Closed Reduction and Casting of Forearm Fractures
Kevin J. Little
Roger Cornwall
INTRODUCTION
The radius and ulna are the most common locations for fractures in children. While distal radius metaphyseal fractures are the most common specific site of injury, diaphyseal forearm fractures rank third in overall fracture incidence just behind supracondylar humerus fractures. Most injuries occur via a fall on outstretched hand (FOOSH) mechanism, commonly from playground equipment or during sporting activities. Diaphyseal forearm fractures are best described by location (proximal, middle, or distal third), by fracture type (greenstick, plastic deformation, complete, or comminuted), and using measurements of biplanar angulation.
The forearm can be considered as a membranous joint, connected by the supporting struts of the proximal and distal radioulnar joints. These are centrally stabilized by the interosseous membrane and work concertedly to allow for approximately 180 degrees pronation and supination. The center of forearm rotation passes from the center of the radial head through the interosseous membrane to the fovea of the distal ulna. The precise alignment of the radius and ulnar shaft allow for full rotational mobility, and malalignment can lead to clinically apparent loss of motion.
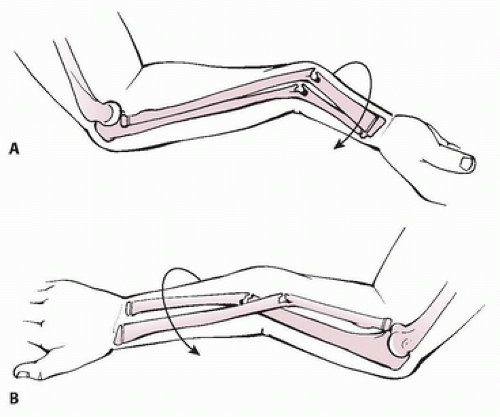
Injuries to the forearm present clinically with pain, edema, and deformity in the forearm. Subtle fractures may not exhibit clinical deformity, especially in small children with a large soft-tissue envelope, but clinical examination can identify tenderness to palpation and loss of forearm motion. Open fractures typically are associated with an inside-out mechanism, with grade I injuries being the most common. A careful clinical exam should be performed to evaluate for subtle open wounds, which can seal over quickly after the initial injury. A standard radiographic evaluation of forearm injuries includes AP and lateral radiographs of the forearm combined with dedicated biplanar elbow and wrist radiographs to evaluate for concomitant Monteggia and Galeazzi lesions. Assessment of angular malalignment on the AP and lateral planes helps determine treatment of diaphyseal fractures. Forearm fractures with fracture lines at the same level at the radius and ulna imply a limited rotational component to the fracture mechanism. Radius fracture more proximal to the ulna fracture implies a supination moment during injury, while a radius fracture more distal to the ulna fracture implies a pronation moment in apex volar extension-type injuries (Fig. 6-1). In complete fractures, rotational malalignment of each bone may be judged by the relationship between the bicipital tuberosity and the radial styloid, which averages 123 degrees, and the relationship between the coronoid process and the ulnar styloid, which is approximately 180 degrees.
INDICATIONS/CONTRAINDICATIONS
Closed reduction and rigid immobilization are the gold standard for pediatric forearm fracture treatment. Closed reduction can be successful for nearly all fracture patterns, including greenstick, complete, plastic deformation, and even comminuted fractures. Any angulated or displaced fracture should undergo attempted closed reduction, except in cases of significant soft-tissue injury where immediate surgical fixation is planned. Contraindications for closed treatment are those where rigid immobilization is not possible due to significant soft-tissue loss or compartment syndrome. Additional
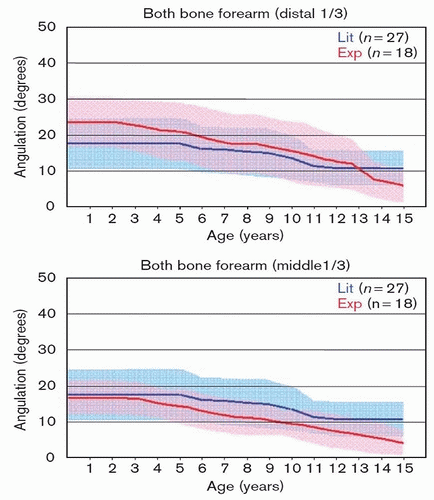
contraindications occur in cases where excessive swelling is expected to occur, such as in closed crush injuries or concomitant injuries such as a humerus fracture (floating elbow) or carpal fracture requiring surgical stabilization. Based on the available evidence in the literature, the threshold for acceptable alignment is approximately 20 degrees in the distal third of the forearm, 15 degrees in the middle third of the forearm, and 10 degrees in the proximal third—with more angulation acceptable at times, particularly in the distal third in children with lots of growth. Ploegmakers published graphs for radius and ulna fractures, which can be used to plot acceptable fracture alignment at all patient ages utilizing both expert consensus and a meta-analysis of available literature (Fig. 6-2). Rotational
deformities in the radius and ulna of up to 30 degrees can be tolerated due to compensatory wrist rotation, but will not remodel over time. Additionally, bayonet apposition with 1 cm of shortening is also acceptable in patients less than 12 (boys) and 10 (girls).
contraindications occur in cases where excessive swelling is expected to occur, such as in closed crush injuries or concomitant injuries such as a humerus fracture (floating elbow) or carpal fracture requiring surgical stabilization. Based on the available evidence in the literature, the threshold for acceptable alignment is approximately 20 degrees in the distal third of the forearm, 15 degrees in the middle third of the forearm, and 10 degrees in the proximal third—with more angulation acceptable at times, particularly in the distal third in children with lots of growth. Ploegmakers published graphs for radius and ulna fractures, which can be used to plot acceptable fracture alignment at all patient ages utilizing both expert consensus and a meta-analysis of available literature (Fig. 6-2). Rotational
deformities in the radius and ulna of up to 30 degrees can be tolerated due to compensatory wrist rotation, but will not remodel over time. Additionally, bayonet apposition with 1 cm of shortening is also acceptable in patients less than 12 (boys) and 10 (girls).
PREOPERATIVE PREPARATION
An AMPLE (Allergies, Medications, Past medical history, Last meal, Events preceding injury) history and physical examination is required prior to any intervention beyond splinting. The physical exam should include inspection of the arm for open wounds, abrasions, or deformity as well as assess for neurovascular deficits and signs of compartment syndrome. The patient should be brought to an appropriate setting for closed reduction such that vital signs can be monitored and the patient’s safety ensured. Such a room could include a dedicated orthopedic reduction room in the ER or operating room where the necessary orthopedic supplies and radiographic control are readily available. There is no evidence to suggest a clinical difference between fractures immobilized in plaster splints as compared to bivalved fiberglass casts following reduction.
TECHNICAL PROCEDURE
Greenstick Fracture
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree