Opening-Wedge Proximal Tibial Osteotomy
Michael J. Stuart
INTRODUCTION
Limb malalignment results in an imbalance of force transmission to the knee joint. A varus deformity is most common, because osteoarthritis typically involves the medial compartment. Articular cartilage, bone, and medial meniscus loss combined with lateral collateral ligament stretching cause an increased tibial condylar-plateau angle. The resultant load concentration at the medial portion of the joint contributes to arthritis pain.
A valgus-producing tibial osteotomy can redistribute the weight-bearing forces, lessen the medial compartment load, and reduce the varus knee moment. The goals of this procedure are to relieve pain, buy time before an arthroplasty is necessary, and decrease forces on ligament, meniscus, and osteochondral grafts. Unicompartment or total knee arthroplasty have supplanted realignment osteotomy as a primary treatment for many middle-aged patients with gonarthrosis. However, the indications for an osteotomy have actually broadened to include younger patients or athletes with ligament deficiencies, chondral defects, absent menisci, or post-traumatic degenerative arthritis. An osteotomy should also be performed in combination with ligament reconstruction, articular cartilage regeneration, or meniscal transplantation in a knee with associated limb malalignment.
The lateral closing-wedge osteotomy of the proximal tibia was popularized by Coventry in the 1960s (1,2). Appropriate patient selection and sufficient postoperative correction have been correlated with a 90% success rate at more than 10 years after surgery (3, 4, 5). Worsening of results is caused by recurrent pain, arthritis progression, and occasionally, recurrence of varus deformity (6). In recent years, a medial opening-wedge osteotomy of the proximal tibia has gained popularity as new instrumentation and implants have become available (7, 8, 9).
The advantages of the opening-wedge technique include:
no violation of the proximal tibiofibular joint
no change in the fibular collateral ligament length
a more precise intraoperative correction
easier biplanar correction
same incision for concomitant procedures (anterior cruciate ligament reconstruction, osteochondral allografts, etc.) or subsequent knee arthroplasty
avoidance of metaphyseal-diaphyseal offset deformity common in closing-wedge proximal tibial osteotomy
Disadvantages of the opening-wedge technique include:
lengthening of the patellar tendon and elevation of the tibiofemoral joint line (10)
increased tension in the medial collateral ligament (MCL)
distal translation of the patella and lateral translation of the tibial tubercle
bone graft requirement
slower healing and longer protection from weight bearing
INDICATIONS
A valgus-producing osteotomy of the proximal tibia is primarily indicated for pain relief in patients with medial compartment arthritis and/or mechanical axis correction as an adjunct to other reconstructive knee procedures. Patients should have pain and tenderness localized to the medial joint line, less than 10 degrees of terminal knee extension loss, and greater than 90 degrees of knee flexion. Osteotomy can be performed in patients with:
varus mechanical axis and medial unicompartmental tibiofemoral arthrosis
chronic posterolateral instability and varus thrust
varus mechanical axis and anterior or posterior cruciate ligament reconstruction
varus mechanical axis and meniscus transplantation
varus mechanical axis and subchondral bone microfracture, autologous chondrocyte implantation, or osteochondral transplantation
CONTRAINDICATIONS
Osteotomy should be avoided in patients with (11):
diffuse knee pain and tenderness
knee stiffness (greater than 10 degrees of terminal knee extension loss and/or less than 90 degrees of knee flexion)
bicompartmental or tricompartmental arthritis
severe deformity
medial tibial bone loss
pronounced joint line obliquity
lateral tibial subluxation
varus angulation of the proximal tibia combined with excessive valgus angulation of the distal femur
uncorrected ligamentous laxity and functional knee instability
obesity
previous meniscectomy in contralateral compartment
inflammatory arthropathy
unrealistic patient expectations
PREOPERATIVE PLANNING
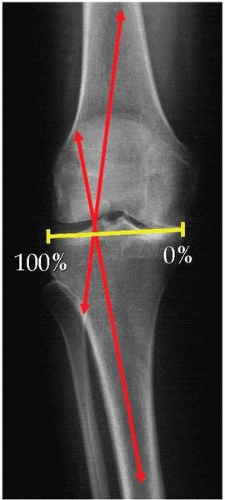
Gait observation and physical examination of the knee will identify a lateral thrust and pathologic collateral ligament laxity that may not be apparent on standing radiographs. The desired angle of correction is determined by static analysis of full-length standing roentgenograms (51 × 14 inches). The mechanical axis of the limb is the angle formed between a line drawn from the hip center to the knee center (femoral mechanical axis) and a line drawn from the knee center to the ankle center (tibial mechanical axis). The normal mechanical axis is approximately 1.2 degrees of varus (12). A valgus-producing proximal tibial osteotomy performed for medial compartment arthritis typically overcorrects the mechanical axis to 3 to 5 degrees of valgus. The Weight-Bearing Line Method is a simple and reproducible technique for determining the desired coronal plane correction angle (Fig. 27-1) (13).
Divide the lateral tibial plateau from 0% to 100% from the medial to the lateral margin.
Draw lines from the center of the femoral head and the center of the tibiotalar joint to the desired coordinate depending on the indication for the procedure (typically 62% [range, 50% to 75%]).
The angle formed by these two lines equals the angle of correction.
The use of standing radiographs can overestimate the magnitude of correction because of osseous defects and/or attenuated ligaments. Each millimeter of lateral tibiofemoral joint separation
causes approximately 1 degree of varus angular deformity. Compare the amount of lateral joint space opening (in millimeters) with the contralateral knee and subtract the difference from the calculated angle (1 degree per mm) to avoid overcorrection.
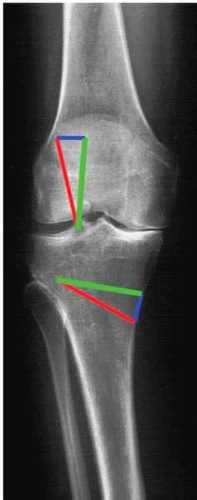
Once the desired angle of correction has been calculated, determine the medial tibial opening in millimeters by measuring “like triangles” on the film (Fig. 27-2) or by performing a cutout using tracing paper.
Study the lateral radiograph to appreciate the sagittal plane geometry of the tibial plateau. The osteotomy should maintain a neutral tibial slope, unless a sagittal plane correction is desired. Increase in the posterior tibial slope will cause excessive anterior cruciate ligament graft strain but may be advantageous for a posterior cruciate ligament-deficient knee. Increase in the anterior tibial slope will cause excessive posterior cruciate ligament graft strain but may be desired in an anterior cruciate ligament-deficient knee.
SURGICAL TECHNIQUE
Setup:
Place the patient supine on a radiolucent operating room table. Check the fluoroscope to ensure clear visualization of the femoral head, knee, and talus.
Exposure:
Exsanguinate the leg and inflate the tourniquet. Make a vertical incision, centered midway between the tibial tubercle and the posteromedial border of the tibia, beginning 1 cm distal to the joint line extending distally for approximately 7 cm (Fig. 27-3). Split the sartorius fascia diagonally between its fibers and identify the superficial MCL (Fig. 27-4). Retract the gracilis and semitendinosus tendons distally or transect the tendons for later repair. Incise the superficial MCL distally, subperiosteally elevate, but preserve the proximal 2 cm of its tibial attachment. Flex the knee to 90 degrees and extend the subperiosteal dissection along the anterior and posterior tibial cortices. Place a malleable or Z retractor along the posterior tibial cortex to protect the neurovascular structures and along the anterior tibial cortex to protect the patellar tendon (Fig. 27-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree