Proximal Tibial Osteotomy for Tibia Vara
J. Eric Gordon
Perry L. Schoenecker
INDICATIONS/CONTRAINDICATIONS
The indication for a proximal tibial osteotomy in the treatment of infantile tibia vara (Blount disease) is the presence of Langenskiold stage III or greater radiographic changes involving the proximal tibia. These patients typically have had a varus deformity noted since they began walking. Following a proximal varus-correcting osteotomy, restoration of normal proximal medial physeal growth is more likely if surgery is performed when the child is 4 years of age or less. The main contraindication for proximal tibial osteotomy in children with tibia vara is the presence of a deformity with sufficient physeal growth to achieve correction by bracing or plate hemiepiphysiodesis. Older children (over 7 or 8 years of age) who have deformities that include partial physeal closure, medial plateau depression, and distal femoral deformity may require additional procedures such as physeal bar resection, plateau elevation, or distal femoral osteotomy in addition to a valgus osteotomy (1, 2).
The indication for a proximal tibial osteotomy in patients with juvenile or adolescent tibia vara is the presence of a deformity that cannot be corrected by temporary hemiepiphysiodesis using a plate or staples. The deformity in late-onset tibia vara is usually noted by the family when the patient is 8 years or more of age. In contrast to the early onset of infantile tibia vara, patients with late-onset tibia vara typically are 8 years of age or older prior to the noted observation of developing a knee-centered varus deformity. The primary contraindication to tibial osteotomy is, like infantile tibia vara, the presence of a deformity with sufficient growth to allow correction by hemiepiphysiodesis. Adolescent tibia vara frequently occurs in association with distal femoral varus, proximal tibial procurvatum, internal rotation, distal tibial valgus, and lateral collateral ligament laxity. When diagnosed, late-onset tibia vara should be surgically treated. Patients with distal femoral or distal tibial deformities should undergo correction of these deformities concurrently with correction of the proximal tibial varus and procurvatum.
PREOPERATIVE PREPARATION
Preoperative planning in younger children, typically 3 to 6 years of age, with infantile Blount deformity, involves insuring that an OR table is available that optimizes the intraoperative use of either image intensification or plain radiographs to monitor intraoperative correction. The fibula is approached through a separate lateral incision and is osteotomized approximately 1 to 2 cm distal to the intended osteotomy of the tibia. The tibia is approached through a proximal, longitudinal incision, and the tibial osteotomy is performed at a level distal to the physeal extension of the tibial tubercle. The osteotomy is performed in a transverse plane, allowing correction of frontal, sagittal, and rotational deformities; fixation is provided with Kirchner wires in this younger age group. Correction of the varus deformity is verified both visually and radiographically.
Preoperative clinical and radiographic planning for children with late-onset tibia vara is essential for successful, accurate correction of the deformity. Older children with tibia vara are frequently
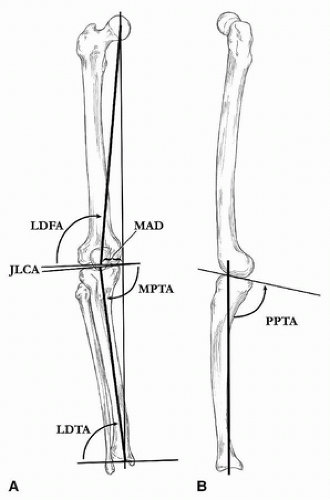
obese and can have complications of obesity such as obstructive sleep apnea (3). After appropriate medical workup, a standing anterior-posterior radiograph of both lower extremities should be obtained on a single image, typically on an electronic digital radiographic system. Alternatively, a traditional radiographic system can be used to obtain a long image on a 51-inch (130-cm) radiographic cassette. A lateral of the knee showing the tibial shaft should also be obtained. An additional standing anterior-posterior radiograph of both ankles extending to the midtibial shaft should also be obtained to evaluate for distal tibial valgus. The anterior-posterior radiograph should be evaluated to determine the presence and magnitude of any distal femoral deformity as well as lateral collateral ligament laxity, proximal tibial varus, and procurvatum. The location of the deformities should also be assessed (4, 5). We have utilized the methods of Paley and Tetsworth in evaluating these deformities by measuring the mechanical axis deviation (MAD), the lateral distal femoral angle (LDFA), the medial proximal tibial angle (MPTA), the joint-line congruency angle (JLCA), and the lateral distal tibial angle (LDTA) (Fig. 32-1A). Proximal tibial sagittal plane deformity should be evaluated by measuring the posterior proximal tibial angle (PPTA) (Fig. 32-1B). Based on the analysis, an overall surgical strategy should be planned for single-stage correction of the deformities. Distal femoral deformity should be corrected by a distal femoral osteotomy and stabilized using a blade plate. Tibial deformities and ligamentous laxity are most often treated by hexapod circular external fixation (1, 6). The tibial deformities can be corrected by proximal and if needed distal tibial osteotomies followed by gradual correction. Lateral collateral ligament laxity can be corrected by distal transport of the proximal fibula resulting in tightening of the lateral collateral ligament. If lateral collateral ligament laxity is not present and there is less than a 2-cm limb-length discrepancy as assessed on the anterior-posterior radiograph of the lower extremities, a fibular osteotomy will not be required during gradual correction if the correction is centered at the proximal fibula, allowing mild lengthening of the tibia. A definitive plan for the magnitude of the femoral and tibial osteotomies should be prepared prior to the initiation of operative care in line with the principles of deformity correction.
obese and can have complications of obesity such as obstructive sleep apnea (3). After appropriate medical workup, a standing anterior-posterior radiograph of both lower extremities should be obtained on a single image, typically on an electronic digital radiographic system. Alternatively, a traditional radiographic system can be used to obtain a long image on a 51-inch (130-cm) radiographic cassette. A lateral of the knee showing the tibial shaft should also be obtained. An additional standing anterior-posterior radiograph of both ankles extending to the midtibial shaft should also be obtained to evaluate for distal tibial valgus. The anterior-posterior radiograph should be evaluated to determine the presence and magnitude of any distal femoral deformity as well as lateral collateral ligament laxity, proximal tibial varus, and procurvatum. The location of the deformities should also be assessed (4, 5). We have utilized the methods of Paley and Tetsworth in evaluating these deformities by measuring the mechanical axis deviation (MAD), the lateral distal femoral angle (LDFA), the medial proximal tibial angle (MPTA), the joint-line congruency angle (JLCA), and the lateral distal tibial angle (LDTA) (Fig. 32-1A). Proximal tibial sagittal plane deformity should be evaluated by measuring the posterior proximal tibial angle (PPTA) (Fig. 32-1B). Based on the analysis, an overall surgical strategy should be planned for single-stage correction of the deformities. Distal femoral deformity should be corrected by a distal femoral osteotomy and stabilized using a blade plate. Tibial deformities and ligamentous laxity are most often treated by hexapod circular external fixation (1, 6). The tibial deformities can be corrected by proximal and if needed distal tibial osteotomies followed by gradual correction. Lateral collateral ligament laxity can be corrected by distal transport of the proximal fibula resulting in tightening of the lateral collateral ligament. If lateral collateral ligament laxity is not present and there is less than a 2-cm limb-length discrepancy as assessed on the anterior-posterior radiograph of the lower extremities, a fibular osteotomy will not be required during gradual correction if the correction is centered at the proximal fibula, allowing mild lengthening of the tibia. A definitive plan for the magnitude of the femoral and tibial osteotomies should be prepared prior to the initiation of operative care in line with the principles of deformity correction.
The tibial deformity is carefully analyzed to identify the magnitude of both the frontal and sagittal plane deformities and the limb-length discrepancy. The magnitude of the internal rotation deformity is assessed clinically. The desired correction is entered into the software program after determining the CORA and mounting parameters of the fixator. Preconstruction of the external fixator should be carried out prior to surgical intervention. If the patient is skeletally immature, a single proximal full ring is used to stabilize the proximal fragment (Fig. 32-2A). If the patient is skeletally mature, a ring block of two 2/3 rings separated by two-hole Rancho cubes can be used to stabilize the proximal fragment (Fig. 32-2B).
SURGICAL PROCEDURE (ACUTE CORRECTION)
Children in whom an acute correction is planned are positioned supine on a radiolucent table. Both lower extremities are prepped and draped exposing each from the level of the proximal thigh to the toes. In unilateral procedures, exposure of both extremities allows for comparison of correction of the involved versus the uninvolved extremity. A sterile tourniquet is applied on the upper thigh, and antibiotics are administered prior to the tourniquet inflation. The proximal tibia is approached through a longitudinal incision centered over the anteromedial proximal tibia extending from a point proximal to the tibial tubercle distally down the leg to a point a few centimeters beyond the anticipated site of the tibial osteotomy. Subcutaneous flaps are raised medially exposing the anteromedial surface of the tibia. The overlying periosteum is incised, and the tibia is carefully subperiosteally circumferentially exposed using subperiosteal elevators. The anterior compartment musculature is directly exposed at this time and/or later during the time of osteotomy of the tibia. The tibial tubercle is palpated but is not exposed. An image intensifier is helpful in selecting the appropriate site of the intended transverse osteotomy.
Once the site of the tibial osteotomy has been exposed, this wound is packed and the fibula is approached through a separate lateral incision. This approach is made through a 2- to 3-cm longitudinal incision centered over the lateral intramuscular septum. Again, subcutaneous flaps are elevated. The interval between the posterior edge of the lateral compartment (peroneal musculature) and the posterior compartment is the most direct internervous approach to the proximal fibula. This interval is developed with scissors and/or digitally. The fibula is palpated and visualized, and the deepest portion of the peroneal muscle that surrounds the fibula and underlying periosteum is incised exposing the fibular diaphysis. With caution, small subperiosteal retractors are carefully placed around the entire fibula. The fibula is then osteotomized in a transverse plane with an oscillating saw. Care must be taken so as not to directly or indirectly injure neurovascular structures (peroneal nerve motor branches to the anterior compartment and adjacent veins) lying just medial to the tibia (7). Depending on degree of varus correction necessary, a small segment (1 cm or less) of fibula is excised. This fibular wound is packed, and a transverse tibial osteotomy is carefully performed again using a microsagittal saw (Fig. 32-3). In correcting the varus deformity, the goal




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree