Open Reduction and Internal Fixation of Jones Fractures
Scott J. Koenig
Steven D. K. Ross
DEFINITION
A Jones fracture represents an acute injury at the metaphyseal-diaphyseal junction of the fifth metatarsal (FIG 1).
The fracture begins on the lateral aspect of the fifth metatarsal and propagates into the articulation between the fourth and fifth metatarsals.
There is no extension distal to the fourth and fifth intermetatarsal articulation.
ANATOMY
Stability of the proximal fifth metatarsal is provided by the lateral Lisfranc complex, capsular ligaments, lateral band of the plantar aponeurosis, and the peroneus brevis.19
There are two major motor insertions onto the fifth metatarsal:
The peroneus brevis inserts onto the dorsal aspect of the fifth metatarsal tubercle.
The peroneus tertius inserts onto the dorsal aspect of the metatarsal at the proximal metaphyseal-diaphyseal junction.
The plantar fascia has a strong insertion along the plantar aspect of the fifth metatarsal tubercle.
The proximal metaphyseal-diaphyseal junction represents a watershed vascular supply.
PATHOGENESIS
Acute Jones fractures are the result of an adduction force applied to the forefoot while the ankle is in plantar flexion.
Tensile forces along the lateral border of the metatarsal result in a transverse fracture.
They are typically the result of athletic events, with many instances described in football and basketball players.
This should not be confused with a tuberosity avulsion or diaphyseal stress fracture.
Fracture occurs in the area between the peroneus brevis and tertius tendons2 and propagates to the fourth-fifth metatarsal articulation.
This fracture is often associated with patients that have a varus foot posture.
NATURAL HISTORY
The Jones fracture was originally described in 1902 by Sir Robert Jones, who described a series of transverse fractures at the metaphyseal-diaphyseal junction in four individuals, including his own injury.9
The natural history and outcomes of nonoperative and operative treatment are difficult to determine because many published reports include a mixture of acute Jones fractures and diaphyseal stress fractures.
Various studies have examined nonoperative versus operative treatment.
There is an increased risk of delayed or nonunion due to the watershed blood supply at the metaphyseal-diaphyseal junction.
Operative treatments have included internal fixation with or without bone grafting and bone grafting alone. Various fixation techniques have been examined.
Treatment options vary based on the functional demands of the patient.
Operative fixation is typically reserved for elite athletes or delayed unions and established nonunions in nonathletes.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient may describe participation in an athletic event where, after a particular maneuver, there is an acute onset of pain over the lateral border of the foot.
The patient may have swelling and ecchymosis over the lateral border of the foot.
Pain will be elicited with direct palpation over the base of the fifth metatarsal.
Physical examination should include the following:
Direct palpation over the base of the fifth metatarsal: Pain in this region increases suspicion of injury.
Direct palpation over the tarsometatarsal joint complex: Pain indicates possible injury to the Lisfranc complex.
Passive dorsiflexion-plantarflexion of individual metatarsal heads: Pain indicates possible injury to the Lisfranc complex.
Attempted single-limb heel lift: Pain indicates possible injury to the Lisfranc complex.
Examination of the lateral ankle ligamentous complex for instability.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs of the affected foot, including anteroposterior, lateral, and oblique views, are sufficient to diagnose an acute Jones fracture.
Location of fracture is used to distinguish between tuberosity avulsions, Jones fractures, and diaphyseal stress fracture.
Sclerotic changes delineate between acute injury and chronic stress injury.
Weight-bearing radiographs of the affected foot are obtained to rule out a Lisfranc injury.
Computed tomography (CT) and magnetic resonance (MR) imaging are typically unnecessary.
DIFFERENTIAL DIAGNOSIS
Must differentiate from other types of proximal fifth metatarsal fractures
Tuberosity avulsion fractures
Can be extra-articular or extend in to the cuboid-metatarsal joint.
Initially thought to be due to avulsion of the peroneus brevis, but Richli et al16 elucidated that avulsion by the lateral band of the plantar aponeurosis was the likely mechanism.
May be mistaken for os peroneum or os vesalianum13
Same mechanism may produce lateral ankle ligamentous injury.
Fracture is stable and may be treated symptomatically due to the attachment of plantar aponeurosis.
Diaphyseal stress fracture
Secondary to repetitive tensile forces causing microfractures of the lateral cortex
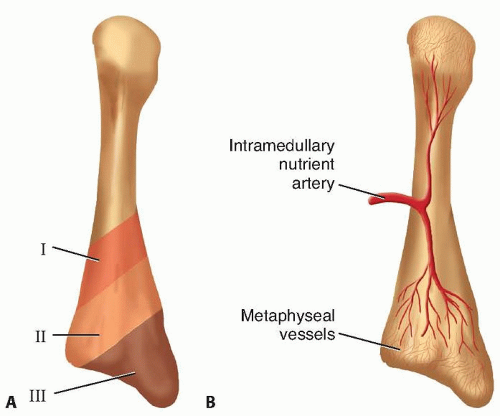
FIG 2 • A. The three anatomic and clinical zones for fractures of the proximal fifth metatarsal. B. Arterial blood supply of the fifth metatarsal.
Typically occur in the proximal 1.5 cm of the diaphysis.
Prodromal symptoms are common.
Radiographs show periosteal reaction, cortical hypertrophy, and narrowing of the medullary canal.
Type 1: Acute fracture where the fracture line has sharp margins and no intramedullary sclerosis. Often involves only the lateral cortex.
Type 2: Delayed union where fracture line involves both cortices with associated periosteal bone formation, widening of the fracture line, and evidence of intramedullary sclerosis.
Type 3: Nonunion demonstrated by bone resorption with radiolucency at the fracture line and obliteration of the medullary canal by sclerotic bone.
Treatment consists of prolonged immobilization and non-weight bearing. Even with treatment, nonunion is a common result and may require fixation.
Lisfranc sprain or subluxation
Cuboid fracture
Lateral ankle ligamentous injury
Peroneal tendon subluxation/rupture
NONOPERATIVE MANAGEMENT
Nonoperative management is preferred treatment for all patients other than elite athletes.
Non-weight bearing in a short-leg cast for 6 to 8 weeks, followed by weight bearing in a walker boot for an additional 6 weeks17
Non-weight bearing compliance is critical for healing.17
Torg et al’s24 series of 15 patients demonstrated a 93% union rate at an average of 6.5 weeks.
Clapper1 reported union in 72% of acute Jones fractures treated with a non-weight-bearing short-leg cast for 8 weeks followed by weight bearing in a cast or walker boot.
Time to union reported as long as 21.2 weeks.1
SURGICAL MANAGEMENT
Nonoperative treatment remains treatment of choice for acute Jones fractures.
The indications for surgical fixation of an acute Jones fractures have not been clearly defined.
Surgery has been advocated for elite athletes, patients with fracture displacement, and in cases of delayed union or established nonunions.
Earlier studies have reported prolonged healing in athletes treated nonsurgically, but these reports have been questioned for both patient compliance and the presence of an alternative fracture mechanism, such as axial load or stress fracture.3, 10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










