Fig. 1.1
The Reeves prosthesis showing the spiked glenoid component which was cemented into the glenoid (from Professional Engineering Publishing from Reeves et al. [17])

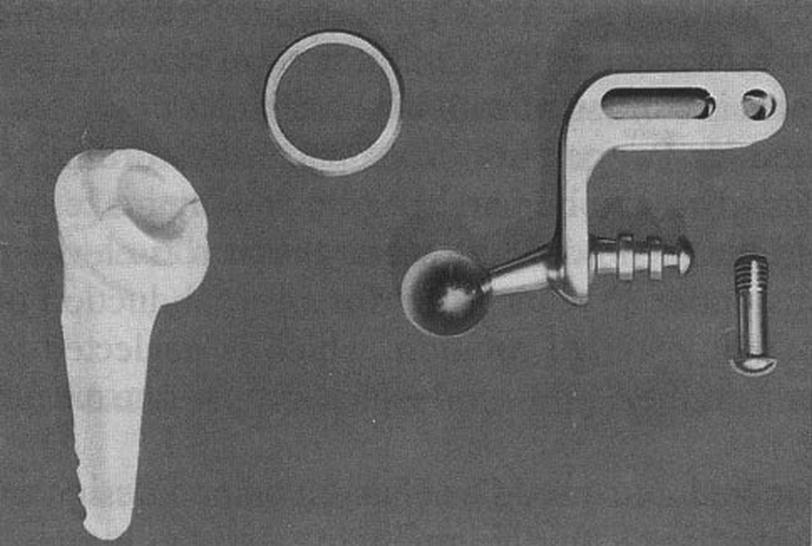
Fig. 1.2
Gerard prosthesis featuring a glenoid component that was screwed into the glenoid without cement (from Wolff and Kölbel [69]). Used with permission
1973
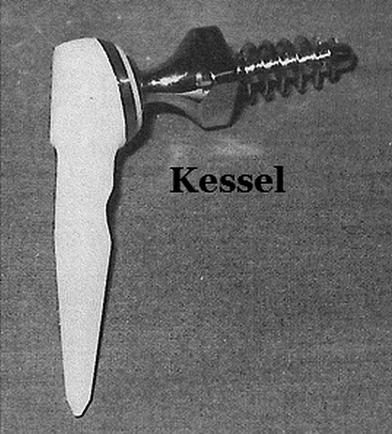
The Kessel RSA was unique from previous designs in that it was the first design to be attached to the scapula with a single large self-tapping lag screw which was used without cement (Fig. 1.4). Kessel and Bayley reported on their first series of patients in 1979 [13] but followed that up with an expansion of this series with longer follow-up in 1982 [6]. In the 1982 report of 30 patients (31 shoulders), 25 patients (26 shoulders) were satisfied with their outcome. There were 5 failures requiring removal of the device which included 3 dislocations, 1 failure to relieve pain, and one wrenched shoulder. There were no reported loosenings of the glenoid component. A later study by Brostrom et al. [21] reported on 22 patients (23 shoulders) with rheumatoid arthritis treated with the Kessel prosthesis. Six patients had failures requiring removal of their prosthesis. Two of these failures were not device related as one patient with Parkinson’s fell and fractured his scapula and another patient had a malalignment of the components which caused frequent dislocations. The other 4 failures were two patients with aseptic loosening of the scapular component, one patient with both components loose secondary to an infection, and one patient with a fatigue fracture of the scapular component. In all, there were only 3 device-related failures due to aseptic loosening or failure of the scapular component (13 %); however, all patients had a radiolucency around the scapular component although the majority were not progressive.
1975
At Thomas Jefferson University in Philadelphia, Pennsylvania, Fenlin [9] documented his design rationale and 5 clinical cases of his initial use of his RSA (Fig. 1.5). Fenlin made it clear in his design rationale that he was most concerned about the loosening of the scapular component. His idea involved designing a two-piece scapular component that could essentially fill the two cancellous cavity extensions that extend beyond the glenoid vault. One of these extensions continues irregularly up to the coracoid process and the other extends down the axillary border of the scapula. His rationale for inserting components into these cavities was that he thought they would predictably be surrounded by the most dense cortical bone in the scapula. His scapular anchor was cemented into the scapula like previous RSA designs. Fenlin went on to describe 5 difficult cases that were treated with his implant. Among them were a 44-year-old man with a Charcot shoulder, a 38-year-old woman with a shotgun wound with loss of the proximal humerus, a 70-year-old female with failed previous ORIF which went on to nonunion and avascular necrosis, a 64-year-old female with a fracture dislocation of the shoulder with 2 previous operations, and a 62-year-old woman with an old undiagnosed posterior dislocation of the shoulder. Despite the difficulties inherent in this cohort of patients, he only reported 2 complications: loosening of the scapular anchor in the Charcot shoulder and a partial nerve palsy in the fracture-dislocation patient. It is important to note that this report by Fenlin was primarily a description of his design rationale but is often quoted to support the notion that these types of implants had a high complication rate.
In England, the Liverpool shoulder, designed by Beddow and Elloy in 1975, was based on the design of the Charnley hip [7]. The authors mention that there was a metal prototype designed in 1969 but included no other information or images. Their clinical series was based on the 1975 design; therefore, I am including this implant in the 1975 section. Their design featured a glenoid component that resembled a small femoral stem that is cemented into the medullary cavity of the axillary border of the scapula. The ball of the glenoid component interfaced with a stemless polyethylene socket that was cemented into the humerus. The humeral component snapped onto the glenoid ball to add constraint to the shoulder joint. Their series of 16 patients had a complication rate of 37.5 % (6/16). Four of those patients had loosening of the scapular component although one was due to a scapula fracture as a result of a fall.
1978
The Buechel–Pappas implant was designed to keep the stability afforded by the constrained reverse geometry; however, they added a third component which was essentially a floating socket [8]. Their rationale for adding this functionality was to increase the theoretical range of motion. In their only report of this implant, the 6 patients treated with it reported good outcomes and there were no cases of loosening. This implant was also cemented to the scapula.
The final implant discussed was the trispherical total shoulder replacement designed by Gristina and Webb [12]. This implant was unique from the rest in that the humeral and glenoid components had a sphere, which were both interposed with a polyethylene sphere with a metal shell which gave it the “trispherical” name. The glenoid component was keeled and was cemented into the scapula. In their early series, 18 patients (20 shoulders) reported overall good outcomes; however, there were 4 cases of device complications with components dislocating or malfunctioning. There were no cases of loosening reported.
The overall device-related complications of these series are summarized in Table 1.1. Neer’s Mark I–III devices [16] and the Reeves device [17] are not included as they lacked a clinical series of their implants. Despite some of these reports showing few or no complications, none of these devices caught on as a viable option to treat patients with rotator cuff deficiency. The resurgence of RSA began with Grammont’s [11] work with his “Trompette” prosthesis which he designed in 1985 and later reported on in 1987 (Fig. 1.6). This design was unique in that Grammont’s desire was to medialize and lower the center of rotation (COR) relative to where it is found normally. His rationale was that this medialization would strengthen the deltoid to improve function in patients. His design utilized two-thirds of a sphere for the glenosphere with a ceramic baseplate that was cemented to the glenoid. In his first series on RSA utilizing the Trompette prosthesis, 3 of the 8 patients had elevation at 100° or higher. However, according to Baulot [22], he personally observed some loosening and made two major changes in the implant design. First, he increased the medialization by changing the 2/3 sphere to a hemisphere, putting the COR right at the glenoid surface. The second change was that he changed the glenoid component from one that required cement to a press-fit baseplate with a central peg and porous coating, along with 2 divergent transfixion screws oriented superiorly and inferiorly (Fig. 1.7). This updated design was called the “Delta III” and came onto the European market in 1991. His initial experience with this device was reported in 1993 [23] which was encouraging. This resurgence has led to numerous recent reports on the Grammont’s design that have shown its effectiveness [1, 4, 5, 24, 25]. These reports often mention the failures of the previous RSA devices and give credit to Grammont for designing an RSA device that overcame those deficiencies. These have become known as “Grammont’s principles” [22, 25].

Table 1.1
Complications of early RSA designs
Author/year | Device | # patients | Device-related complication (%) | Aseptic BP failure (%) |
|---|---|---|---|---|
Gerard 1973 | Gerard–Lannelongue | 11 | 36 | 0 |
Kölbel 1982 | Kölbel | 20 | 20 | 5 |
Bayley 1982 | Kessel | 31 | 16 | 0 |
Brostrom 1992 | Kessel | 23 | 26 | 13 |
Beddow 1982 | Liverpool | 16 | 31 | 19 |
Fenlin 1975 | Jefferson | 5 | 20 | 20 |
Buechel 1978 | Buechel–Pappas | 6 | 0 | 0 |
Gristina 1982 | Trispherical total shoulder replacement | 20 | 20 | 0 |

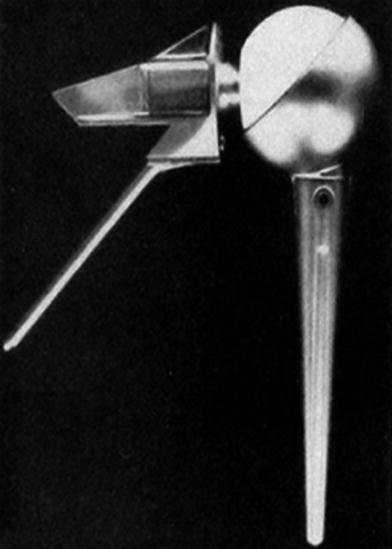
Fig. 1.7
Grammont’s Delta III showing the modifications from the Trompette prosthesis to a glenoid hemisphere and a press-fit baseplate with transfixion screws
Common Misconceptions
My interest in studying misconceptions about RSA began when I was reviewing articles on the early success of the Delta III prosthesis and how it was different than previous RSAs. When reading an article by Boulahia [24] on their clinical outcomes with the Delta III, I noticed two assertions in the discussion section that I found interesting. The first assertion was that “Earlier attempts using a reverse shoulder prosthesis design were burdened by early loosening of the glenoid component caused by a laterally offset center of rotation resulting in a rocking horse phenomenon occurring at the glenoid bone component interface (Figure 4).” No reference was provided, but as I looked into the origin of the “rocking horse” effect, it was in a study by Franklin [26] on glenoid loosening in total shoulder arthroplasty. In that study, the “rocking horse” phenomenon was only attributed to anatomic total shoulder replacements and not RSA. This is because the superiorly migrating humeral head provides an eccentric load onto the glenoid component. As I reviewed the original studies on the early RSAs, I was unable to find any reference to a rocking horse mechanism mentioned as a cause of failure [6–10, 12–18, 21]. Thus, the assertion that the lateral center of rotation resulted in a rocking horse phenomenon in RSA was unsubstantiated. The second assertion is found in the legend of Figure 4: “The laterally located center of rotation of the early reverse design prostheses caused early loosening.” Again, as I reviewed the reports on the early RSAs, I was unable to find any assertions of causality of failure nor was I able to find any biomechanical studies concluding this was a mechanism for RSA failure. This was likely due to the fact that those early studies were not designed to determine causality. According to Kooistra et al. [27], “When a study lacks a control group, no causal inferences should be made about the relationship between the treatment and the outcomes, since it is impossible to determine whether the outcomes are attributable to the treatment effect or to other patient characteristics.” Therefore, this assertion of the lateral center of rotation causing early loosening was also unsubstantiated. These unsubstantiated claims of the “rocking horse effect” and the attribution of causation of failure to lateral center of rotation were the impetus to conduct a study to understand the extent to which these assertions have been repeated unchallenged in the orthopedic literature.
The Investigation
The purpose of my study was to search all studies on RSA post-Grammont’s initial series and examine their assertions and claims regarding the experience and outcomes of the early RSA devices designed in the 1970s. A Pubmed and Embase search of published RSA studies from 1985 to 2011 was performed using the search criteria: “(shoulder* OR gleno* OR humer*) AND (revers* OR inver*) AND (arthroplast* OR prosthe* OR replacement).” The search returned 218 articles on RSA. These articles were reviewed for any mentions of the early RSA devices from the 1970s as discussed earlier in this chapter. If an article contained any mention of early RSA devices, it was included for further analysis. The included articles were examined for quotational accuracy according to the method of Evans et al. [28]. Assertions made by the current articles regarding the original RSA devices were evaluated to determine if the assertions were substantiated. A major error of quotation was assigned if the referenced article failed to substantiate, was unrelated, or contradicted the authors’ assertions. A minor error of quotation was assigned for articles that contained an oversimplification or a generalization not asserted by the original author(s) cited.
Findings
Thirty-two articles were identified as containing mentions of the original RSA designs and were included in the study [1, 3, 5, 19, 22, 24, 25, 29–53]. Twenty-four out of 32 (75 %) contained at least one quotational error. Twenty out of 32 (62.5 %) contained at least one major quotational error and 4 out of 32 (12.5 %) contained a minor quotational error. Out of the 20 papers with major quotational errors, five had 2 major errors. The most common type of major error was an assertion of causation that was not substantiated by the referenced article(s) involving the original RSA devices. I have selected several examples below to illustrate the quotational errors found. The complete analyses of errors, as well as references [54–65] specifically used by the included articles, are contained in the appendix at the end of this chapter.
Examples
1.
Boileau [25] assertion: “These previous constrained shoulder prostheses, other than the Grammont, tended to fail because their design resulted in excessive torque and shear forces at the glenoid component-bone interface.” The authors are referring to 6 references cited earlier in the text: Bayley, Brostrom, Fenlin, Gerard, Kölbel, and Neer.
Major Quotational Error 1: The assertion is unsubstantiated by the references given as none of these articles determined that failure was caused by excessive torque and sheer forces nor were they designed to do so [27]. The authors’ assertion is also not supported by all of the references. For example, two of the references, Bayley [6], Gerard et al. [10], report no aseptic baseplate loosening. Furthermore, the Fenlin reference is a design rationale paper that gives a brief summary of 5 cases with only one of the 5 patients experiencing glenoid loosening [9]. The case of loosening involved a Charcot shoulder which would be considered a contraindication to joint replacement surgery today.
Major Error 2: Unrelated reference. The Neer reference given is the classic article on cuff tear arthropathy and is not about an original RSA device.
2.
Frankle [3] assertion: “Early designs of reversed shoulder implants, however, were plagued with difficulties related to glenoid failure and soon fell out of favor [17].”
Minor Error: While the assertion that early designs were plagued with difficulties related to glenoid failure is true for some devices, it is not true for all of them so I consider this an oversimplification/generalization. In fact, while the study referenced (Brostrom [21]) had a 13 % aseptic baseplate failure rate, another study by Bayley [6] on the same implant reported no aseptic cases of loosening.
3.
Nam [40] assertion: “After its introduction in the 1970s, reverse shoulder arthroplasty had minimal clinical success, as its constrained design and lateralized glenohumeral center of rotation led to excessive shear forces and failure of the glenoid component [1, 2].”
Major Error: Both references 1 and 2 are unrelated in that neither is about the early RSA designs. Reference 1 is a book chapter on hemiarthroplasty by Basamania [66], and reference [29] is an editorial by Charles Rockwood on overuse of current RSAs and makes no mention of the early RSAs from the 1970s [67].
4.
Nyffeler [44] assertion: “Earlier types of reversed total shoulder prostheses were withdrawn from the market because of high rate of aseptic loosening of the glenoid component due to high eccentric loads [12].”
Major error: The reference contradicts the assertion that high eccentric loads caused glenoid component failure. The reference listed is a study on the long-term follow-up of the Kessel prosthesis and does not conclude anything about eccentric loads, but rather high loads associated with constrained devices (anatomic and reversed). However, this study does note that “The screw of the scapular component was large in comparison with the bone available for fixation in the scapular neck, leaving little room for variations. Thus, individual bone quality and differences in neck size could account for variations in loosening” [68].
5.
Trappey [48] assertion: “These initial RSA designs had a laterally offset center of glenohumeral rotation that led to a high rate (26 %) of glenoid component loosening and failure [1].”
Major Error: The authors are referring to the 26 % failure rate of the Kessel design in the 1992 paper by Brostrom [21]. However, the authors do not reference Brostrom directly, and they only reference Boileau’s paper from 2005 which states the re-operation rate in Brostrom’s paper was 26 % which is true. However, the aseptic baseplate loosening rate in the Brostrom’s paper is only 13 % and not 26 % as asserted by Trappey et al.
Summary of Investigation
This study showed that 24 out of 32 (72 %) of articles found in the current RSA literature that refer to the original RSA devices contain at least one quotational error. The most common form of error was asserting that failure in the original RSA devices on the glenoid side was caused by a particular factor when in fact none of the referenced studies were designed to determine causative factors of failure. Seventeen of the 32 articles made at least one assertion of causality, with the most frequent being that a lateral center of rotation and/or excessive shear forces led to high rates of glenoid-sided failures in early RSA designs [1, 3, 5, 24, 25, 29, 30, 34, 36, 37, 39–41, 43, 44, 48, 49]. Not only did the referenced articles not determine causality nor attempt to, but some of the articles did not report any glenoid-sided failures [6, 8, 10, 12]. One possible reason for this mistake is that the authors assumed that all of these devices had high rates of failure and did not read the original articles to verify this assertion.
In looking at these articles in total, I have identified what I believe is a two-part narrative that made its way in whole or partially into the studies that asserted causality. One part of the narrative is the assertion that all early RSA designs had a high rate of failure. I believe this is partly due to the fact that some early RSA articles were included in reports of the early anatomic constrained designs which had up to a 100 % failure rate (Stanmore [58]). In fact in a study by Wirth et al. [63], the authors mention that the failure rates range from 8 to 100 % in constrained arthroplasty and they reference 13 articles. It turns out that only two of those 13 references are about early RSA designs. Those two articles happen to be the study by Fenlin [9] and the other by Kölbel [15]. Again, the Fenlin’s study is more of a design rationale with a report of 5 very difficult and unusual cases undermining most conclusions drawn from it, and the other study by Kölbel only reported one glenoid component loosening. Also, as seen in the Boileau [25] study in example 2, when discussing failures in the past, he cites 5 studies, but only one was on early RSA and the other 4 were on anatomic constrained devices. These are good examples of how the failures of the anatomic constrained devices may taint the perception of early RSAs and thus influence the narrative today.
The second part of the narrative has to do with the notion that the lateral center of rotation is the main causative factor for failure in RSAs. In reviewing the early RSA series, it is not possible to isolate one causative factor as failures may have been due to various patient factors, cementation of the glenoid component, lack of boney ingrowth surfaces, the constraint of the implants, or other unknown factors. Additionally, for some reason many authors tended to focus exclusively on Grammont’s modification from 2/3 of a sphere to a hemisphere and conclude that this medialization of the COR was the key to success. However, they ignore the other substantive change of making the press-fit baseplate with porous coating and transfixion screws, eliminating the need to cement the glenoid component. It is likely that both of these changes had an effect, but for some reason, the latter is omitted from discussion. The result of this narrative has been 16 subsequent studies that essentially repeated the unsubstantiated causal assertion of Boulahia’s [24] study from 2002. Our group is not immune to this as we have repeated the narrative in two of our studies as well (Frankle, Holcomb). At the time of publication of this chapter, the Boulahia [24] study had been citied 184 times. The 16 subsequent studies [1, 3, 5, 25, 29, 30, 34, 36, 37, 39–41, 43, 44, 48, 49] had been cited 2,341 times. It becomes apparent how an unsubstantiated assertion can become an accepted narrative.
Conclusion
The intent of this investigation was not to make my own assertion about the causes of failure or success in both early and modern RSA. Rather, my investigation began as a deep dive into the original studies on RSA for a more thorough understanding of how this procedure came to be. In examining these original articles it became clear that there are current misconceptions, and this chapter is an attempt to present evidence to counter the narrative that has emerged as a result.
Appendix
Type | |||||||||
|---|---|---|---|---|---|---|---|---|---|
No error | Major error | Minor error | |||||||
Lead author | Year | Title | Unrelated reference | Unsubstantiated assertion | Generalization | Specific quotation(s) | Description of error | Description of error | |
Ahir, S.P. | 2004 | Analysis of glenoid fixation for a reversed anatomy fixed-fulcrum shoulder replacement | 1 | ||||||
Baulot E.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||||||||