Fixation of Periprosthetic Fractures About/Below Total Hip Arthroplasty
Aaron Nauth
Iain Stevenson
Matthew D. Smith
Emil H. Schemitsch
DEFINITION
Periprosthetic fractures about a total hip arthroplasty are fractures which occur in the femur or acetabulum adjacent to either the femoral or acetabular component, respectively. These fractures can occur intraoperatively or postoperatively. The focus of this chapter will be postoperative fractures of the femur which occur adjacent to the femoral component of a total hip arthroplasty.
ANATOMY
Fractures of the femur adjacent to the femoral component of a total hip arthroplasty are most commonly described using the Vancouver classification system which categorizes the fracture on the basis of anatomic location, stability of the femoral component, and surrounding bone stock (Table 1; FIG 1).5 This classification system is simple, reliable, and serves to guide treatment.
Type A fractures occur in the trochanteric region and involve either the greater trochanter (AG) or the lesser trochanter (AL).
Type B fractures occur around or just distal to the stem of the femoral component and are subclassified based on the stability of the implant and the surrounding bone stock. Type B1 fractures occur around a stable implant. Type B2 fractures occur around a loose implant with adequate bone stock. Type B3 fractures occur around a loose implant with poor bone stock.
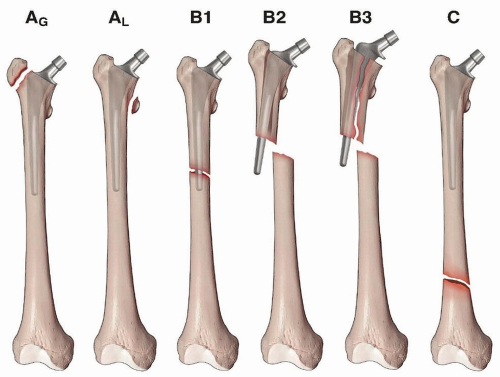
FIG 1 • The Vancouver classification of periprosthetic fractures of the femur about a total hip arthroplasty.
Type C fractures occur well distal to a stable femoral component.
Table 1 Vancouver Classification of Periprosthetic Fractures of the Femur about a Total Hip Arthroplasty | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
PATHOGENESIS
Postoperative periprosthetic fractures can occur in a variety of settings; however, major trauma accounts for a very small proportion.
The majority of these fractures occur with a low-energy fall and up to 25% occur without any significant trauma.
A large proportion of these patients have pathologic and osteopenic bone due to a combination of factors including localized osteopenia of the proximal femur due to stress shielding and osteolysis as well as a high prevalence of osteoporosis in this patient population.
NATURAL HISTORY
The vast majority of these fractures require surgical management for effective fracture healing and return of function.
Retrospective literature has demonstrated a 1-year mortality of 11% and morbidity/mortality very similar to hip fracture patients.1 This is an important consideration as these patients should be managed in a similar fashion to hip fracture patients by incorporating a multidisciplinary team approach (geriatrics assessment, delirium prevention etc.), carrying out early surgical intervention (<48 hours from injury), and using a surgical strategy that allows early weight bearing and mobilization.
PATIENT HISTORY AND PHYSICAL FINDINGS
It is important to obtain information regarding the mechanism of injury and level of energy imparted as well as the cause of the fall.
Information regarding prodromal symptoms such as thigh pain with weight-bearing or start-up pain should be obtained and may indicate a preexisting loose femoral stem prior to fracture.
A history of past infections, wound healing complications, or constitutional symptoms may indicate a periprosthetic infection.
A social history including the patient’s prior ambulatory status, use of walking aids, level of independence, and overall functionality is helpful for setting reasonable treatment goals.
Physical examination may indicate gross deformity of the limb in a displaced fracture or the findings may be more subtle in minimally displaced fractures such as pain with range of motion or rotation of the hip, difficulty weight bearing, or weakness of the limb. Physical examination should also focus on ruling out open wounds, neurovascular injury, and associated injuries.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Investigation begins with anteroposterior (AP) and lateral radiographs of the affected femur and an AP pelvis. Radiographs should be carefully inspected for the location of fracture lines, fragment displacement, implant loosening, and quality of bone stock.
It is critical to identify any evidence of implant loosening as the surgical management of a periprosthetic fracture with a loose femoral component (Vancouver type B2) requires revision to a long-stem component in addition to fracture fixation, whereas a fracture with a stable component (Vancouver type B1) can be readily treated with fracture fixation alone. Lindahl et al4 reported that the most common reason for treatment failure in the fixation of Vancouver type B1 fractures was loosening of the implant, presumably due to failure to recognize that the implant was loose at the time of fracture.
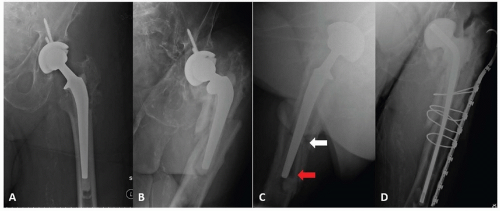
Definite signs of radiographic loosening include progressive periprosthetic or cement mantle lucency, change in position of the stem, and component or cement mantle fracture (FIG 2). Radiographic signs of probable loosening include
greater than 2 mm of periprosthetic or cement mantle lucency, bead shedding, endosteal scalloping, and endosteal bone bridging at the tip of the stem.
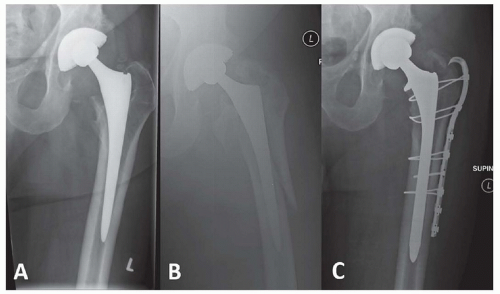
Whenever possible, preinjury radiographs should be obtained to assess for change in component position, as this is the best indication of a loose stem. Careful comparison of implant position on injury and preinjury radiographs is required, as the findings of implant subsidence can range from noticeable to relatively subtle (FIGS 3 and 4).
Efforts should be made to obtain original operative reports in case revision of the implant is required.
Inflammatory markers such as white cell count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are often elevated in the setting of trauma, and therefore can be difficult to interpret in the setting of a fracture unless they are significantly elevated. If concern for infection exists on the basis of preinjury symptoms, a preoperative hip aspiration can be obtained or the surgeon should be prepared to proceed with a two-stage revision should infection be encountered at the time of surgery (see FIG 2).
DIFFERENTIAL DIAGNOSIS
Periprosthetic infection
Aseptic loosening
Pathologic fracture
NONOPERATIVE MANAGEMENT
Operative intervention is indicated for the vast majority of periprosthetic fractures of the femur with the exception of stable fractures of the lesser trochanter without shaft extension, minimally displaced fractures of the greater trochanter, and completely undisplaced fractures around the stem of a stable implant. In addition, minimally displaced fractures about the femoral stem in patients who are poor surgical candidates can be considered for a trial of conservative management.
SURGICAL MANAGEMENT
The surgical management of periprosthetic femur fractures about a total hip arthroplasty is guided by the Vancouver classification.
Type AL fractures of the lesser trochanter are generally managed nonsurgically as are minimally displaced type AG fractures of the greater trochanter. Displaced type AG fractures are generally managed with open reduction and internal fixation (ORIF) +/- bone grafting and polyethylene liner exchange if they are associated with osteolysis and liner wear.
Type B1 fractures have a stable implant and are managed with fracture fixation. The focus of this techniques chapter is on the fixation of these fracture types and techniques for type B1 fracture fixation are described below in detail. There is relative controversy in the literature regarding the optimal technique for fixation of Vancouver type B1 fractures, with the main controversy centered around the use of cable plating combined with allograft strut versus isolated lateral locked plating. The biomechanical literature suggests that the use of a lateral cable plate and screws combined with the use of an anterior allograft strut (90-90 fixation) is the optimal biomechanical construct.7 Buttaro et al2 retrospectively reviewed a 14 patient series of type B1 fractures treated with lateral locked plating +/- the use of a cortical strut. The authors reported a high rate of failure when isolated lateral locked plating was used (five of nine constructs) versus when lateral plating was combined with the use of a cortical strut (one of five constructs). In contrast, other authors have reported a very high rate of success when isolated lateral plating is combined with indirect reduction and biologically friendly techniques.6 High-level prospective evidence comparing the
two techniques is lacking. Irrespective of the fixation strategy used, several biomechanical and surgical principles must be adhered to when treating these fractures. First, it is critical that the fracture is fixed without the stem in varus, as increased rates of fixation failure have been reported with varus positioning of the stem. Second, proximal fixation around the stem is best achieved with a combination of wires/cables and screws, and it is critical that sufficient overlap of the femoral prosthesis is obtained to avoid mechanical failure (FIG 5). This generally requires fixation to the level of the greater trochanter. Third, it is important to remember that these fractures commonly occur in pathologic/osteopenic bone, and the use of a plate of sufficient length to stabilize the entire length of the femur is recommended to avoid future peri-implant fracture. Finally, it is important to adhere to the principles of absolute versus relative stability depending on the type of fracture healing desired. In the setting of a simple transverse or spiral fracture, absolute stability and compression at the fracture site should be achieved using compression plating or lag screw fixation. This is in contrast to comminuted fractures which require relative stability and spaced fixation to allow for fracture healing indirectly by callus formation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree