Open Reduction and Internal Fixation of the Patella
Samir Mehta
DEFINITION
The patella, the largest sesamoid bone, is an essential component for knee extension (in conjunction with the patellar and quadriceps tendons) and provides leverage to the quadriceps mechanism. Fractures of the patella have the potential to disrupt the extensor mechanism.
Fractures of the patella can impact knee function, as these are often articular injuries.
Management of patellar fractures must restore any disruption to the extensor mechanism while ensuring minimal disruption of the articular surface.
Descriptive terms (stellate or comminuted, transverse, vertical, apical or inferior pole, and sleeve) are used to classify patellar fractures.
ANATOMY
The articular surface is composed of medial and lateral facets, with the medial facet having the most variability in size and shape. Horizontal ridges further subdivide the medial and lateral facets. An odd facet lies at the most medial aspect of the articular surface. The undulating nature of the articular surface can make interpretation of the lateral radiograph difficult. The distal pole of the undersurface is extra-articular, which is an important consideration when addressing injuries in this region (FIG 1).
The superior pole of the patella serves as an attachment for the quadriceps tendon. The most superficial portion of the quadriceps tendon courses over the anterior patellar surface and is contiguous with the patellar tendon. The patellar tendon courses from the apex of the patella to the tibial tubercle.
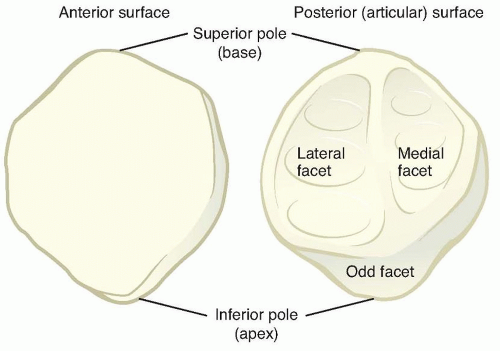
FIG 1 • Patellar anatomy. The major facets include the medial, lateral, and odd facets. The medial and lateral facets are further subdivided by subtle horizontal ridges.
The patellar retinaculum is composed of thickenings of the fascia lata of the thigh in addition to the aponeurosis of the vastus medialis and lateralis.15 In addition to stabilizing the patella, the retinaculum acts as a secondary extensor. An intact retinaculum in the setting of a displaced patellar fracture may allow for extension of the knee. The retinaculum is often torn in conjunction with an extensor mechanism injury.
Multiple arteries about the knee supply a peripatellar plexus, although the main intraosseous blood supply is from a distal to proximal direction.16
The patella acts to increase the moment arm of the extensor mechanism by displacing the quadriceps tendon anteriorly. This increased moment arm is most critical during terminal extension, when the quadriceps is otherwise at a mechanical disadvantage.9
Due to the small contact area of the articular surface and the high level of compressive forces generated by the extensor mechanism, the contact stress on the patellofemoral joint has been estimated to be higher than any other major weight-bearing joint.5
PATHOGENESIS
Fractures of the patella may result from direct force to the anterior knee, indirect forces transmitted through the extensor mechanism, or a combination of both.
The patella is particularly susceptible to injury from direct blows given its superficial location and minimal soft tissue envelope.
The portion of the patella articulating with the femur moves from distal to proximal with increasing degrees of flexion.
The fracture pattern for direct blows to the patella has been shown to correspond to the articulating portion of the patella at the time of injury, thus corresponding to the amount of knee flexion at time of injury.1
Indirect forces causing fracture can be caused by unanticipated and rapid flexion of the knee while the quadriceps is also firing. Fractures from an indirect mechanism tend to be less comminuted than those from direct trauma.5
NATURAL HISTORY
Depending on the type of fracture and involvement of the retinaculum, various amounts of long-term extensor lag and weakness can be expected. The long-term effect on range of motion likewise depends on fracture pattern and displacement.
There is an increased incidence of osteoarthritis of the knee after patellar fracture. The increased rate of arthritis may be both from initial cartilage injury and posttraumatic arthritis due to articular cartilage incongruity. Despite advances in techniques and technology, outcomes after operative fixation still show functional impairment.
PATIENT HISTORY AND PHYSICAL FINDINGS
Physical examination findings are as follows:
Often, a defect can be palpated in the patella.
New onset of joint effusion after injury localizes within the capsule of the knee. A knee effusion may not be present if there is disruption of the retinaculum, allowing hematoma to escape from the joint capsule. A significant effusion can increase tension on the limited soft tissue envelope resulting in necrosis of the skin.
The position of the patella (baja vs. alta) and palpation of defects with the patella, quadriceps tendon, or patellar tendon can help differentiate between patellar fracture and ligamentous extensor disruption.
Pain can limit the ability to test for active extension of the knee or for extensor lag. Introduction of local anesthesia after aspiration of hematoma can aid in assessment of extensor function. The surgeon should note any extravasation of local anesthetic to evaluate intra-articular extension of skin defects.
Aspiration: The surgeon notes the amount of fluid aspirated. The presence of fat lobules in the syringe signifies a fracture extending into the knee capsule.
Patients with patellar fractures are able to actively extend the knee in marginal or longitudinal fracture types or with intact secondary extensors (ie, retinaculum). Knee extension is usually not possible with displaced transverse fractures.
History is critical in determining a direct versus indirect cause of fracture. Patellar fractures caused by a high-energy direct cause (ie, head-on motor vehicle accident with dashboard injury) are often associated with other injuries to the knee.
Peripheral pulses and neurologic function must be examined.
Knee stability should be evaluated. Patellar fractures may be accompanied by cruciate ligament injury or associated knee dislocation.
Open fractures will require urgent operative management and are associated with an increased rate of nonunion and infection.19 Open fractures also connote higher energy and an increased likelihood of associated injury.
Physical examination must include a thorough secondary survey for other associated injuries. Distal femur fractures and acetabular injuries are commonly associated in highenergy motor vehicle accidents owing to transfer of force through the flexed knee (eg, dashboard injury).
IMAGING AND OTHER DIAGNOSTIC STUDIES
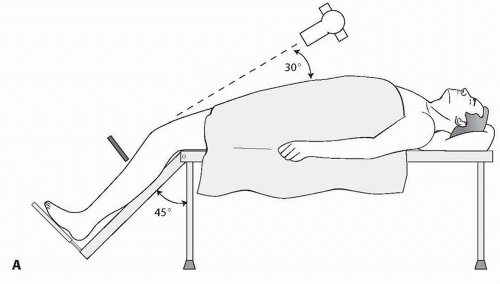
Anteroposterior (AP) and lateral views of the knee and an axial view of the patella provide sufficient information for nearly all fracture types.
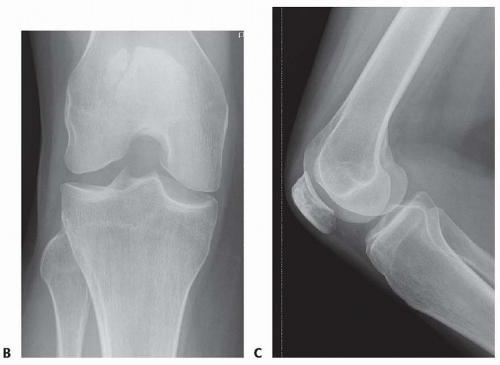
A bipartite patella, arising from failed fusion of patellar ossification centers, can be mistaken for a fracture. Bipartite patellae are most commonly located superolaterally and occur more frequently in males. In 40% of individuals with a bipartite patella, the contralateral patella will also be bipartite7 (FIG 2B,C).
The normal Insall-Salvati ratio (height of the patella over the distance from the inferior pole to the tibial tubercle) is about8 1.0.
DIFFERENTIAL DIAGNOSIS
Quadriceps rupture
Patellar tendon rupture
Bipartite patella
Ligamentous or meniscal injury
Distal femur or tibial plateau fracture
Inflammatory arthritis or septic arthritis
Osteochondral injury
Patellar dislocation or retinacular injury
Severe hemarthrosis
NONOPERATIVE MANAGEMENT
Fractures must meet two criteria to be managed nonoperatively:
No associated extensor mechanism disruption (ability to perform an active straight-leg raise without significant lag)
The described period of immobilization varies. Historically, patients were kept in a long-leg or cylinder cast for 4 to 6 weeks. Current nonoperative management involves early functional treatment.
Our preference for nonoperative treatment includes full weight bearing with crutches and a hinged knee brace.
The leg is maintained in extension for 3 weeks, 0 to 30 degrees of flexion for 3 weeks, followed by full motion with physiotherapy as needed.
High-impact activity including contact sports is allowed at 12 weeks.
SURGICAL MANAGEMENT
Operative treatment is the preferred treatment for the majority of fractures not meeting the nonoperative criteria outlined earlier. Treatment is aimed at anatomic reconstruction of the articular surface and restoration of the extensor mechanism.
Open reduction and internal fixation is the treatment of choice.
Cases with severe comminution of the inferior or superior pole may be considered for partial patellectomy with reapproximation of the patellar tendon.
Functional deficits without a patella are significant, therefore a total patellectomy should only be reserved for the most severe cases where reconstruction is not possible.
Methods involving arthroscopy or external fixation have not gained widespread use.
Soft tissue management is essential due to the limited soft tissue envelope covering the patella. This care for soft tissue begins in the emergency department. Splints or knee immobilizers must be accompanied by copious padding to minimize complications from pressure. Similarly, early aspiration of the hemarthrosis can prevent pressure necrosis.
Preoperative Planning
Operative timing is dictated by patient condition, presence of open fractures, and condition of the soft tissues.
Fracture imaging is reviewed.
Necessary equipment for surgical stabilization should be available.
Examination under anesthesia is critical, as evaluation of coexisting ligamentous injuries is often limited by patient pain prior to surgery. Lachman, pivot shift, posterior drawer, and varus-valgus testing should be undertaken before preparing the surgical site.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree