Operative Management of PIP Dislocations and Fracture-Dislocations
Nikhil R. Oak
Brian Najarian
Jeffrey N. Lawton
BACKGROUND
Proximal interphalangeal (PIP) joint fracture-dislocations are intra-articular injuries that also include a concomitant soft-tissue injury to the surrounding ligamentous and capsular structures. These injuries most often occur from an axial load, but a bending torsional load or combined mechanism of injury can also occur. Injuries to the PIP joint are among the most common in the hand (1). Evaluation and treatment may be delayed as the injury can often be dismissed as a “jammed finger” (2). Swelling, stiffness, arthritis, and permanent pain can be the result of inadequate treatment of these injuries (3).
The head of the proximal phalanx is bicondylar and has almost complete articular congruency with the middle phalanx allowing for joint stability with axial loading (4). The PIP joint is crucial in our ability to grasp objects, contributing 85% of the total active motion necessary due to its unique anatomy with 110 degrees arc of motion (5,6). Stability in the flexion-extension arc is provided by the thick volar plate, proper and accessory collateral ligaments, checkrein ligaments, and joint capsule, which form a three-sided box with the dorsal aspect relatively devoid of stabilizing structures (6) (Fig. 9-1). The extensor complex plays a role in limiting volarly directed stresses. The precise anatomy of the joint allows for equal loading throughout motion; therefore, any subluxation or abnormalities in the joint can cause increased wear and arthritis (7).
CLASSIFICATION
The pattern of joint injury depends on the direction, degree, and rate of force application. Injuries to the middle phalanx can be classified based on the portion of the articular surface involved and the direction of deformity (Fig. 9-2).
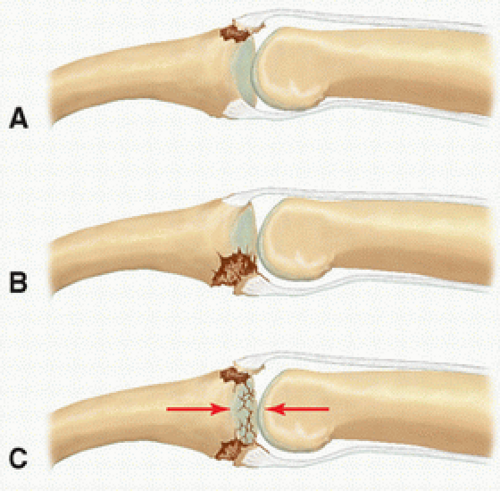
Palmar lip fractures with dorsal subluxation or dislocations of the middle phalanx are the most common type of injury. These injuries are caused by axial loading and hyperextension of the middle phalanx on the head of the proximal phalanx. Palmar lip fractures can be graded based on the percentage of articular surface involvement and joint subluxation (7,8,9). Stable fractures are those that remain reduced in extension with less than 30% of articular surface involvement. Tenuously stable fracture-dislocations are those that involve 30% to 50% of the articular surface with reduction of the
joint maintained with less than 30 degrees of flexion. Unstable fractures are those with greater than 50% of the articular surface involved or 30% to 50% involved but needing more than 30 degrees of flexion to maintain adequate reduction of the PIP joint (Fig. 9-3).
joint maintained with less than 30 degrees of flexion. Unstable fractures are those with greater than 50% of the articular surface involved or 30% to 50% involved but needing more than 30 degrees of flexion to maintain adequate reduction of the PIP joint (Fig. 9-3).
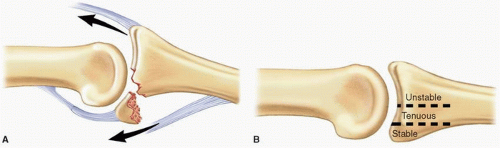
Dorsal lip fractures occur with palmar subluxation of the middle phalanx and can be caused by axial loading with hyperextension or an avulsion fracture by hyperflexion (10). Stable injuries are
those in which the joint remains reduced in extension. Unstable injuries are those demonstrating palmar subluxation of the middle phalanx with the joint in extension. Often, a disruption of the normal digital cascade accompanies palmar subluxations or dislocations.
those in which the joint remains reduced in extension. Unstable injuries are those demonstrating palmar subluxation of the middle phalanx with the joint in extension. Often, a disruption of the normal digital cascade accompanies palmar subluxations or dislocations.
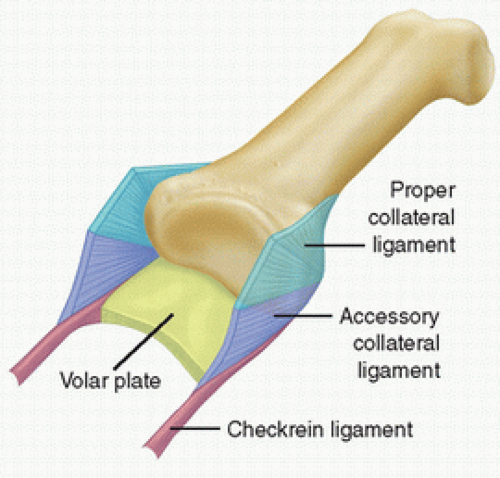 FIGURE 9-1 PIP joint anatomy. The thick volar plate, proper and accessory collateral ligaments, checkrein ligaments, and joint capsule form a three-sided box. |
Pilon fractures of the middle phalanx are those where the volar and dorsal margins are disrupted with comminution of the central articular surface (10,11). These fractures are caused by high-energy axial load with the joint in partial flexion and are almost always unstable. Commonly, dorsal and palmar fragments surround a depressed central fragment.
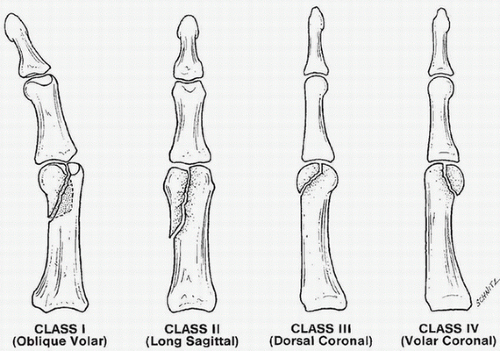
The proximal phalanx can also be involved in PIP fractures-dislocations. These injuries occur during an axial load through the tip of the finger. Proximal phalanx articular fracture patterns include unicondylar, bicondylar, or comminuted fractures. Unicondylar fractures can be classified into four basic groups: oblique volar, long sagittal, dorsal coronal, and volar coronal (12) (Fig. 9-4).
INDICATIONS
It is important to promptly recognize the complexity of the initial injury and to understand appropriate treatment options. Most PIP dislocations and fracture-dislocations can be treated with closed reduction, splinting, early motion, and close follow-up. Open treatment of PIP joint dislocations or fracture-dislocations is indicated when the joint cannot be concentrically reduced or if the reduction cannot be maintained by closed methods. Open reduction is also indicated in open displaced fractures and most unstable fractures that present after a remote trauma. Unstable or tenuous fractures include those that require more than 30 degrees of flexion to maintain reduction. Attempting closed management of a fracture-dislocation that would require extreme flexion to prevent redislocation will likely result in a significant flexion contracture. Other indications for open reduction include significant articular depression, displacement, or joint incongruity. An irreducible joint is consistent with entrapment of a soft-tissue structure such as the volar plate, collateral ligament, and/or tendons in the joint, which necessitate surgical extraction prior to reduction. There are no absolute contraindications to surgical treatment of these injuries other than a medically unstable patient or inability of the patient to cooperate with operative treatment and postoperative rehabilitation.
The goals of treating PIP joint fracture-dislocations include obtaining concentric joint reduction, restoring a stable arc of motion, and allowing early motion to minimize adhesions and contractures (11). If full stable extension is achieved, recovery is much simpler as regaining/correcting PIP joint extension is far more difficult than regaining/correcting flexion. Anatomic restoration is desirable but not as important as the above outlined goals (10,13).
PREOPERATIVE PREPARATION
Presentation and Evaluation
After injury, the PIP joint quickly stiffens. Pain and instability will limit motion in the acute period following injury. Subacute or chronic injuries will present with stiffness, loss of function, persistent swelling, and pain due to the fibrosis of the capsular and ligamentous structures of the joint.
An adequate history must be obtained, which includes a detailed description of the mechanism of injury and any previous treatments. The neurovascular exam is generally normal; however, capillary refill and sensation should be documented. Skin and soft tissues should be inspected particularly at the level of the PIP flexion crease for any open or healed wounds that would indicate an open fracture-dislocation. Deformity noted in extension or flexion can indicate a volar or dorsal dislocation. Location and extent of swelling or tenderness can indicate which soft-tissue structures are injured. Attention should be paid to both axial and rotational alignments, which may be altered secondary to articular depression of a condyle. This can be recognized clinically as angulation when full digital flexion and extension is attempted. Passive and active range of motion should also be documented, including any deficits. A digital nerve block may be necessary for a thorough exam (5). Passive testing of joint stability can allow for the assessment of volar plate and collateral ligament integrity; subluxation during active range of motion suggests ligament disruption or a significant intra-articular fracture (1). It is important to note the range of motion through which the joint remains reduced. For dorsal dislocations, the degree of extension that results in instability or dislocation determines the angle for extension block splinting or pinning.
Elson’s test (14) can be performed to evaluate the integrity of the central slip of the extensor apparatus. From a 90-degree flexed position of the PIP joint, the patient can be asked to actively extend the PIP against resistance. If the central slip is still intact, the force will be demonstrated through the middle phalanx and the distal interphalangeal (DIP) joint will remain supple during this effort. If the DIP joint remains rigidly extended due to the compensatory extensor actions of the lateral bands alone, a complete rupture of the central slip can be documented. In an acute setting, the patient may need a local digital block to allow for a good effort.
Diagnostic Studies
After clinical examination, radiographic views including posteroanterior (PA), lateral, and oblique views of the digit are required. Oblique views are helpful in identifying fracture planes and to judge the extent of fracture comminution. Radiographs can be misleading as a seemingly small fragment of bone may result in incompetence of structures that lead to joint instability. A postreduction true lateral is needed to determine the amount of articular involvement, and views in full PIP joint extension are used to evaluate the stability of the joint. With superimposition of the proximal phalangeal condyles, subtle subluxation of the middle phalanx can be detected. Dorsal subluxation of the joint produces the “V” sign caused by separation of the incongruous articular surface of the proximal phalanx head and undamaged portion of the middle phalanx base. Presence of the “V” sign indicates subtle joint instability (11) (Fig. 9-5). Dynamic fluoroscopy, when available, can also be very helpful in evaluating joint reduction and stability.
Palmar Lip Fractures Stable fractures maintain joint congruency in full PIP extension, tenuous fractures stay reduced with less than 30 degrees of flexion, and unstable fractures need more than 30 degrees of flexion to maintain joint congruency (4,5,10,11).
Dorsal Lip Fractures Stability is assessed in full extension. Articular surface involvement is usually less than 50% when stable, but if there is any palmar subluxation in full extension or concern for central slip rupture, these fractures are deemed unstable (5,10).
Pilon Fractures All pilon fractures are grossly unstable and involve up to 100% of the articular surface. They often have areas of central depression and peripheral comminution and have the greatest amount of joint disruption (4).
Condylar Fractures Fractures of the head of the proximal phalanx also undergo the same workup as middle phalangeal base fractures. PA radiographs are beneficial to visualize articular step-off. Type I fractures have an oblique volar fracture pattern, which renders it highly unstable. These fractures can create both lateral angulation and rotational misalignment. Type II fractures have a long oblique fracture line in the sagittal plane, which also renders it unstable. Type III fractures have a dorsal coronal fragment, which is usually small and can be associated with a dorsal PIP joint dislocation. Type III fractures are often stable and can be treated with fragment excision unless the fracture involves greater than 50% of the condylar diameter in the PA plane. Type IV fractures have a palmar coronal fragment and can be associated with a volar PIP joint dislocation. These fragments are unstable and can interfere with flexion.
TECHNIQUES
Closed Reduction
Most PIP joint dislocations and fractures can be treated with closed reduction. This is almost always successful for acute dorsal PIP dislocations. Volar dislocations can be more problematic especially if there is a rotatory component to the deformity.
Reductions can be performed immediately after injury or if in a delayed presentation with the help of a 1% lidocaine digital block.
Complete a neurologic exam of the digit prior to block and confirm adequate anesthesia before the reduction maneuver.
Dorsal dislocations—apply gentle traction on the finger with the wrist in neutral position followed by a volar directed force on the base of the middle phalanx while holding the proximal phalanx steady.
Volar dislocations
Without rotatory component—place wrist in neutral position and apply gentle longitudinal traction with a dorsally directed force to the middle phalanx and a volarly directed force on the proximal phalanx.
With rotatory component—often more difficult to reduce as the head of the proximal phalanx becomes entrapped between the central slip and one of the lateral bands of the extensor mechanism. Attempt reduction by placing the metacarpophalangeal (MCP) and PIP joints in 90 degrees of flexion with wrist extension and apply light traction to the digit while rotating the middle phalanx in the direction opposite to the deformity.
Open Reduction: Positioning/Equipment
Patient is placed supine with a radiolucent hand table.
Brachial or forearm tourniquet can be placed prior to draping—can be inflated to 250 mm Hg after exsanguinating the arm prior to incision.
Surgery can be performed under general or regional anesthesia. Axillary blocks can achieve adequate sensory anesthesia and motor relaxation of muscle groups.
Supinate the operative hand. Optionally, it can be held in place with a “lead hand” malleable positioner.
Mini C-arm fluoroscopy is utilized to assess and confirm fracture/joint reduction.
Depending on the technique used—minifragment plate/screw set, 24-gauge cerclage wire, and/or Kirschner (K)-wires should be available.
Closed Reduction and Percutaneous Pinning
When acute fractures are reducible by closed means and an anatomic reduction can be achieved, this can be maintained by percutaneous K-wire fixation.
Fractures involving the articular surface can be compressed together by using a fracture reduction forceps externally.
Mini C-arm is used to assess fracture reduction with a goal being an anatomic joint surface and congruent PIP joint.
Reduction is then secured using percutaneous K-wires—a minimum of 2 is required to prevent redisplacement.
Either 0.045- or 0.035-inch K-wires can be used based on the size of the fracture and the phalanx.
Optimal fixation points in the proximal phalanx are distal and palmar as the central and dorsal regions have thin cortical elements and provide weaker fixation.
For condylar fractures (9):
K-wires are inserted from the contralateral dorsal side of the intact condyle and advanced palmarly into the fractured condyle. Holding the PIP joint in extension relaxes the conjoined lateral bands.
K-wires may also be inserted from the palmar/lateral fractured fragment and advanced to the intact condyle.
A towel clip can be used to reduce the volar fragment with one point placed percutaneously into the middorsal base of the middle phalanx and other point percutaneously through the midline of the flexor tendons directly onto the volar fragment.
The K-wire is manually inserted through the skin just lateral to the volar limb of the towel clip distal to the articular surface.
The K-wire can then be drilled across the dorsal cortex of the middle phalanx and through the dorsal skin. This is then repeated on the other side of the volar lip so that two wires are now entering the volar fragment and exiting dorsally through the skin.
The K-wires can be withdrawn from the dorsal side until almost flush with the volar fracture fragment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree