rehabilitation for complex regional pain syndrome.
BONY INJURIES OF THE WRIST AND HAND
1. The number of fragments in the fracture
2. The fragment orientation (displaced or in alignment)
3. The approach used to restore anatomic alignment (closed reduction or open reduction)
4. The method used to maintain the reduction (external fixation: casts, splints; internal fixation: pins, screws, or plates; or percutaneous fixation: pins that protrude through the skin into the bone)
Distal Radial and Ulnar Fractures
Radius
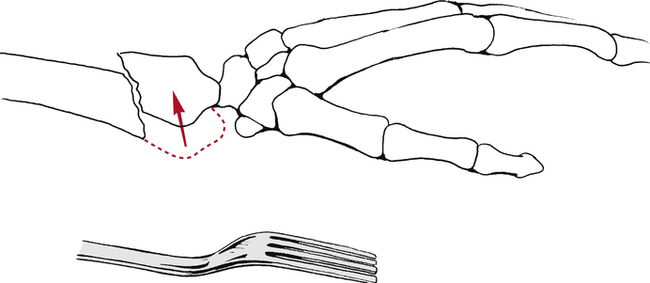
The most common distal radius fractures are Colles fractures.10 A Colles’ fracture is defined as a radius fracture within 2.5 cm of the wrist in which the distal fragment is displaced in a dorsal direction.10 This is also known as a dinner fork deformity due to the resemblance resulting from the shape of the wrist and hand following this fracture (Fig. 23-1). This injury is usually the result of a fall on the palm of an outstretched hand. Treatment of these common fractures is controversial and more than 85% require reduction.10
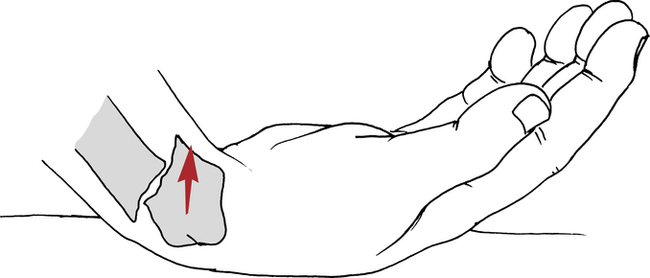
A Smith fracture is also referred to as a reverse Colles fracture.10 The fracture usually occurs from a fall on the dorsum of the hand, with the resultant distal radial fragment displaced in a palmar direction (Fig. 23-2). The course of treatment is similar to the Colles fracture and the rehabilitation is the same.
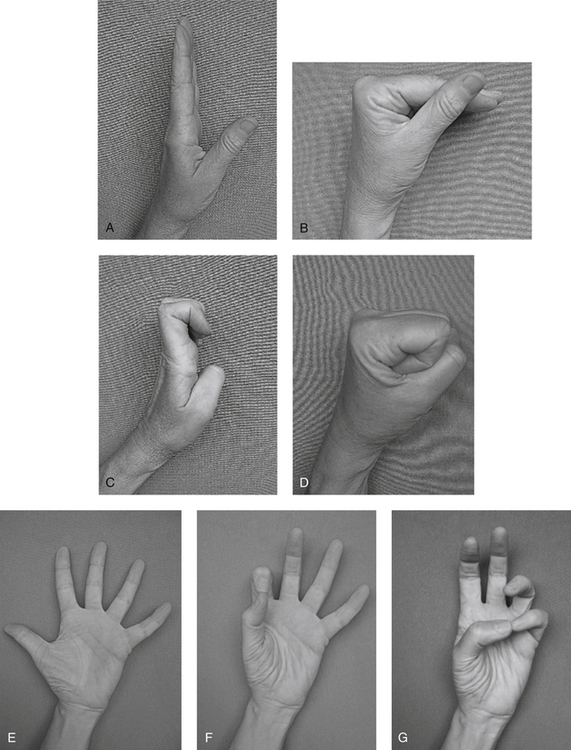
Rehabilitation starts as soon as stable immobilization has been achieved. The goals are to reduce edema through positioning and retrograde massage and to maintain digit ROM through exercise. The distal edge of the cast or splint must be proximal to the distal palmar crease in order to allow full flexion of the metacarpal phalangeal (MP) joints. “Six-pack” exercises are taught and performed hourly while awake (Fig. 23-3).6 These exercises maintain MP and interphalangeal (IP) ligament length and encourage differential gliding of the finger and wrist tendons. Passive assistance may be needed to achieve full range. Light gripping, pinching, and using the fingers is encouraged as long as there is no pain at the fracture site. Active forearm rotation within the limit of the cast should also be started. Shoulder pain should be evaluated further by the PT as proximal injuries can be overlooked in light of the distal radius fracture.
Some distal radius fractures require immobilization of the elbow to prevent forearm rotation for the first 3 weeks.26 Once the cast is modified to free the elbow, active and passive exercise to the elbow can begin. The PT should be consulted before beginning resisted elbow flexion because of the attachment of the brachioradialis on the radial styloid. Strong contractions of this muscle may cause a loss of the fracture reduction.26 Complications following distal radial fractures include: loss of reduction of the fracture fragments, nonunion (the break does not heal), malunion (partial healing or poor alignment), tendon adhesions, median nerve compression, instability, Volkmann ischemic contracture, and complex regional pain syndrome (CRPS).10 The patient’s pain, circulation and sensation should be monitored during each session and the exercises should be adjusted accordingly.
When the cast is discontinued, the patient may be placed in a soft splint between exercise sessions until the wrist muscles are stronger. Active and active assisted ROM to the wrist and forearm are initiated, making sure combinations of motion, such as flexion and ulnar deviation, are performed. Patients should be taught to isolate the wrist muscles from the finger muscles as they will have a tendency to lead wrist motion with the finger muscles. Encouraging the patient to hold a paper towel core while moving the wrist helps to accomplish this without adding resistance. Submaximal isometric exercises at various positions in the range are also started. Modalities to increase tissue extensibility or relieve pain are initiated as long as edema remains controlled. Strengthening is usually started 4 to 5 weeks after cast removal. The physician will order this only if the fracture site is no longer tender to palpation and evidence of bony union is seen. Closed-chain weight bearing is also gradually started at this time. Joint mobilization can be helpful in regaining full ROM. Patients generally return to work without restrictions about 10 weeks after cast removal.26
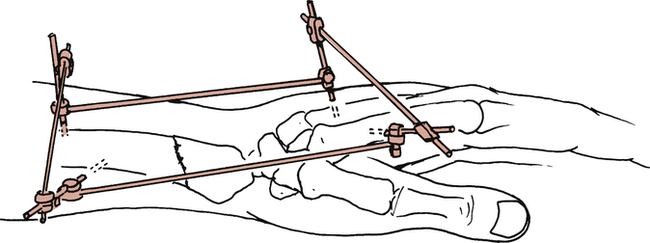
Patients with percutaneous fixation (sometimes called external fixators) can often follow the same exercise program outlined earlier (Fig. 23-4). The fixator stays in place until radiographs reveal evidence of bony healing, generally in 6 weeks.6
Distal Ulna Fractures
Fractures of the distal ulna usually occur in combination with distal radius fractures.20 The medical management and rehabilitation follow the guidelines outlined above. Persistent pain with rotation or weight bearing suggests further evaluation of the triangular fibrocartilage complex is necessary to rule out tears (see later discussion).
Scaphoid Fractures
A scaphoid fracture is often the result of a minor fall on the palm with the wrist hyperextended and radially deviated.1 It is often dismissed as a sprain, delaying treatment. Pain and swelling in the area of the anatomic snuffbox that do not resolve over a few weeks, pain with wrist extension, and decreased grip strength are signs indicating further evaluation is needed.
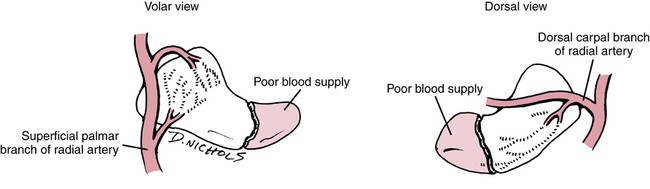
The location of the fracture within the scaphoid determines the method of treatment. The blood supply to this bone enters distally, leaving the proximal portion without direct circulation when it is separated by a fracture (Fig. 23-5). Fractures in the proximal third of the bone have a high incidence of nonunion, and those that do heal take much longer, anywhere from 12 to 24 weeks of immobilization compared with 5 to 6 weeks for the distal portion.1,4 Fractures that are not displaced or can easily be reduced are immobilized in a thumb spica cast. Nonreducible fractures require internal fixation with rigid immobilization. If nonunion and avascular necrosis (AVN) occur, bone grafts from the distal radius may be necessary.4
Rehabilitation should begin during immobilization as described under distal radial fractures. Edema reduction and ROM of the uninvolved distal joints are the primary focus. Following cast removal, the patient usually wears a thumb spica splint between exercise sessions. Wrist exercises should focus on differential gliding of the wrist and finger muscles. Strengthening with exercise putty, sustained grip activities, and gradual closed-chain activities progress to tolerance. Patients usually return to full activity within 12 weeks after cast removal.4 If the patient is having difficulty regaining motion, static progressive splinting, dynamic splinting, and joint mobilization can help restore full range.
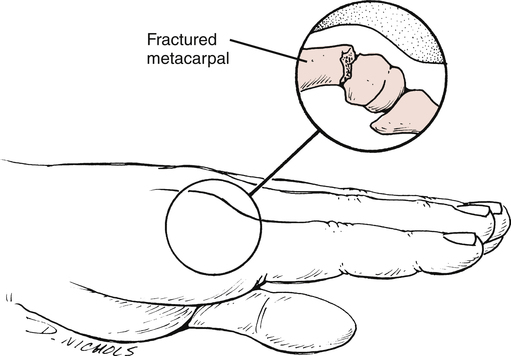
Metacarpal Fractures
Fractures of the metacarpals can occur in the base, shaft, neck, or head. These are due to falls, jammed fingers, or direct blows.29 Fractures that are nondisplaced or minimally displaced are placed in a cast or splint for 3 to 4 weeks, usually including the joint above and the joint below the fracture.30 The MP joint is placed in 45° to 60° of flexion to prevent collateral ligament shortening. Displaced fractures require surgical intervention and fixation by open or percutaneous techniques.
Fractures of the neck of the fourth or fifth metacarpal are called boxer’s fractures (Fig. 23-6). These occur when the patient strikes a hard object with a clenched fist. Ironically, these are rarely seen in professional boxers.30 These patients are immobilized with the wrist in slight extension and the MP joint flexed for 3 to 4 weeks.29,30 The proximal interphalangeal (PIP) joints are free to flex and extend often within 24 hours. Edema control sometimes requires the use of an isotoner glove as well as massage and elevation.
Active range of motion (AROM) should emphasize isolated extensor digitorum communis motion, MP flexion, and composite flexion. Tendon adhesions to the fracture site or, in the case of open procedures, the skin, often limit gliding of the extensor tendons. A splint should be worn in between exercise sessions for an additional 2 weeks. At 6 weeks, passive ROM and resistance can be started emphasizing interossei strengthening in order to achieve full IP extension.19 If the fixation is less stable, ROM may be delayed until 3 to 4 weeks, then follow the course outlined previously. When the incision has healed, scar mobilization techniques should be started.
Bennett fracture is a fracture of the palmar base of the proximal first metacarpal.30 The ligaments hold the fragment in place, but the remainder of the base is pulled radially and dorsally, resulting in a fracture-dislocation.30 As with a boxer’s fracture, treatment can be with closed reduction and rigid cast immobilization or with an open reduction with internal fixation (ORIF) procedure, depending on the severity of the fracture. There must be nondisplaced solid union at the fracture site before active motion can begin. If closed reduction is used, immobilization lasts 6 weeks to promote stable union.30 If an ORIF procedure is used, immobilization is slightly shorter because of the rigid internal fixation. Rehabilitation closely parallels the treatment for a boxer’s fracture with emphasis on regaining the thumb web space, opposition and composite flexion and extension. Resisted exercise, pinch, grip, and weight bearing on the palm with the thumb abducted can progress when stable fracture healing has occurred.
Phalanx Fractures
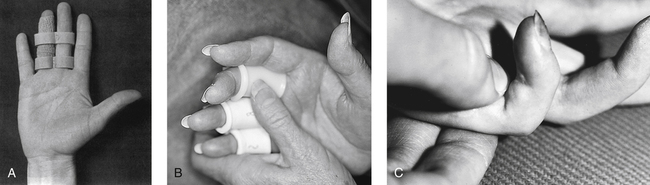
Phalanx fractures can occur at the neck, shaft, or base of the phalanx. Stable, closed, nondisplaced fractures are treated by buddy taping (Fig. 23-7, A) or with simple splints and immediate active ROM. More complex closed proximal and middle phalanx fractures should be placed in a hand-based splint for 3 to 4 weeks.24 This splint should hold the MP joints in 50° to 70° flexion and the IP joints in 10° to 15° of flexion.24 Once radiographic evidence of healing is confirmed, ROM can progress. The most common complication is loss of PIP joint extension.9 Blocking exercises can help prevent the tendons from adhering to the fracture site (Fig. 23-7, B, C).
The distal phalanx is the most frequently fractured bone in the hand.21 These fractures are usually splinted in extension using a small aluminum splint leaving the PIP joint free. Isolated PIP motion and MP motion can be started immediately. Often the nail bed is injured, leaving the finger hypersensitive and stiff. These patients are started on a program of desensitization, using touching, tapping, fluidotherapy, and vibration to overcome the hypersensitivity. Once movement can begin at the distal interphalangeal (DIP) joint, (usually at 3 weeks), the emphasis is on composite digit flexion and coordinated use of the digits. Patients often bypass the injured digit in functional activities, so this is addressed in therapy with buddy taping, light grasping, and pinching exercises that isolate the thumb and the involved finger. If the terminal extensor tendon is disrupted (see “Mallet Finger” section), the DIP joint is splinted for 6 to 8 weeks. Aggressive passive flexion should be avoided because it may lead to an extensor lag.21
SOFT TISSUE INJURIES OF THE WRIST AND HAND
Ligament Injuries of the Wrist
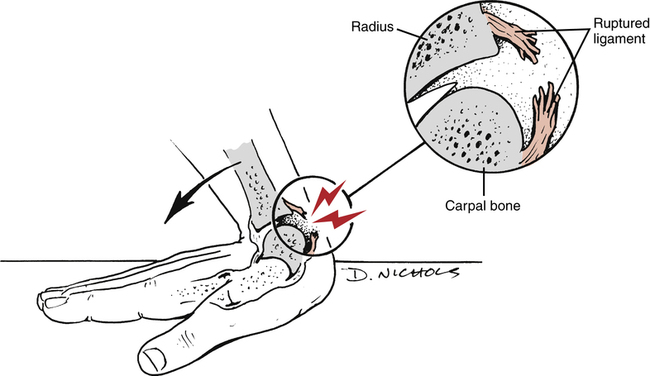
Stability of the wrist depends primarily on intracapsular ligaments and not on intrinsic dynamic support from musculotendinous tissue.34 Ligament sprains with varying degrees of carpal instability usually result from a fall with the wrist hyperextended (Fig. 23-8).34
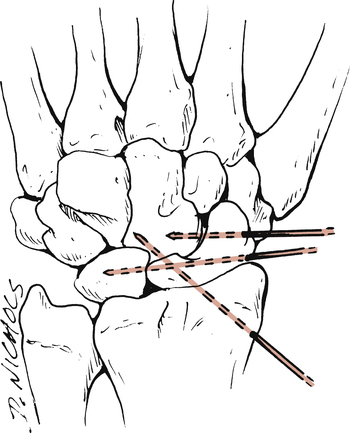
Partial ligament injuries without carpal instability are immobilized in a short arm cast or splint for 3 to 4 weeks. Severe ligament injuries lead to carpal instability and reduction and maintenance of the alignment are more difficult. Options include rigid cast immobilization, closed reduction with percutaneous pinning, and ORIF (Fig. 23-9).34 If cast immobilization is used to stabilize the joint, the patient is placed in the cast for 6 to 12 weeks, depending on the severity of the injury.34 If closed reduction and internal fixation is required, the wrist is immobilized for about 2 months. After two months, the pins are removed, and the arm is placed in a cast for an additional 4 weeks.34 With an ORIF procedure, the ligaments are directly repaired and the unstable carpal articulations are stabilized with wires or pins. The duration of immobilization is similar to that for closed reduction with percutaneous pinning.34
Regardless of the severity of the injury, the principles for rehabilitation are the same.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree