Operative Reconstruction of Boutonnière and Swan-Neck Deformities
Jun Y. Matsui
Samantha L. Piper
Martin I. Boyer
DEFINITION
Rheumatoid arthritis is a poorly understood systemic disease affecting the synovium of joints and tendon sheaths. The synovial tissue in rheumatoid arthritis is characterized by a proliferation of synovial lining cells, angiogenesis, and relative lymphocytosis.15
A combination of cartilage degeneration, synovial expansion, periarticular erosion, and ligamentous laxity creates an imbalance within the extrinsic and intrinsic tendon systems of the digit, causing progressive deformity.
A boutonnière (“buttonhole”) deformity involves attenuation or disruption of the central slip and attenuation of the triangular ligament. It results in a characteristic deformity with flexion at the proximal interphalangeal (PIP) joint and hyperextension (as well as an inability to flex actively) at the distal interphalangeal (DIP) joint.
A swan-neck deformity is characterized by hyperextension of the PIP joint and flexion of the DIP joint.
In the posttraumatic setting, it results from laxity of the PIP joint volar plate and an inability of the terminal tendon to extend the DIP joint (chronic mallet finger deformity).
Classification
Type I—boutonnière deformity: metacarpophalangeal (MCP) joint flexion and interphalangeal joint hyperextension. The carpometacarpal (CMC) joint is not primarily involved.
Type II—rare: a combination of types I and III involving MCP joint flexion and interphalangeal joint hyperextension and associated CMC joint subluxation or dislocation
Type III—swan-neck deformity: MCP joint hyperextension, interphalangeal joint flexion, and thumb metacarpal adduction, resulting from progressive CMC joint pathology
Type IV: gamekeeper’s deformity. Attenuation of the ulnar collateral ligament of the thumb MCP joint results in radial deviation of the MCP joint and secondary metacarpal adduction deformity or contracture.
Type V: results from attenuation of the MCP volar plate with progressive MCP joint hyperextension and secondary interphalangeal joint flexion. There is no metacarpal adduction deformity.
Boutonnière deformity
Stage I—mild: PIP joint synovitis and a mild, fully correctable extension lag
Stage II—moderate: flexion deformity of the PIP joint, either flexible or fixed
Stage III—severe: PIP joint articular destruction
Swan-neck deformity
Type I: PIP joint is fully mobile.
Type II: Active and passive motions of the PIP joint are limited, with the MCP joint held in extension due to intrinsic tightness.
Type III: decreased PIP joint motion in all positions of MCP joint flexion and extension
Type IV: fixed PIP joint hyperextension with advanced destruction of the PIP joint articular surfaces
ANATOMY
Bone and Joint
The MCP joint is a condyloid joint with average range of motion from 15 degrees hyperextension to 90 degrees flexion.
A cam effect for collateral ligaments is due to the shape of the metacarpal head; collateral ligaments are taut with MCP joint flexion and lax with MCP joint extension.
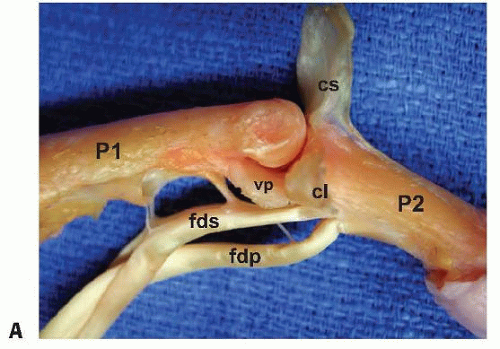
The PIP joint (FIG 1A) is a hinge joint with greater inherent osseous stability than the MCP joint due to the configuration of the two condyles of the head of the proximal phalanx, which articulates with the median ridge at the base of the middle phalanx.
The collateral ligaments are taut throughout the joint arc of motion.
The volar plate resists PIP joint hyperextension; it originates on the proximal phalanx and inserts into the base of the middle phalanx.
The DIP joint is stabilized by the collateral ligaments, the terminal extensor tendon insertion, the flexor digitorum profundus (FDP) insertion, and the volar plate.
Dorsal Restraining Structures of the Digit
The sagittal bands originate on both sides of the MCP joint, from the volar plate and the base of the proximal phalanx, and insert into the lateral margins of the extensor tendon over the dorsal MCP joint (FIG 1 B-D).
They stabilize the extrinsic extensor tendon over the MCP joint to prevent lateral subluxation.
They contribute indirectly to MCP joint extension and prevent extensor bowstringing.
The triangular ligament stabilizes the two conjoined lateral bands over the dorsal aspect of the middle phalanx and prevents volar subluxation of the conjoined lateral bands.
The transverse retinacular ligament is composed of fibers oriented in a volar-dorsal direction at the level of the PIP joint. It prevents dorsal subluxation of the conjoined lateral bands.
The oblique retinacular ligament is a static restraining ligament, linking the PIP and DIP joints. It runs from the fibro-osseous gutter at the A2 flexor pulley and the middle third of the proximal phalanx to insert into the terminal extensor tendon and couples PIP joint and DIP joint extension.
Flexor Tendon: Digit
At the level of the A1 pulley, the flexor digitorum superficialis (FDS) tendon flattens and bifurcates to allow the more dorsal FDP tendon to pass distally within the flexor sheath to insert at the volar base of the distal phalanx.
The FDS tendon slips rotate laterally and dorsally around the FDP and then divide again into medial and lateral slips. The medial slips rejoin dorsal to the FDP tendon and insert into the distal aspect of the proximal phalanx. The lateral slips continue distally to insert into the base of the middle phalanx.
Extensor Tendon: Digit
At the base of the proximal phalanx, the extrinsic extensor tendon trifurcates with the central portion inserting into the dorsal base of the middle phalanx as the central slip.
The lateral slips are joined by the oblique fibers of the lumbrical tendons to form the conjoined lateral band. The conjoined lateral bands converge over the middle phalanx to form the terminal tendon, which inserts at the dorsal base of the distal phalanx, where it functions to extend the DIP joint.
The interosseous muscles contribute to the dorsal extensor apparatus through their deep muscle belly, which travels superficial to the sagittal band as the lateral tendon, becoming the transverse fibers of the extensor hood (MCP joint flexion).
PATHOGENESIS
Posttraumatic Boutonnière Deformity
Disruption of the central slip and triangular ligament is the inciting pathology in the development of the boutonnière deformity.
Injury patterns can be grouped into two broad categories, closed and open.
Closed injuries: Forceful hyperflexion of the PIP joint may result in a detachment of the central slip from its insertion. An associated avulsion fracture involving the insertion of the central slip may be identified from the dorsal base of the middle phalanx.
Volar dislocations of the PIP joint or digital crush injuries may disrupt the central slip.
Open injuries: Dorsal laceration or deep abrasions over the PIP joint may disrupt the integrity of the central slip.
Disruption of the central slip and attenuation of the triangular ligament allows for the migration of the lateral bands volar to the PIP joint axis of rotation. This results in flexion at the PIP joint and extension at the DIP joint through the action of the displaced lateral bands.
The displaced lateral band becomes a flexor of the PIP joint and an extensor of the DIP joint.
Posttraumatic Swan-Neck Deformity
Unrecognized volar plate injury at the PIP joint may result in volar plate insufficiency. Although this injury usually leads to scarring volar to the PIP joint and the subsequent development of a PIP fixed flexion deformity without coexistent DIP hyperextension deformity (a so-called “pseudoboutonnière deformity”), this leaves the action of the central slip unchecked by the volar plate, resulting in a progressive PIP joint hyperextension deformity.
Recurrent dorsal dislocation of the PIP joint is an example of an injury pattern that may result in volar plate incompetence.
Avulsion of the terminal tendon from its insertion at the base of the dorsal distal phalanx (a soft tissue mallet finger) results in an imbalance in the extensor mechanism. Extension forces are concentrated at the central slip and by the lateral bands dorsal to the axis of rotation of the PIP joint, producing a progressive hyperextension deformity of the PIP joint.
Patients predisposed to volar plate laxity (such as from generalized ligamentous laxity, inflammatory conditions, and collagen vascular disorders) are more susceptible to the development of deformity.
An extension-type malunion of the middle phalanx or peritendinous adhesions secondary to previous digital fracture injury may contribute to the development of a swan-neck deformity, although an extensor lag at the PIP joint from dorsal adhesions may also lead to an inability to actively extend the finger at the PIP joint (not a boutonnière deformity because there is no DIP hyperextension deformity and not a pseudoboutonnière deformity because the PIP flexion deformity is passively correctible).
Hyperextension of the PIP joint and attenuation of the transverse retinacular ligament permits dorsal migration of the lateral bands relative to the PIP joint axis of rotation. The displaced lateral bands act to extend the PIP joint and to flex the DIP joint.
Rheumatoid Boutonnière Deformity
Fingers
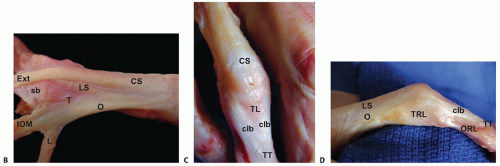
Boutonnière (buttonhole) deformity results from pathologic synovitis of the PIP joint that causes progressive attenuation of the central slip, transverse retinacular ligaments, and triangular ligament. The PIP joint essentially buttonholes through the extensor mechanism.31 Characteristic flexion of the PIP joint and hyperextension deformities of the MCP and DIP joint prevail due to the extensor imbalance22 (FIG 2A).
Subluxation of the lateral bands, volar to the axis of PIP joint rotation, occurs due to the loss of these restraints. The lateral bands become flexors of the PIP joint rather than extensors.
It is important to differentiate this pathologic involvement of the extensor mechanism from a flexion contracture of the PIP joint.
Due to persisting PIP joint flexion, the volar plate, collateral ligaments, and oblique retinacular ligaments become increasingly contracted, resulting in a stiff and subsequently fixed boutonnière deformity.
Thumb
Type I boutonnière deformity is the most common rheumatoid deformity of the thumb.30,38 It is characterized by MCP joint flexion and interphalangeal joint hyperextension (FIG 2B).
The pathologic changes affecting the thumb typically involve synovitis of the MCP joint with resulting attenuation of the extensor mechanism (dorsal joint capsule, extensor pollicis brevis tendon insertion, extensor hood). This relative
extensor imbalance results in MCP joint flexion and possible joint subluxation.
Attenuation of the sagittal band permits ulnar and volar subluxation of the extensor pollicis longus (EPL) tendon, which accentuates MCP joint flexion and interphalangeal joint hyperextension as it translates volar to the axis of MCP joint rotation.
The destructive influence of prolific MCP joint synovitis can cause progressive articular erosion and altered joint surface mechanics, resulting in progressive joint instability and deformity.
As the MCP joint flexion posturing increases in severity, compensatory radial abduction deviation of the thumb metacarpal ensues.
Rupture of the EPL tendon at the wrist can result in a similar “extrinsic-minus” deformity of the thumb.21,27
Boutonnière deformity can result, also, from a hyperextension deformity of the thumb interphalangeal joint secondary to joint synovitis with attenuation of the volar plate or to rupture of the flexor pollicis longus tendon.20
Generally, these primary interphalangeal joint etiologies present with less dramatic MCP joint flexion deformity.34
Rheumatoid Swan-Neck Deformity
Fingers
Swan-neck deformity may result from pathologic rheumatoid synovitis of the MCP, PIP, or DIP joints and is characterized by PIP joint hyperextension and MCP and DIP flexion deformities.
Progressive attenuation of the volar plate, collateral ligaments, and insertion of the FDS tendon results in the development of a PIP hyperextension deformity.
Attenuation of the transverse retinacular ligaments may occur from synovitis, thereby resulting in a loss of the normal restraints to dorsal translocation of the lateral bands. As the lateral bands subluxate dorsal to the axis of PIP joint rotation, they become a constant hyperextension force on the PIP joint.
The DIP joint may be the primary cause of swan-neck deformity where synovitis results in the attenuation and possible rupture of the terminal extensor tendon. This leads to a concentration of the extensor forces at the PIP joint and a resultant hyperextension deformity.
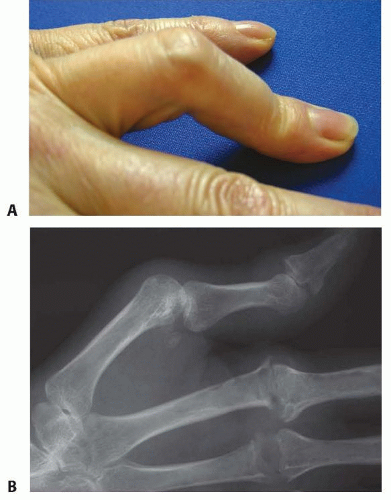
Pathologic alterations in MCP joint mechanics may initiate the development of a swan-neck deformity. Progressive flexion deformity and ulnar drift of the digit results in an imbalance of the extensor mechanism whereby the lateral bands are drawn dorsally, concentrating an extension-hyperextension force at the PIP joint. Flexion deformity at the MCP joint may be secondary to several causes (FIG 3A,B):
Chronic synovitis and associated attenuation of the sagittal bands
Articular destruction with associated joint deformity and volar joint subluxation
The influence of intrinsic tightness or contracture
Persisting PIP hyperextension results in contracture of the extensor apparatus, particularly the triangular ligament as well as the skin. These progressive changes result in a stiff and subsequently fixed PIP joint hyperextension contracture.
Digital flexor tenosynovitis may contribute to poor initiation of digital flexion and an increased extension imbalance at the PIP joint.
Thumb
Type III rheumatoid thumb deformity is the second most common thumb deformity after boutonnière deformity.27,30
The deformity occurs as the result of CMC joint synovitis and associated alterations in thumb mechanics.
Progressive dorsal and radial subluxation of the thumb CMC joint occurs with the deleterious effects of chronic synovitis, including capsular attenuation and articular erosions.
The force vectors associated with pinch and grasp activities accentuate the CMC deformity and accentuate a progressive thumb metacarpal adduction contracture due to a loss of thumb abduction.
As the adduction contracture worsens, hyperextension of the MCP joint (permitted by volar plate laxity) and interphalangeal joint flexion becomes a functional compensation (FIG 3C,D).
NATURAL HISTORY
Traumatic Injury
Early diagnosis is critical for achieving satisfactory outcomes. Reconstructive options become limited as the deformity becomes rigid.
Boutonnière Deformity
Deformity may not be evident immediately after injury but may develop over 2 to 3 weeks.
The pathologic finger posture develops through five stages9:
Disruption of the central slip results in resting flexion of the PIP joint and weak extension of the middle phalanx via the lateral bands.
Attenuation of the triangular ligament and contracture of the transverse retinacular ligaments results in the volar migration of the lateral bands. Active PIP joint extension is absent.
Extension forces are transmitted through the lateral bands, causing hyperextension at the DIP joint.
Progressive contracture of the PIP joint volar plate and the oblique retinacular ligament results in fixed flexion contracture at the PIP joint.
Progressive articular degeneration occurs after prolonged and untreated pathology.
Swan-Neck Deformity
The deformity may be subclassified into four groups that describe the natural history26:
Presence of full passive range of motion at the PIP joint
Prolonged hyperextension of the PIP joint results in intrinsic tightness. The PIP joint exhibits full range of motion when the MCP joint is flexed. However, with the MCP joint extended, PIP flexion becomes limited.
As the transverse retinacular ligament attenuates and the triangular ligament contracts, the subluxated lateral bands become fixed dorsal to the PIP joint axis of rotation. Hyperextension of the PIP joint becomes fixed regardless of MCP joint position.
Progressive PIP joint articular degeneration occurs with chronic, fixed deformity.
Rheumatoid Deformity
The rate of progressive rheumatoid arthritis-related upper extremity deformity appears to be slowing due to improved medical management of this systemic disease process.
The incidence of uncorrectable boutonnière and swan-neck deformities during the first 2 years after the onset of systemic disease is about 16% and 8%, respectively.9
The prevalence of finger deformities in patients with established rheumatoid arthritis is about 36% for boutonnière and 14% for swan-neck deformities.9
The wrist, MCP, and PIP joints are the most commonly affected joints of the upper extremity, and pathologic proliferation of the flexor and extensor tenosynovium may influence digital function and deformity.
PATIENT HISTORY AND PHYSICAL FINDINGS
Posttraumatic Injury
Boutonnière Deformity
A history of blunt trauma to the digit with swelling and tenderness over the PIP joint should arouse suspicion as to the condition. Often, patients report “jamming” or spraining the digit. History of a dorsal digital laceration is similarly concerning.
Deformity may not develop until 10 to 21 days after the injury, making early diagnosis challenging and diligent follow-up imperative. Laceration, ecchymosis, or tenderness over the dorsum of the PIP joint may be diagnostic when a PIP joint extension lag is present.
If the examination is limited due to pain, a digital block should be considered to facilitate a comfortable examination.
The following physical findings are supportive in confirming an early diagnosis:
A 15- to 20-degree PIP joint extension lag with the wrist and MCP joint fully flexed5
Weak extension of the middle phalanx against resistance2
Elson test: Effort to extend the PIP joint accompanied by rigidity of the DIP joint suggests that the central slip is ruptured and forces are being transferred by the lateral bands.
The Elson test is most reliable in diagnosing early boutonnière deformities.32
Boyes test: When the central slip is disrupted, passive extension of the PIP joint causes tension across the lateral bands, resulting in loss of active flexion at the DIP joint. When flexion at the PIP joint is restored, motion at the DIP joint returns.
Swan-Neck Deformity
A history of unrecognized or undertreated trauma or multiple dorsal PIP joint dislocations is common. A patient who presents with a long-standing “mallet” deformity should arouse suspicion, particularly if there is associated hypermobility in the PIP joint of unaffected digits.
Physical examination begins with inspection of the involved digit.
Typically, the PIP joint is hyperextended and the DIP joint is flexed. MCP joint flexion may be present also.
Active and passive range of motion of the PIP joint should be assessed.
In the presence of a flexible deformity, a Bunnell test for intrinsic tightness should be performed.
This test assists the examiner in determining the relative contribution of intrinsic tightness to the deformity.
Increased resistance to passive PIP flexion with the MCP joint in extension compared with flexion indicates a relative shortening of the intrinsic muscle-tendon units.
Rheumatoid Deformity
Diagnostic criteria for rheumatoid arthritis are based on the American College of Rheumatology’s 1988 recommendations.2
Current medications and medical comorbidities may influence decision making for treatment and the timing for surgical intervention.
The evaluation of digital deformities associated with rheumatoid arthritis requires careful global assessment, including neurologic assessment (cervical spine, peripheral compressive neuropathy); appreciation for shoulder, elbow, and wrist involvement; and the awareness of lower extremity deformities that will need reconstructive surgery for which the use of ambulatory aids might be necessary.
As progressive deformity of the wrist occurs, its pathologic influence on digital function and deformity should be recognized.
The carpus typically collapses into supination, with concomitant volar translation and ulnar translocation.4
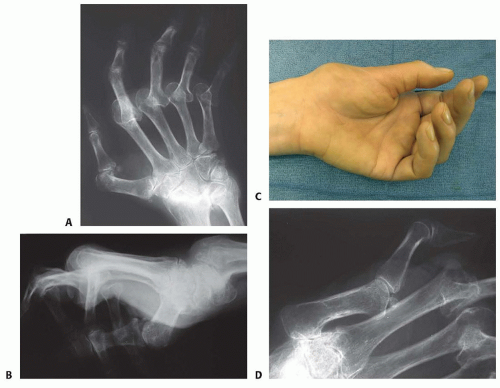
Relative dorsal prominence of the distal ulna may involve a loss of distal radioulnar joint (DRUJ) congruity and may be associated with ruptures of the extensor carpi ulnaris tendon and extensor tendons to the small and ring fingers (caput ulnae syndrome). Inspection of the extrinsic digital extensors, including the EPL,21 should be done, particularly in the presence of active synovitis of the radiocarpal joint and DRUJ (FIG 4).
The MCP joint should be assessed for active synovitis and for characteristic volar subluxation and ulnar drift.
Just as pathologic changes to both the wrist and MCP joints may influence the development of swan-neck and boutonnière deformities of the digits, these changes may adversely affect the outcomes of digital reconstruction if they are not addressed.
Evaluation of the digits should be performed individually with inspection of the resting posture of each digit, assessment of the active and passive motion of each digital joint, and inspection for joint synovitis or tenosynovitis. Skin integrity is assessed for attenuation and for its contribution to joint contracture.
Flexor tenosynovitis may be identified by a palpable fullness in the distal volar forearm or along the digital flexor sheath. Swelling, palpable crepitus along the digital flexor sheath, and a discrepancy between active and passive digital motion are hallmarks of flexor tenosynovitis of the digit.
Flexor tendon rupture may be present, often secondary to attenuation at the volar carpus,20 and should be addressed in the presence of a loss of active digital joint flexion.
Extensor tenosynovitis at the wrist may be determined by palpable tenosynovial hypertrophy, or fullness, and crepitus along the dorsal extensor compartments, proximal and distal to the extensor retinaculum.
Tendon ruptures may be identified by a lack of active digital extension despite active muscular contraction, by palpable tendon deficit, and by a lack of digital extension through tenodesis with passive wrist flexion.

FIG 4 • Preoperative assessment of the digits should include evaluation of the wrist and MCP joints due to their influence on digital function. Wrist stabilization with total wrist arthrodesis and concomitant distal ulnar resection may include soft tissue reconstruction such as tendon repair or tenodesis; such reconstruction should occur before digital reconstructions due to its influence on the outcomes of swan-neck or boutonnière reconstructions. Reconstruction of the MCP joints should occur before or simultaneously with digital swan-neck or boutonnière reconstructions. (Photographs © Copyright of Fraser J. Leversedge, Charles A. Goldfarb, and Martin Boyer.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access