20
Orthopedic Management of the Lumbar, Thoracic, and Cervical Spine
Cheryl Sparks, Joseph Kelly and Gary A. Shankman
1. Outline and describe basic mechanics of the lumbar spine.
2. Discuss and apply the principles of fundamental mechanics of lifting.
3. Identify common sprains and strains of the lumbar spine.
4. Discuss common methods of management and rehabilitation of lumbar spine sprains and strains.
5. Identify and describe injuries to the lumbar intervertebral disc.
6. Define and describe methods of quantifying back strength.
7. Define and describe components of the back school model.
8. Define ergonomic and functional capacity evaluations.
9. Define spinal stenosis and describe methods of management and rehabilitation.
10. Define and contrast the terms spondylolysis and spondylolisthesis.
11. Describe methods of management and rehabilitation for spondylolysis and spondylolisthesis.
12. Identify common lumbar and thoracic spine fractures.
13. Define kyphosis, lordosis, and scoliosis.
14. Identify and describe methods of management and rehabilitation for kyphosis and scoliosis.
15. Identify and describe common cervical spine injuries, and discuss methods of management and rehabilitation.
In an age when health care expenditures are a concern for many, back pain continues to cost billions of dollars in intervention and lost labor.42,45 It is imperative that the physical therapist assistant (PTA) possess a sound understanding of the anatomy and appropriate management of patients with various spinal disorders. In this chapter the PTA is introduced to overall symptomatology and effective intervention strategies for some of the more prevalent diagnoses affecting the spine.
THE LUMBAR SPINE
Perhaps no other medical condition draws as much attention from researchers and clinicians as the identification and management of lumbar spine injuries. The primary cause of disability in the middle-aged working class adult is related to low back pain and accounts for approximately $50 billion in health care costs annually in the United States.26,42,45 Lumbar spine injuries are also to blame for literally millions of lost work days per year in the United States and internationally. The rate of disability from injuries to the low back was estimated over a 10-year period to be a staggering 14 times greater than the rate of population growth for that same period.1,15 Overall, lumbar spine injuries are the second leading cause of all physician visits in the United States and the prevalence of low back pain in the population is close to that of the common cold.1,5,8,16,17,42
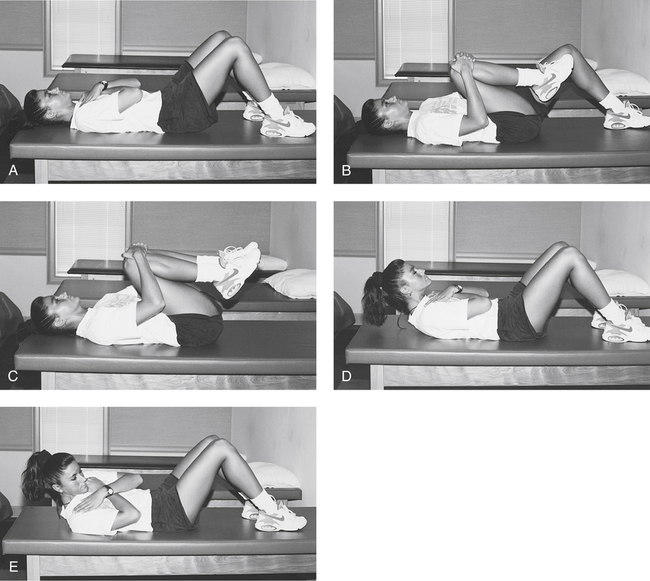
Historically, absolute bed rest, medications, thermal agents (e.g., hot packs or ultrasound), and a series of rudimentary lumbar flexion exercises (e.g., pelvic tilts, single knee-to-chest, double knee-to-chest, and partial direct and oblique sit-ups) (Fig. 20-1) were the components of a typical protocol for lumbar sprains, strains, and disc-related pathologic conditions. It is now widely accepted that active rest and resumption of function has a significant impact on improving long-term outcomes.20,24
Basic Mechanics
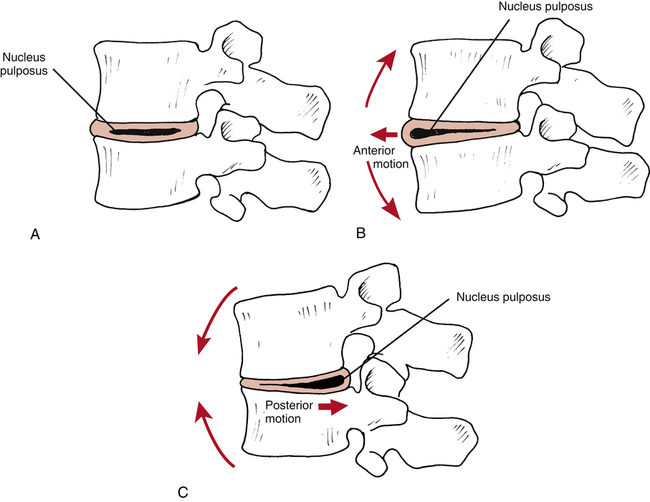
In the adult spine there are 23 intervertebral discs found in between the vertebral bodies (Fig. 20-2). The outer wall of the disc is called the annulus and comprises 12 to 18 concentrically arranged rings of fibroelastic cartilage.30,56 Contained within the annulus is the nucleus pulposus. Nuclear material is a mucopolysaccharide gel30 that transmits forces, equalizes stress, and promotes movement.55 The annulus provides stability, enhanced movement between vertebral bodies, and minimal shock absorption. The greater portion of shock absorption comes from the vertebral body.56,65
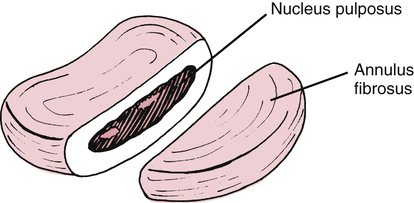
The intervertebral disc is largely avascular and aneural. The vascular supply to the disc is provided by diffusion from the vertebral bodies above and below the disc.14,30,49,56 The outer one third of the annulus is said to be innervated along with the facet joint capsule and exiting nerve roots.14 When injured, without an intense vascular response, the disc has a limited capacity to heal and repair. In addition, degenerative changes also occur within the disc as a normal process of aging throughout the life span.
A popular theoretical model describes the fluid mechanics of the disc (nucleus pulposus) influenced by the motion of the lumbar vertebral segments. McKenzie49 describes flexion and extension motion of the spine as having clinically significant effects on the nucleus’s direction of movement (Fig. 20-3, A). The theoretical model proposes when positional changes occur in the lumbar spine, from flexion to extension, the nucleus moves anteriorly (Fig. 20-3, B).49 Conversely, when the spine moves from extension to full flexion, the nucleus tends to displace or move posteriorly (Fig. 20-3, C). Thus it is necessary to fully understand the individual nature of each injury and avoid or enhance certain motions and postures as directed by the physical therapist (PT).
The lumbar spine is composed of five anterior convex and posterior concave segments that produce the recognizable lordotic curve. Normal lordosis is increased with spinal extension and reduced with spinal flexion. The lumbar spine serves to support the weight of the upper body and dissipate compressive loads with minimal production of muscular torque. As a result significant forces are transmitted through the intervertebral disc during certain motions. Allman1 describes lumbar motion and postural alterations as producing significant pressure within the disc (intradiscal pressure). The compressive forces that influence intradiscal pressure are as follows1:
 Standing: Disc pressure is equal to 100% of body weight
Standing: Disc pressure is equal to 100% of body weight
 Supine: Disc pressure is less than 25% of body weight
Supine: Disc pressure is less than 25% of body weight
 Side-lying: Disc pressure is less than 75% of body weight
Side-lying: Disc pressure is less than 75% of body weight
 Standing and bending forward: Disc pressure is approximately 150% of body weight
Standing and bending forward: Disc pressure is approximately 150% of body weight
 Supine with both knees flexed: Disc pressure is less than 35% of body weight
Supine with both knees flexed: Disc pressure is less than 35% of body weight
 Seated in a flexed position: Disc pressure is approximately 85% of body weight
Seated in a flexed position: Disc pressure is approximately 85% of body weight
 Bending forward in a flexed posture and lifting: Disc pressure is close to 275% of body weight
Bending forward in a flexed posture and lifting: Disc pressure is close to 275% of body weight
Intradiscal pressure also can be expressed in terms of pressure or load measured within the intervertebral lumbar disc. Cailliet9 reports that isometric abdominal sets produce approximately 110 kg of pressure within the disc, whereas walking produces 85 kg; sitting, 100 kg; bilateral straight-leg raises in supine position, 120 kg; and lifting with a flexed torso and knees held straight, an astounding 340 kg of intradiscal pressure. This information may help clarify the rationale for protective postures, lifting protocols, and appropriate body mechanics, as well as prescribed exercises for specific lumbar spine conditions.
Muscle Strains
Although some authorities27 point out that most low–back–related dysfunction results from soft-tissue injury, it is important to note that many other structures can potentially be involved (ligaments, disc, nerve tissue, and bone) and often the exact pathoanatomic cause of pain is elusive. The function however of the lumbar spine musculature is to contribute to dynamic stability.55 Panjabi and co-workers55 have identified the need for specific low back strengthening to reduce injury and “to stabilize the spine within its normal physiologic motions.”
Muscle strains of the lumbar spine are common and general treatment goals are as follows62: reduce or eliminate inflammation (pain and swelling), restore muscle strength and control, restore flexibility, enhance cardiorespiratory fitness, restore function, and protect the affected area from further injury through education and supervised practice of proper lifting mechanics.
Ligament Sprains
These spinal ligaments69 can be injured by a sudden violent force or from repeated stress. The PT conducts a comprehensive examination of the patient to confirm or deny the presence of segmental instability (hypermobility resulting from ligament sprain) and evaluate the degree of pain with or without active or passive movement of the lumbar spine in general or in individual segments.1,5 In addition to isolated ligament sprains, muscle strains can be superimposed, making the identification of specific single-ligament sprains exceedingly difficult. The management of lumbar ligament sprains essentially parallels the care of muscle strains. Each patient has specific, identified impairments and goals that must be addressed individually through the initial evaluation performed by the PT. The PTA, under the direction of the PT, must identify which specific positions are contraindicated by carefully reviewing the initial evaluation data. Both the short- and the long-range goals for recovery from lumbar strains and sprains emphasize protecting the spine from unwanted forces and positions.
Radiculopathy
Radiating pain into one or both lower extremities could signify nerve root compression from an adjacent herniated intervertebral disc. A sensitive test for nerve root compression or disc herniation requires the patient to be supine while the symptomatic leg is raised passively with the knee completely extended. This is called a straight leg raise test. When the uninvolved, or asymptomatic, lower extremity is tested in the same manner, this is called a crossed straight leg raise test. The crossed straight leg raise has been found to be highly specific for disc herniation. These tests are considered positive only if radicular pain is increased or reproduced.21 Any positive findings noted during the initial examination performed by the PT should be confirmed or denied.62
Lumbar Intervertebral Disc Pathologies
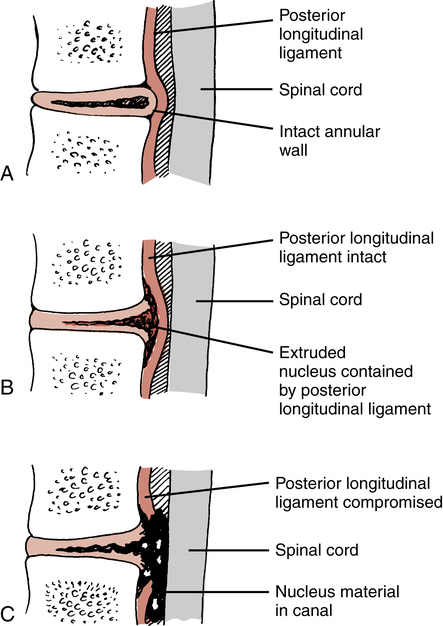
Various terms are used to describe injuries to the disc. Although “slipped disc” is a common expression used to describe various ailments of the low back among the general population, a disc does not “slip” from within its confines between the vertebral bodies. Also incorrectly applied are the two terms, disc bulge and herniated nucleus pulposus (HNP). These are frequently used interchangeably. To clarify, a HNP can be defined by specific nomenclature to more precisely describe the injury. Miller51 describes the three categories of HNP as protruded, extruded, and sequestrated. In a disc protrusion, the nucleus bulges against an intact annulus (Fig. 20-4, A). This would more closely resemble the layperson’s disc bulge terminology. An extruded disc is characterized by the nucleus extending through the annulus, but the nuclear material remains confined by the posterior longitudinal ligament (Fig. 20-4, B). Finally, in a sequestrated disc, the nucleus is free within the canal (Fig. 20-4, C).
Macnab46 offers a variation of this classification model:
Regardless of the exact nature of the injury, a HNP remains primarily a disease of young to middle-aged adults.51 Common age-related degenerative changes that occur within the disc include decreased hydration, with a decreased water content from 70% to 88% by the third decade; biochemical changes in the glycosaminoglycans of the nucleus; and increases in collagen. As a result these changes make disc herniations rare in elderly people.51,56
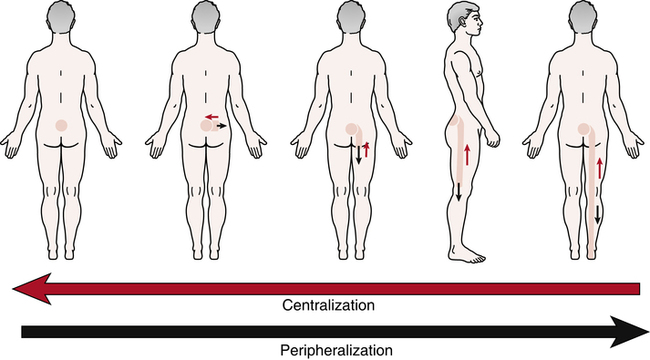
When examining a patient who exhibits radicular signs, the PT confirms or denies the presence of peripheralization or centralization phenomena by observing a directional preference.41,49 These conditions identified during the initial examination are defined by Kisner and Colby41 as follows: “When repeating the forward-bending test, the symptoms increase or peripheralize. Peripheralization means the symptoms are experienced further down the leg.” Centralization is defined by McKenzie49 as, “the phenomenon whereby, as a result of the performance of certain repeated movements or the adoption of certain positions, radiating pain originating from the spine and referred distally, is made to move away from the periphery and toward the mid-line of the spine” (Fig. 20-5). The evaluation data obtained by the PT regarding the presence of a directional preference is essential in determining treatment.
Spondylolysis and Spondylolisthesis
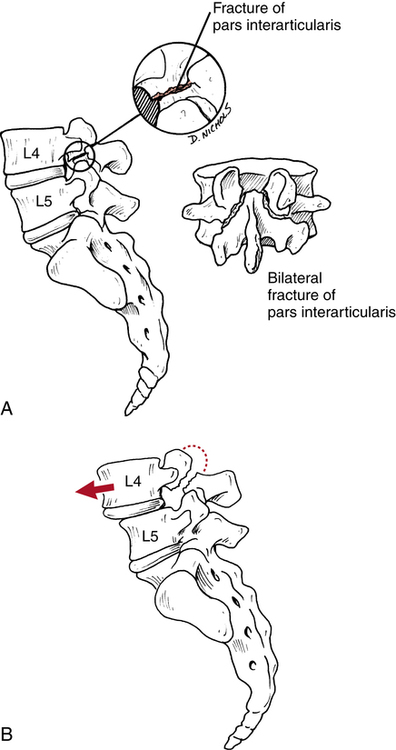
Spondylolysis is a bony defect (stress fracture or fracture) in the pars interarticularis of the posterior elements of the spine (Fig. 20-6, A).8,9,15,21,51,56,62 Spondylolisthesis, on the other hand, describes a forward slippage of one superior vertebra over an inferior vertebra (usually L4-L5 and L5-S1)18,21 as a result of instability caused by the bilateral defect in the pars interarticularis (Fig. 20-6, B).8,9,15,21,51,56,62 There are specific classification types, as well as degrees of slippage or “migration” of the vertebrae in the disease process of spondylolisthesis.21 Five types, or classifications, have been identified, as follows8,21,51:
 Type I: Congenital or dysplastic. Results from a “congenital malformation of the sacrum or neural arch of L5, which allows forward slippage of L5 on the sacrum.”8 Most common in children.
Type I: Congenital or dysplastic. Results from a “congenital malformation of the sacrum or neural arch of L5, which allows forward slippage of L5 on the sacrum.”8 Most common in children.
 Type II: Isthmic spondylolisthesis. The most common type, affecting persons 5 to 50 years of age.51 Usually a result of mechanical stress that causes a stress fracture at the pars interarticularis.21,51
Type II: Isthmic spondylolisthesis. The most common type, affecting persons 5 to 50 years of age.51 Usually a result of mechanical stress that causes a stress fracture at the pars interarticularis.21,51
 Type III: Degenerative spondylolisthesis. Most commonly affects the older population. Characterized by a loss of ligament integrity (or stability) that results in forward slippage of the vertebrae. Generally associated with the normal aging process.8
Type III: Degenerative spondylolisthesis. Most commonly affects the older population. Characterized by a loss of ligament integrity (or stability) that results in forward slippage of the vertebrae. Generally associated with the normal aging process.8
 Type IV: Traumatic spondylolisthesis. Caused by trauma that produces an acute fracture of the pars interarticularis. Casting is the most appropriate form of treatment.8 Because of their generally high levels of physical activity, this type usually affects young patients.51
Type IV: Traumatic spondylolisthesis. Caused by trauma that produces an acute fracture of the pars interarticularis. Casting is the most appropriate form of treatment.8 Because of their generally high levels of physical activity, this type usually affects young patients.51
 Type V: Pathologic spondylolisthesis. Characterized by bone tumors that affect the pars interarticularis.
Type V: Pathologic spondylolisthesis. Characterized by bone tumors that affect the pars interarticularis.
The degree or grade of slippage is determined radiographically by the examining physician and is defined as the amount of forward displacement of the superior vertebrae over the inferior vertebrae, as outlined in the following:8,15,51
The cause of the defect in the pars interarticularis is in part a congenital weakness in this area. In addition, the pars interarticularis is subjected to high levels of mechanical stress.64,65 Authorities also suggest that the primary initial cause of the most common type of spondylolisthesis (isthmic) is fatigue fracture of the pars interarticularis.65
Patients primarily report pain with extremes of lumbar motion, especially extension. The pain generally follows the belt line.37 During examination, the PT also may identify a palpable step-off between the affected lumbar vertebrae (usually L4-L5) because of the forward slippage.15
The patient may require more specific attention when there is a greater degree of slippage with significant symptoms. Generally, pain and muscle spasm are addressed with physician-prescribed analgesics, muscle relaxants, nonsteroidal antiinflammatory drugs (NSAIDs), and agents (heat, ice, ultrasound, and electrical stimulation) to alleviate acute pain and swelling. If the pain is related to a fatigue fracture of the pars interarticularis, initial treatment focuses on managing stress to the fracture site using a lumbosacral corset or orthosis, which reduces anterior shearing forces through the fracture site and allows for bone healing.21,37
The cornerstone in the care of spondylolisthesis is application of abdominal and paravertebral muscle strengthening exercises to provide dynamic support for the spine during activity and avoidance of extreme lumbar extension. A young active patient must modify activities that directly influence the course of this disease. For example, weight lifting without proper precaution can contribute significantly to the occurrence of spondylolysis.19
Surgery is rare and usually is reserved for patients with radicular symptoms and high-grade slippage (grades III or IV), which compresses the nerve roots and causes neurologic signs.8,51 The type of surgery advocated in these cases is a decompression laminectomy (to reduce compression of the nerve roots) with fusion to stabilize the vertebral segments.8,51
Rehabilitation after surgery for spondylolisthesis is deferred until solid bony union is determined radiographically. The patient is usually in a lumbosacral orthosis that does not permit lumbar extension. During immobilization, the patient can ambulate as tolerated and perform rudimentary ROM and strengthening exercises for the upper and lower extremities (ankle pumps, quadriceps sets, and knee ROM). Once bone healing is confirmed, a gradually progressive program of abdominal strengthening (from isometrics to concentric and eccentric abdominal contractions), lumbar ROM (avoiding dynamic, ballistic, and extreme lumbar extension), general conditioning, and a progressive return to function is advocated.8,51
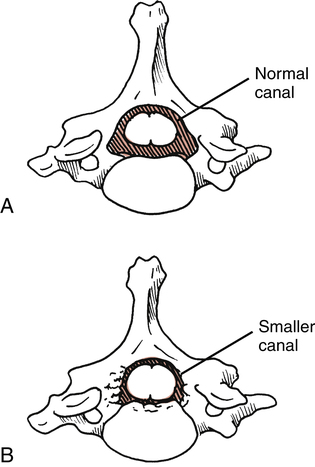
Spinal Stenosis
Lumbar spinal stenosis is defined as a narrowing of the spinal canal, which constricts and compresses nerve roots (Fig. 20-7).51 This gives rise to symptoms of neurogenic or spinal claudication, as follows:
1. Radicular ache into the thigh and less frequently into the calf8
2. Paresthesias into the lower extremity29
This condition occurs in males “twice as often as females”51 and typically is observed during late middle age and older.29,51
Lumbar spinal stenosis is most commonly acquired as a result of degenerative arthritic changes that encroach on the diameter of the canal, producing nerve root compression.51 The patient with stenosis frequently complains of pain and increased symptoms with lumbar extension. Extension of the lumbar spine in a patient with stenosis further compresses the spinal canal, thereby increasing pain and paresthesias.15,29,51
During ambulation and gait training, an elderly patient typically demonstrates a forward-flexed trunk posture when using a walker. Under careful observation and questioning, the patient may suggest that leaning forward feels better and reduces back and leg pain. The role of the PTA is to continually educate the patient, reinforcing appropriate postures, body mechanics, and lifting techniques. Sitting and sleeping changes, as well as a general physical conditioning and weight management programs are also addressed and have been identified as an important adjunct in the overall management of patients with spinal stenosis.51 Whitman and colleagues63 demonstrated that subjects with spinal stenosis experienced greater improvements in pain and recovery at 6 weeks with manual therapy, exercise, and walking than subjects who just performed routine flexion exercises and walking. The physical therapy team should work together to provide the appropriate manual intervention followed by specific exercise and a walking program for the best management of patients with spinal stenosis.
Lumbar Spine Fractures
Fractures of the lumbar vertebrae generally occur after a profound traumatic event and can be classified according to the forces that produce the fracture. For example, compression, flexion, extension, flexion-distraction, flexion-rotation, and lateral flexion are forces that produce fractures.51 Lumbar spine fractures also can be described in terms that graphically depict a specific fracture deformity, including crush, wedge, burst, shear, slice, and teardrop fractures.51
Perhaps the most clinically relevant spine fracture for the PTA to consider is the vertebral compression fracture. Vertebral compression fractures are the most common osteoporosis-related spinal fracture with approximately 700,000 occurring per year, and the prevalence of vertebral compression fractures increases with age.15,29,43
Many benign activities can produce compression fractures in an elderly population of patients with osteoporosis.8,43 Care must be taken to ensure that no rapid deceleration occurs when an elderly patient transfers to a bedside commode or any other hard surface. This seemingly trivial activity frequently causes multilevel compression fractures in patients with osteoporosis. Compression fractures produce symptoms ranging from acute local pain to essentially no signs at all.43 Thus subtle complaints of pain caused by typical daily activities, such as bending, lifting, or rising from a chair, must be viewed with a high level of suspicion in elderly patients.43
Treatment of compression fractures focuses on relief of pain; authorities29,43 advocate activity modification, physician-prescribed analgesics, NSAIDs, heat, ice, massage, and electrical stimulation to control pain, swelling, and associated muscle spasm. During the acute and subacute phases of recovery, the patient with compression fractures must avoid thoracic or lumbar flexion activities.29 Repeated trunk flexion is contraindicated because it creates an anterior wedging of the vertebral bodies, producing greater stress and compression at the fracture site.29Appropriate exercise progression should target the muscles supporting or attached to the affected bone, and they will be determined by the PT. Exercises should be combined with postural correction, scapular stabilization, and improving weight-bearing patterns, strength, balance, and flexibility.
Treatment-Based Classification
Rehabilitation of the lumbar spine is focused toward impairments rather than labeling pathoanatomic findings. As a result, when a patient experiences low back pain, the evaluating PT assimilates information from the patient history, examination, and current best evidence, and classifies the patient into the most appropriate category. The rehabilitation plan will include a multimodal approach that categorizes patients based on their overall symptomatology and response to a specific intervention. This system has been identified as treatment-based classification (TBC).6
The TBC system consists of subgroupings through which the patient moves fluidly in and out of during the course of care. The interventions within these categories include manual therapy and exercise,12,22 specific exercise for directional preference,7,63 traction,24,25 neuromuscular reeducation and stabilization exercise,34,52,54 aerobic exercise, and recommendations to stay active. PTs will use their findings from the clinical examination to match the patient with the most appropriate intervention. Research has shown patients managed with this systematic approach experience significant decreases in pain and disability.6,24 For the PTA it is important to be aware of the categories along with exercise and educational concerns within each.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree