in the coronal plane due to advanced medial plateau concavity. This finding indicates that it will not be possible to significantly unload the medial compartment, and a majority of the weight-bearing loads will be confined to the medial compartment. Marked patellofemoral symptoms contraindicate an HTO. Medical contraindications include diabetes, rheumatoid arthritis, autoimmune diseases, and malnutrition states.
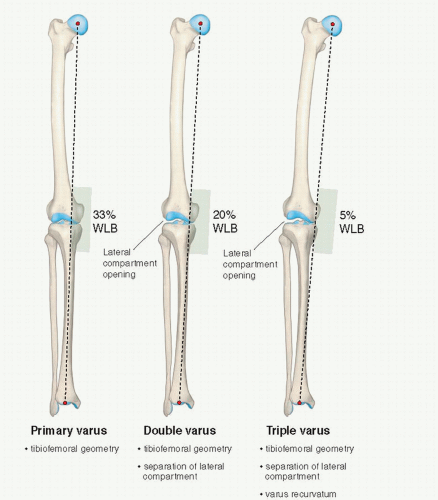
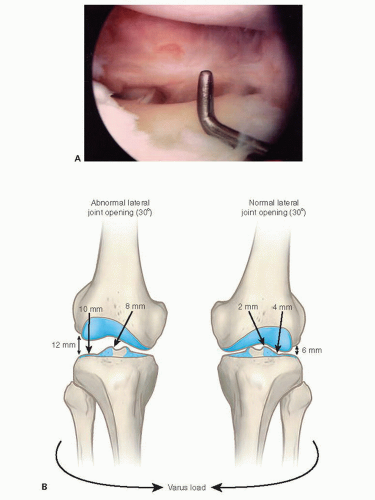
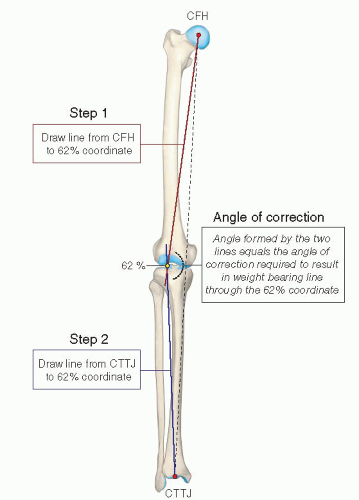
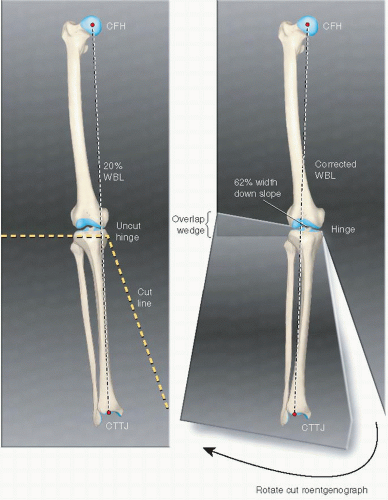
If separation of the lateral tibiofemoral joint is observed, it is necessary to subtract the lateral compartment opening so that the true tibiofemoral osseous alignment is determined and a valgus overcorrection is avoided. Other radiographs include a lateral at 30° knee flexion, weight-bearing posteroanterior at 45° knee flexion, and patellofemoral axial views. Telos medial or lateral stress radiographs may also be required of both knees. The height of the right and left patella is measured on lateral radiographs to determine if an abnormal patella infera or alta position exists (1).
Table 76.1 Preoperative planning | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
slope is required before cruciate ligament surgery or other conditions discussed. Empirically, a tibial slope greater than two standard deviations above normal (e.g., a tibial slope of 15° or greater) usually requires correction.
between the tibial tubercle and the posteromedial tibial cortex, starting 1-cm inferior to the joint line. Once the dissection is complete, a Keith needle is placed in the anteromedial joint just above the tibia, and the distance is marked on the desired point of the osteotomy along the anteromedial cortex. A second Keith needle is placed at the posteromedial tibial joint space, and the same millimeters are marked to provide a measurement of the tibial slope. The two marks are connected to provide the osteotomy line perpendicular to the tibial slope.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree