Opening Wedge Thoracoplasty and Vertical Expandable Prosthetic Titanium Rib Insertion for Congenital Scoliosis and Fused Ribs
Robert M. Campbell Jr.
DEFINITION
This procedure lengthens the concave constricted hemithorax through a vertical expandable prosthetic titanium rib (VEPTR) expansion thoracoplasty with indirect correction of congenital scoliosis to maximize the potential for thoracic growth in order to benefit the growth of the underlying lungs.
ANATOMY2
Congenital scoliosis and fused ribs is a severe variant of congenital scoliosis.
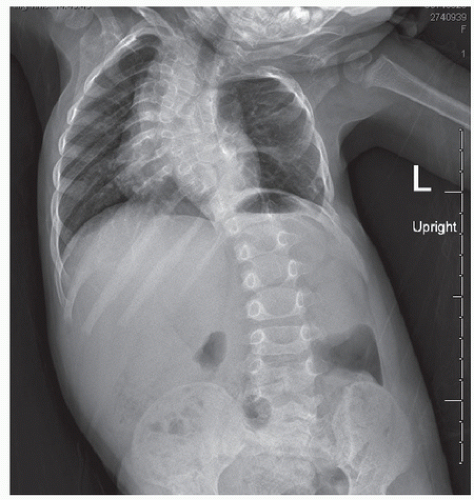
Long unilateral unsegmented bars are common on the concave side of the curve with multiple contralateral hemivertebrae (FIG 1).
The extent of rib fusion is commonly extensive, usually concentrated on the concave side of the curve, and, when adjacent to the spine, can contribute to curve progression through tethering.
Mixed deformities are also seen, with areas of absent ribs adjacent to areas of fused ribs.
Both the height and width of the concave fused hemithorax is often diminished, with reduction in height of the entire thorax common from multiple congenital anomalies of the thoracic spine.
All these anomalies combine to reduce overall thoracic volume.
This variant is classified as a type II volume depletion deformity of the thorax.1
PATHOGENESIS
Congenital scoliosis is associated with haploinsufficiency of the Notch signaling pathway genes8 and the more severe variant spondylocostal dysostosis is associated with DLL3 mutations.4
Fused ribs and congenital scoliosis is a widespread “failure of segmentation” involving both spine and rib cage and is most commonly seen in conditions such as VACTERL (vertebral anomalies, anal atresia, cardiovascular anomalies, tracheoesophageal fistula, esophageal atresia, renal or radial anomalies, limb anomalies) syndrome or spondylocostal dysostosis but can also occur as an isolated anomaly.
NATURAL HISTORY
Severe congenital scoliosis with fused ribs often progresses rapidly without treatment, with growth inhibition of the lung on the concave side of the curve.
Early extrinsic restrictive lung disease from the constrictive effects of the severe spine and rib cage anomalies may be clinically masked in the young child by elevation in resting respiratory rate and reduction in play activities to aid overall body oxygenation, but as the youngster becomes older, a high respiratory rate becomes difficult to sustain and early respiratory insufficiency develops.
Clinically, sleep disturbances are usually first seen, then frank clinical daytime dyspnea may develop with the need for respiratory assistance such as nasal oxygen, continuous positive airway pressure (CPAP)/bilevel positive airway pressure (BIPAP), or even ventilator support. Untreated infantile scoliosis patients begin to experience increased mortality from respiratory failure after age 20 years, with a death rate three times normal by age 60 years,6 but the longterm mortality in untreated congenital scoliosis and fused ribs is unknown.
PATIENT HISTORY AND PHYSICAL FINDINGS
The clinical assessment should include both general and pulmonary health.
Onset of radiologic and clinical scoliosis should be determined; clinical course and response to treatment recorded.
Details about any prior spine surgery are important to note because that may affect growth potential of the spine.
A respiratory history should include determination of the frequency of colds, bronchitis, and pneumonias due to bacterial origins or viral etiology such as respiratory syncytial virus (RSV). Increasing frequency of respiratory illnesses, need for hospitalization for them, or the need for ventilatory assist to recover from them is worrisome and suggests developing respiratory insufficiency.
Voluntary reduction in play activities by the child, gradually lowering them to the point where aerobic demands are minimal, also is an early sign of respiratory insufficiency. An extensive review of related body systems is important.
Congenital heart disease can contribute to clinical respiratory insufficiency and cor pulmonale can be life-threatening.
Gastrointestinal (GI) abnormalities such as gastroesophageal reflux disease (GERD) may cause aspiration pneumonia.
Congenital renal abnormalities are seen in a third of congenital scoliosis patients.
Abnormal bowel and urinary incontinence should be documented and neural cause investigated.
Physical examination should include measurement of percentile weight/height and resting respiratory rate.
Low weight is common in children with thoracic insufficiency syndrome and may be related to the increased work of rapid breathing.7
Normal respiratory rate is 60 to 80 breaths per minute in the first year of life, declining to 20 to 24 breaths per minute by age 4 to 6 years.5
Nasal flaring suggests labored breathing.
Perioral cyanosis or clubbing of the fingertips implies hypoxia.
Unequal shoulder heights, head and truncal decompensation as well as any leg limb inequality are measured.
Adams forward bend test is used to observe rotation of the back on the convex side of the curve. Isolated rib prominences and any generalized abnormal shape of the chest is noted, including pectus carinatum or excavatum.
Rib defects are measured, and clinical instability is estimated by degree of collapsing inward paradoxical motion with respiration. Areas of stiff chest wall over fused ribs are measured and location recorded. Chest circumference at the nipple line is measured and normal percentile determined.
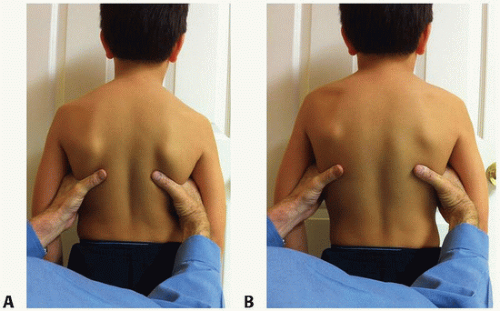
A thumb excursion test (FIG 2) is done. From the back, the hands are placed lightly on each side of the chest with the thumbs extended medially, equidistant from the spine. The patient takes a deep breath, with chest expansion moving each hand outward with the tips of the thumbs moving away from the spine.
In normal individuals, the thumbs move out symmetrically with deep respiration, but with chest wall stiffness, the thumbs barely move with breathing.
The motion is graded: +3 is greater than 1 cm motion outward, +2 is 1 to 0.5 cm motion, +1 is less than 0.5 cm, and +0 is no movement. The patient is also assessed for a marionette sign.1
With respiration, the patient’s head bobs up and down, much like that of a marionette puppet.
This is a positive sign, suggesting that the diaphragm is encountering resistance to downward excursion with inspiration, common in spine deformity, and in essence, the diaphragm is doing a “push-up” against body weight to fully expand the lung.
This is a high-energy expenditure and is not sustainable over time, leading to respiratory failure.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Weight-bearing anteroposterior (AP) and lateral radiographs of the spine, including the entire chest as part of the radiographs should be obtained, along with supine lateral bending films of the spine.
AP and lateral radiographs of the C-spine with flexion/extension laterals should be obtained. Computed tomography (CT) scan of the chest and lumbar spine, 5-mm intervals, and an unenhanced magnetic resonance imaging (MRI) of the entire spinal cord is obtained.
Dynamic lung MRI (FIG 3) is helpful in visualizing functional impairment of the thorax.
Pulmonary function tests by spirometry for patients older than age 6 years and infant pulmonary function tests for younger patients, if available. Complete blood count (CBC), sedimentation rate, C-reactive protein (CRP), electrolytes, prothrombin time (PT), and partial thromboplastin time (PTT) are also obtained.
DIFFERENTIAL DIAGNOSIS
Infantile scoliosis
Congenital scoliosis without rib fusion
Scoliosis associated with arthrogryposis
NONOPERATIVE MANAGEMENT
Observation with serial radiographs is indicated for mild or even moderate curves.
Bracing is ineffective for congenital scoliosis.
Progression requires operative intervention.
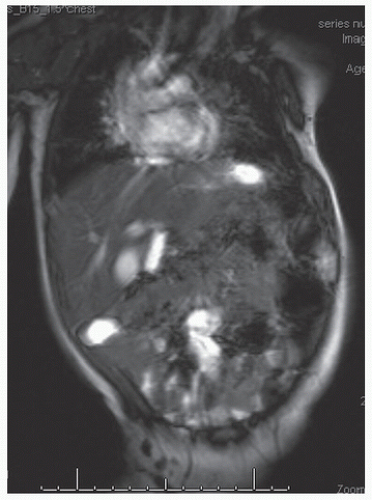 FIG 3 • A dynamic lung MRI was performed and showed complete absence of rib cage expansion in inspiration and marked decrease in downward excursion of each respective hemidiaphragm during respiration.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|