Operative Treatment of Radial Neck Fractures
Donald S. Bae
INDICATIONS/CONTRAINDICATIONS
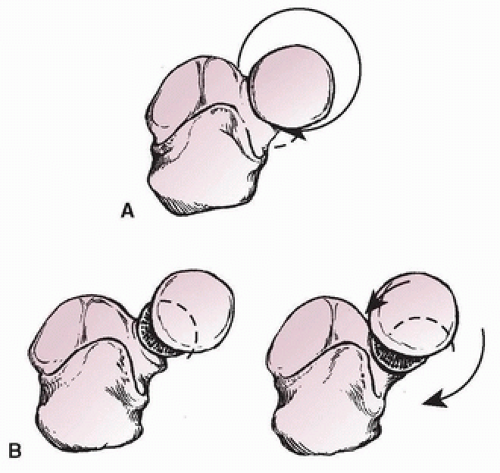
Radial neck fractures are common in children, and a number of anatomic considerations guide orthopedic management. First, due to the relatively constrained morphology of the proximal radioulnar joint (PRUJ), excessive angulation or displacement may cause limitations in forearm rotation (Fig. 4-1). Second, given the proximity of these injuries to the adjacent radiocapitellar joint, marked displacement may result in static or dynamic radiocapitellar instability. In addition, as there are no direct ligamentous or muscular attachments to the radial head/neck, closed reduction maneuvers may be challenging, and open approaches to the proximal radial epiphysis carry the risk of osteonecrosis. Finally, due to the relatively minor contribution of the proximal physis to the longitudinal growth of the radius, remodeling potential is limited, and therefore, careful consideration of radiographic alignment is needed.
Fractures are classified according to anatomic location, displacement, and angulation. Chambers, O’Brien, and Judet have previously classified these fractures into three categories (Table 4-1). At present, surgical indications include fractures with excessive angulation and/or displacement resulting in joint instability or functional loss of forearm rotation that will not be expected to remodel with continued skeletal growth. In general, injuries with greater than 30 degrees angulation or 3 mm translation merit reduction with or without stabilization.
There are challenges associated with surgical treatment. Historic literature suggests that open and more invasive approaches to radial neck fractures are associated with worse clinical results. Therefore, rather than think about contraindications to surgery, perhaps it is best to maximize non-operative treatment unless there is a contraindication to nonsurgical care.
PREOPERATIVE PREPARATION
Preoperative planning begins with characterization and understanding of the injury pattern and deformity. Appropriate plain radiographic imaging consisting of anteroposterior (AP), lateral, and oblique views of the elbow should be carefully evaluated. A systematic approach to radiographic evaluation should also include assessment of associated injuries (e.g., medial epicondyle fractures, coronoid fractures, concomitant elbow dislocations), which may be present in up to 20% of patients. Advanced imaging is rarely necessary; computed tomography (CT) scans do not visualize the cartilaginous articular surfaces and epiphyses and confer additional radiation exposure.
Comprehensive preoperative physical examination should assess for neurologic status, particularly of the radial and posterior interosseous nerves, as well as range of forearm rotation.
TABLE 4-1 Judet Classification of Pediatric Radial Neck Fractures | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
EDITOR’S NOTE
DLS recommends warning the family ahead of time that with this injury some permanent loss of pronation and supination is likely even if everything is done just right. If you tell the family ahead of time, you may be perceived as a wise and experienced surgeon; if you explain this afterwards, you may be perceived as making excuses.
SURGICAL PROCEDURE
There is a wealth of published information suggesting open reduction is associated with poorer outcomes and should be avoided if possible. Potential reasons for this include selection bias inherent in retrospective studies (i.e., more severe injuries necessitating open reduction are prone to worse clinical results); increased soft-tissue trauma during surgical exposure resulting in scar formation, stiffness, and even devascularization of the small proximal chondroepiphyseal fragment; or greater instability imparted by disruption of the periosteum and surrounding soft tissues. For these reasons, a stepwise treatment algorithm has been suggested in the approach to displaced radial neck fractures, beginning from the least invasive method of reduction and advancing to more invasive techniques only if needed (Table 4-2).
After adequate induction of general anesthesia and administration of preoperative antibiotics, patients are placed in the supine position with the affected limb supported by a radiolucent hand table. Care is taken to provide adequate access for intraoperative fluoroscopic imaging of the elbow during patient positioning. A nonsterile tourniquet may be placed on the upper brachium. The entire affected limb is prepped and draped in the usual sterile fashion.
Closed reduction maneuvers may be attempted first, and a number of techniques have been proposed (Fig. 4-2). The Patterson technique employs longitudinal traction, elbow extension, forearm
supination, and varus stress with direct pressure applied to displaced proximal radius epiphysis. The Israeli technique utilizes elbow flexion and forearm rotation to rotate the displaced epiphyseal segment into the pressure of the provider’s finger to effectuate reduction. Use of an Esmarch elastic bandage wrapped from distal to proximal may also facilitate reduction of the displaced proximal fracture fragment. Careful evaluation of both radiographic alignment and forearm rotation may be performed. In cases in which adequate reduction is achieved, the limb is placed in a long-arm cast. These techniques frequently work well enough to avoid surgery, so persistence in trying multiple techniques may be worthwhile.
supination, and varus stress with direct pressure applied to displaced proximal radius epiphysis. The Israeli technique utilizes elbow flexion and forearm rotation to rotate the displaced epiphyseal segment into the pressure of the provider’s finger to effectuate reduction. Use of an Esmarch elastic bandage wrapped from distal to proximal may also facilitate reduction of the displaced proximal fracture fragment. Careful evaluation of both radiographic alignment and forearm rotation may be performed. In cases in which adequate reduction is achieved, the limb is placed in a long-arm cast. These techniques frequently work well enough to avoid surgery, so persistence in trying multiple techniques may be worthwhile.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree