Operative Treatment of Pediatric Forearm Fractures Using Flexible IM Rodding
Julie Balch Samora
Donald S. Bae
Peter M. Waters
Pediatric diaphyseal fractures of the forearm constitute about 6% of pediatric fractures and occur in approximately 1:100 children yearly. Distal metaphyseal and physeal fractures of the radius and ulna are far more common. Diaphyseal radius and ulna fractures are classified as plastic bone deformation injuries, incomplete or greenstick fractures, or complete, displaced fractures. These fractures rarely involve disruption of the distal radioulnar joint (Galeazzi fractures) or the proximal radioulnar joint (Monteggia fractures). They can coexist with fractures of the humerus, thereby constituting a pediatric floating elbow. Treatment options for displaced radial and ulnar diaphyseal fractures include closed reduction and cast immobilization, closed reduction and intramedullary (IM) fixation, and open reduction with internal fixation. Most plastic deformation and incomplete diaphyseal fractures can be successfully treated with closed manipulation and cast immobilization. Fracture reduction and maintenance of postmanipulation alignment in a cast depend on the presence of a periosteal tension band. With increasing age and worsening severity of fracture, closed reduction and cast treatment will more often fail to maintain acceptable alignment in complete fractures. In the 1970s, Prevot and Metaizeau introduced elastic intramedullary nail (ESIN) fixation in Nancy, France, to treat unstable fractures with unacceptable alignment.
The goals of closed IM fixation of the forearm are to achieve near-anatomic reduction of the radius and ulna and to maintain fracture alignment throughout the healing process. If fracture stabilization has been carried out with use of percutaneously placed IM rod(s), the periosteum of a child’s bone will mechanically resist torsional forces and will aid in healing through its vascularity. Thus, most unstable pediatric forearm fractures can be treated with IM rods instead of the plate-and-screw internal fixation that is required in adult diaphyseal forearm fractures.
IM fixation offers the advantages of less-invasive surgery with small incisions and minimal soft-tissue insult. Restoring the anatomic bow of the radius requires appropriate pre-bending of the radial elastic nail. Smaller nails (typically 2 to 3 mm in diameter) are chosen to fill approximately one-third of the IM canal. Physeal-sparing entry sites are preferred.
In general, fixation of both the radius and the ulna is utilized for fracture alignment and stability. Single-bone fixation, usually with an IM rod in the ulna, has been successfully utilized in unstable fractures in younger children (Fig. 5-1). This technique converts the complete fracture into an incomplete fracture and allows the radius to be rotated to an acceptably reduced position. If there is persistent radial deformity, a radial IM nail should be considered to be added to the ulnar nail to reduce the radius. This chapter addresses the indications, principles of treatment, techniques, postoperative care, and complications of IM fixation of the forearm in the pediatric patient.
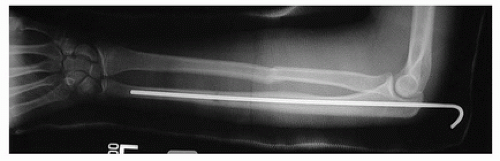 FIGURE 5-1 Single-bone fixation of an unstable forearm fracture with IM rod placement in the ulna. (Used with permission of Children’s Orthopaedic Center, Los Angeles, CA.) |
TABLE 5-1 Indications for Internal Fixation of Pediatric Forearm Fractures | |
|---|---|
|
INDICATIONS/CONTRAINDICATIONS
The main indication for internal fixation in a pediatric patient is malalignment of the radial and ulnar fracture(s). However, there is controversy about how much angulation is acceptable in a child’s diaphyseal forearm fracture. For acceptable cast treatment, maintenance of the radial bow and angulation of fewer than 10 degrees are desired both acutely and during healing. Failure to achieve or maintain reduction by these standards may be considered an indication for internal fixation, with more angulation acceptable in young children with remodeling potential. The less stable the fracture is when initially reduced, particularly in an older child, the clearer are the indications for internal fixation. A floating elbow is also an indication for internal fixation to obviate the need for circumferential cast immobilization, thereby lessening the risk of the development of a compartment syndrome. Open fractures, pathologic fractures, or refractures may also be considered indications for internal fixation in the forearm. (Table 5-1 provides a summary of the indications for internal fixation of pediatric forearm fractures.)
Possible contraindications for the use of IM nails for radius and ulna diaphyseal fractures include an older patient or a severely contaminated open fracture. If all growth plates in the forearm are closed, it may be better to use plate-and-screw internal fixation, as the rate of delayed union of the radius and ulna in older teens and adults appears to be higher with IM nail treatment than if some growth remains. If there is a type III open fracture with marked soft-tissue injury and wound contamination, use of an external fixator to facilitate soft-tissue care would be preferred.
PREOPERATIVE PLANNING
Preoperative anteroposterior (AP) and lateral radiographs of the radius and ulna need to include views of the elbow and wrist. This is particularly important at the elbow to prevent the orthopedist from not recognizing a possible coexisting Monteggia-type injury about the proximal radius. Entry sites for the nail are planned and are to some degree based on the diaphyseal level of the fracture, particularly in the case of the radial fracture. The entire instrument set for inserting flexible IM nails must be available, and all IM nail sizes from 2 to 4 mm should be sterile and ready for use. Fluoroscopy needs to be set up in the operating room. A radiolucent arm operating table is used.
SURGICAL PROCEDURE
Closed reduction and IM fixation of the pediatric forearm is performed in the operating room under general anesthesia. The affected arm is draped to the side on a radiolucent arm table, with the child supine and the shoulder abducted 90 degrees. Antibiotic prophylaxis is provided prior to the
incision. Usually, the bone easiest to reduce is stabilized first. For the ulna, apophyseal and metaphyseal proximal entry sites have both been utilized (Fig. 5-2). Because the olecranon apophysis does not contribute significantly to the growth of the ulna, most pediatric orthopedists will pass a small-diameter, smooth rod or Steinmann across the proximal ulnar apophysis, thereby allowing a straight passage of the nail down the ulnar medullary canal. Alternatively, a split is made in the anconeus muscle on the subcutaneous border of the ulna, and an appropriate bend is made in the nail for passing the rod from the proximal to the distal end of the ulna. Distal entry between the flexor carpi ulnaris tendon and the extensor carpi ulnaris tendon has also been used. The size of the nail used depends on the size of the medullary canal on radiograph. The thinnest diameter of the ulna is located at its distal end; the ulna nail is usually 2 to 3 mm in diameter.
incision. Usually, the bone easiest to reduce is stabilized first. For the ulna, apophyseal and metaphyseal proximal entry sites have both been utilized (Fig. 5-2). Because the olecranon apophysis does not contribute significantly to the growth of the ulna, most pediatric orthopedists will pass a small-diameter, smooth rod or Steinmann across the proximal ulnar apophysis, thereby allowing a straight passage of the nail down the ulnar medullary canal. Alternatively, a split is made in the anconeus muscle on the subcutaneous border of the ulna, and an appropriate bend is made in the nail for passing the rod from the proximal to the distal end of the ulna. Distal entry between the flexor carpi ulnaris tendon and the extensor carpi ulnaris tendon has also been used. The size of the nail used depends on the size of the medullary canal on radiograph. The thinnest diameter of the ulna is located at its distal end; the ulna nail is usually 2 to 3 mm in diameter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








