Operative Exposure
Jeffry T. Watson
Richard H. Gelberman
Martin I. Boyer
External Fixation for Distal Radius Fractures
External fixation is a well-established method of treatment for fractures of the distal radius. Several different systems are available, but all use bony fixation points in the shaft of the radius and in the index metacarpal. The fixator is placed along the dorsoradial plane of the radius. The ideal interval for proximal pin placement is the space between the extensor carpi radialis longus and the brachioradialis tendons.
The superficial branch of the radial nerve is at risk of injury in this procedure, lying deep to the muscle and emerging from inter the brachioradialis tendon approximately 6 cm proximal to the radial styloid. Additionally, terminal branches of the lateral antebrachial cutaneous nerve lie subcutaneously in this region and are vulnerable to injury. Percutaneous placement of external fixator pins in the radius is ill advised, as it carries the risk of painful neuroma formation and irreversible loss of sensation distally.
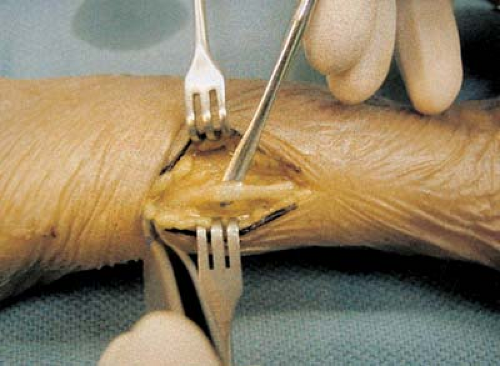
The authors prefer an open approach to the radial shaft for the placement of the proximal fixator pins. This allows the superficial radial nerve to be identified directly. Make a longitudinal incision on the lateral side of the radial shaft, approximately 5 cm proximal to the fracture (Fig. 1-1). Identify branches of the lateral antebrachial cutaneous nerve during subcutaneous dissection down to the forearm fascia, and retract them. Identify the tendons of brachioradialis and extensor carpi radialis longus (the extensor carpi radialis longus can be differentiated from the brachioradialis by observing its excursion with wrist flexion and extension).
Open the fascia overlying the interval and identify the superficial radial nerve, as it lies deep or immediately radial to the tendon of brachioradialis (Fig. 1-2). Dissect the superficial radial nerve free throughout the length of the incision, and retract it. Use Hohmann or right-angle retractors to retract the soft tissues, and place the fixator pins in the radius under direct visualization.
Either one or two incisions may be used along the dorsolateral or lateral aspect of the index metacarpal for placement of the two distal pins of the external fixator. Because it is possible to encounter terminal branches of the superficial radial nerve, we recommend direct visualization of the index metacarpal for the placement of both distal pins. Identify the metacarpal shaft immediately dorsal to the origin of the first dorsal interosseous muscle. Place the fixator pins into the bone under direct visualization. Close all skin incisions before assembling the fixator apparatus.
Dorsal Approaches
Dorsal Longitudinal Approach
The dorsal longitudinal approach provides access to the entire dorsal aspect of the carpus, distal radius, distal radioulnar joint (DRUJ), ulnar head, and ulnocarpal joint. We use this approach frequently for the treatment of acute fractures or osteotomy of the distal radius, management of triangular fibrocartilage complex and DRUJ disorders, carpal ligament repair or reconstruction, intercarpal or total wrist arthrodesis, and total wrist arthroplasty. It allows extension proximally for exposure of the dorsal radial diaphysis and distally for access to the metacarpals. (Figs. 1-3, 1-4, 1-5, 1-6, 1-7 and 1-8).
Because the areolar tissue along the dorsal aspect of the wrist is loose, longitudinal scar contracture is of minimal consequence and does not limit wrist flexion. Start the utilitarian straight dorsal incision proximally over the central portion of the distal radius, proximal to Lister’s dorsal radial tubercle. Continue the incision distally in line with the radius and the long-finger metacarpal (Fig. 1-9). Spread the subcutaneous tissue bluntly, and raise full-thickness skin flaps, exposing the extensor retinaculum (Fig. 1-10).
Familiarity with the location of the sensory branches of both the radial and the ulnar nerves on the dorsal wrist will aid in early identification of these structures after the skin is incised (Fig. 1-11). The sensory branch of the radial nerve becomes subcutaneous 5 to 10 cm proximal to the radial styloid, in the interval between the brachioradialis and extensor carpi radialis longus tendons. It bifurcates into two main branches before reaching the radiocarpal joint. The dorsal branch passes within 1 to 3 cm of the radial side of Lister’s tubercle and continues distally to supply the first and second web spaces.
The palmar branch passes within 2 cm of the first dorsal compartment and provides sensory innervation to the dorsolateral aspect of the thumb after passing directly over the extensor pollicis longus tendon. The dorsal cutaneous branch of the ulnar nerve arises from the ulnar nerve deep to the flexor carpi ulnaris tendon and becomes subcutaneous on the ulnar border of the forearm, approximately 5 cm from the proximal border of the pisiform. Branching of the nerve can begin
proximal or distal to the ulnar head, and the nerve usually passes directly over its medial aspect, as well as the dorsal aspect of the triquetrum and hamate. Anatomic dissections have identified communicating branches between the ulnar and radial dorsal sensory branches.
proximal or distal to the ulnar head, and the nerve usually passes directly over its medial aspect, as well as the dorsal aspect of the triquetrum and hamate. Anatomic dissections have identified communicating branches between the ulnar and radial dorsal sensory branches.
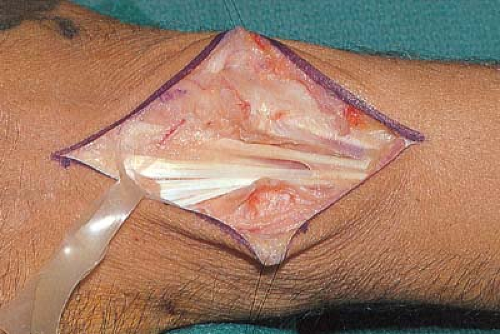 Figure 1-4 The extensor retinaculum is incised longitudinally, exposing the extensor digitorum communis tendons and the extensor indicis proprius tendon. |
 Figure 1-7 Following decortication, a dorsal plate is applied from the long finger metacarpal to the radius. |
 Figure 1-8 Following closure of the dorsal capsule and extensor retinaculum, the skin is closed with horizontal mattress sutures over a closed suction drain. |
 Figure 1-10 The subcutaneous tissue has been spread bluntly, exposing the dorsal aspect of the extensor retinaculum. |
Surgical procedures involving tenosynovectomy or tendon transfer involving the digital extensor tendons are best approached directly through the fourth dorsal compartment. Procedures involving the distal radioulnar joint or the triangular fibrocartilage complex are most effectively approached through the fifth dorsal compartment. The majority of other surgical procedures carried out on the distal radius and carpus are conveniently approached through the third dorsal compartment.
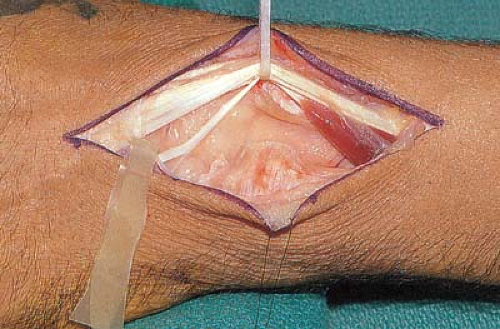
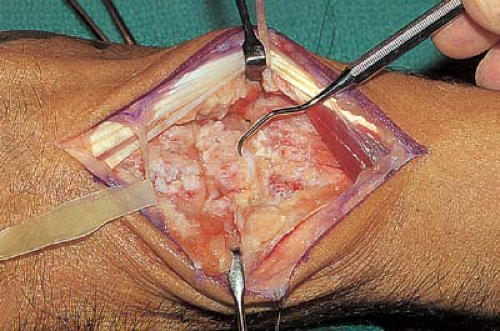
With passive motion of the thumb and the fingers, identify the interval between the extensor pollicis longus (third compartment) and the extensor digitorum communis (fourth compartment), and sharply incise the retinaculum directly overlying the third compartment. Mobilize the extensor pollicis longus tendon proximally and distally, then retract it laterally. Then, dissect the infratendinous retinaculum of the fourth dorsal compartment either from the underlying dorsal wrist capsule as a separate layer, or subperiosteally, along with the dorsal capsule, as a combined layer (Figs. 1-12, 1-13, 1-14 and 1-15).
Continue dissection subperiosteally to expose the distal radius radially as far as the tip of the radial styloid, and ulnarly to the dorsal capsule of the distal radioulnar joint. Preserve the dorsal distal radioulnar ligaments to prevent subsequent instability. Incise the dorsal capsule longitudinally over the carpal bones to elevate full-thickness capsular flaps medially and laterally. Take care to avoid injury to the dorsal aspects of the scapholunate and lunotriquetral interosseous ligaments during the elevation of the dorsal capsular flaps. Identify the extensor carpi radialis tendon along the dorsal proximal base of the long-finger metacarpal, and retract it radially with the capsular flap. Do not detach it from its insertion (Figs. 1-16 and 1-17).
On completion of the surgical procedure, close the wound in anatomical layers. Close the dorsal wrist joint capsule with 2–0 braided nonabsorbable suture material, using interrupted figure-of-eight sutures. The extensor pollicis longus tendon is not replaced within its sheath and lies transposed radially deep to the subcutaneous tissue. In our experience, this situation does not lead to postoperative loss of thumb extension. Close the subcutaneous tissue with 4–0 absorbable suture and the skin with interrupted horizontal mattress sutures of 4–0 or 5–0 monofilament (Figs. 1-18 and 1-19).
Extensor tenosynovectomy or tendon reconstruction requires entry into the fourth compartment. To isolate proximal and distal retinacular flaps, make transverse incisions along the distal and proximal borders of the extensor retinaculum, taking care not to damage the tendons underneath. Carry out exposure of the digital extensor tendons by elevating the distal portion of
the extensor retinaculum as a radially based flap and the proximal portion as an ulnarly based flap. This technique facilitates retinacular closure when tenosynovectomy or tendon reconstruction is completed. If a smooth gliding surface must be restored deep to the extensor tendons, one flap of the extensor retinaculum may be passed deep to the tendons during closure (Figs. 1-20, 1-21, 1-22, 1-23, 1-24, 1-25, 1-26



the extensor retinaculum as a radially based flap and the proximal portion as an ulnarly based flap. This technique facilitates retinacular closure when tenosynovectomy or tendon reconstruction is completed. If a smooth gliding surface must be restored deep to the extensor tendons, one flap of the extensor retinaculum may be passed deep to the tendons during closure (Figs. 1-20, 1-21, 1-22, 1-23, 1-24, 1-25, 1-26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree